Obstruction of the Small Intestine in the Abdomen without Surgery: Presentation of 5 Cases
A B S T R A C T
Introduction: The majority of SBOs develop secondary to postoperative adhesions, however nonsurgical etiologies must also be considered. Patients with no surgical history can develop SBO secondary to hernias, radiation, and other miscellaneous causes.
Materials and Methods: Five cases of intestinal occlusion in a patient without previous abdominal surgery are presented.
Discussion: Small bowel obstruction has been recognized as a life-threatening disease process. Stable patients should undergo conservative treatment and progress to surgical intervention only after failure of conservative treatment.
Conclusion: Intestinal occlusion in patients without previous surgeries is a challenge for the Surgeon.
Keywords
Abdominal pain, Abdomen, acute, gallstones, bezoars, hernia, abdominal, enteritis
Introduction
Small bowel obstruction (SBO), has been recognized as a potentially mortal disease process [1]. United States, SBO is responsible for 12%-16% of all surgical admissions, accounting for more than 300,000 annual operations,7-10 and more than $2 billion per year in healthcare expenditures, up from $1.3 billion in 1994 [2-5]. Between 20% and 30% of patients with SBO will undergo operative intervention. In addition to the cost of hospital admissions and potential operative interventions, additional expenses can be incurred for patients requiring parenteral nutrition, intensive care unit stay, and management of complications [6].
The majority of SBOs develop secondary to postoperative adhesions, however nonsurgical etiologies must also be considered. Patients with no surgical history can develop SBO secondary to hernias, radiation, and other miscellaneous causes.
Materials and Methods
Five cases of intestinal occlusion in a patient without previous abdominal surgery are presented. Four of them received surgical treatment and one was managed with conservative treatment.
Case Presentation
Case No. 1: Gallstone Ileus
Gallstone ileus is defined as a mechanical intestinal obstruction secondary to the presence of a gallstone. Less than 1% of cases of intestinal obstruction are derived from this etiology. The most frequent cause is the impaction of the stone in the ileum, after passing through a bilioenteric fistula. It is a rare and potentially serious complication of cholelithiasis. This pathology occurs more in the elderly, the average age at which it occurs is between 60 and 84 years, mainly affecting the female sex, attributed to the higher frequency of biliary pathology in said sex. It presents a high morbidity and mortality, mainly due to the difficulty and the diagnostic delay [7].
Figure 1: Direct abdominal X-ray, showing dilation of the loops of the small intestine in a stack of coins (white arrow) and air-fluid levels (black arrow).
i Description of Case
A 66-year-old female patient, with a pathological history of known cholelithiasis of five years' evolution, denies a surgical history. He was admitted to the central guard (CG) reporting continuous abdominal pain in the epigastric region, of four days of evolution, of increasing intensity, without irradiation, or response to antispasmodics, accompanied by porraceous vomiting of one day of evolution, constipation of four days of evolution. A direct abdominal X-ray was performed, where dilation of the small bowel loops associated with air-fluid levels was visualized (Figure 1).Computed tomography (CT) of the abdomen and pelvis with intravenous contrast is requested (Figure 2).
Figure 2: Double contrast abdominal CT axial slice of cholecysto-duodenal fistula (black arrow).
ii Treatment
An exploratory laparotomy, enterotomy three centimeters cephalad to the stone, and double-layer enterorrhaphy with absorbable suture were performed.
Case No. 2: Bezoar
Small bowel obstruction secondary to bezoar impaction is considerably uncommon, with a reported frequency of about 0.4% to 4% [1]. The incidence of bezoar as a cause of intestinal obstruction is low. The complementary method with the highest sensitivity and specificity continues to be CT of the abdomen and pelvis with oral and intravenous contrast. Treatment must be surgical. Modifying the diet along with managing the disorders is the best form of prevention [8].
i Description of Case
A 65-year-old woman with no surgical history, with a pathological history of hypothyroidism, consumption of 80mg/day of proton pump inhibitors secondary to acute gastritis. A central guard was presented due to vomiting of 48 hours of evolution.
Direct anamnesis: Patient refers to copious intake of dehydrated fruits 72 hours prior to consultation. He reports having started with food-like vomiting at the beginning, which after hours turned into fecaloid, which was accompanied by colic-type abdominal pain at the beginning and then became continuous.
It was decided to perform computed tomography (CT) with oral and intravenous contrast of the abdomen and pelvis, which revealed multiple dilated loops of the small intestine with a transition point within the right lower quadrant where endoluminal content is evident (Figures 3 & 4).
Figure 3: Axial CT with oral and intravenous contrast demonstrating dilated bowel loops and a mass with a mottled gas pattern suggestive of a bezoar (red arrow).
Figure 4: Coronal CT of the abdomen and pelvis with oral and intravenous contrast, showing dilated intestinal loops, accompanied by an intraluminal component with a mottled gas appearance (blue arrow).
ii Treatment
An exploratory laparotomy was performed, in which a large dilation of the loops of the small intestine was observed, with obvious signs of stoppage 30cm from the ileocecal valve, without signs of ischaemia, an enterotomy was performed proximal to the site of obstruction, with subsequent extraction of bezoar (Figure 5). Raffia is made longitudinally with vicryl 3/0, double plane.
Figure 5: Bezoar extracted from terminal ileum after enterotomy.
Case No. 3: Spiegel Hernia
Spigelian hernia is a rare hernia of the anterior abdominal wall, often remains undiagnosed due to the fact that 90% of cases are asymptomatic, and its unusual location in the semilunar line, lateral to the rectus muscle. It represents 0.1% of hernias,1 with a peak incidence between 50 and 60 years of age. The most common complication is hernia strangulation causing intestinal obstruction, ischaemia and perforation [9].
i Description of Case
An 86-year-old woman, consulted in the emergency department of the Surgical Guard, due to abdominal pain of 12 h of evolution in the left flank of colicky onset, which was modified to continuous 2 h before the consultation, accompanied by nausea, fecaloid vomiting. Abdominopelvic tomography with oral and intravenous contrast is performed, which shows a defect in the abdominal wall, in the interline of the rectus abdominis muscle and the right abdominal oblique muscle, compatible with a stuck Spigelian hernia (Figure 6).
Figure 6: Axial section of computed tomography, in which the Spigelian line hernial defect is evident.
ii Treatment
An exploratory laparotomy was performed, intraoperative semiology, incarcerated terminal ileum was evidenced, it could not be reduced from the abdominal cavity, being forced to expand the hernia ring, with this gesture reduction was achieved.
Case No. 4: Femoral Hernia
Femoral hernia comprise a small proportion of all inguinal hernias. They are more common in women and have a high rate of incarceration and strangulation, leading to emergency repair [10].
i Description of Case
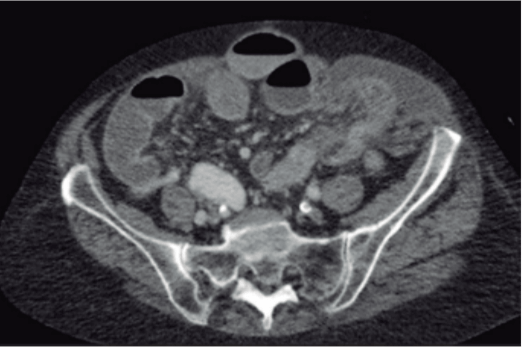
A 61-year-old female patient was admitted to the emergency department with a 2-day history of a painful lump in her left groin that had worsened in the last 24 hours. Physical examination suggested the presence of a strangulated femoral hernia, and the patient underwent emergency surgical repair. Intraoperatively, the right fallopian tube was observed in the hernia sac. Since there were no signs of ischaemia, the tube was reduced back into the pelvic cavity and the hernia was repaired. Abdominal and pelvic CT is performed, in which uncomplicated femoral hernia is confirmed (Figure 7).
Figure 7: Abdominal and pelvic CT scan confirming uncomplicated femoral hernia.
ii Treatment
McVay hernioplasty.
Case No. 5: Actinic Enteritis
Radiation enteritis or actinic enteritis is a complication secondary to the use of radiotherapy to treat pelvic tumors, which can more frequently affect the small intestine. i) Radiotherapy is part of the treatment of various types of neoplasms. ii) Recent reports indicate that up to 70% of cancer patients will receive radiotherapy during the course of their treatment. The deleterious effect of ionizing radiation can affect long after resolution of the primary disease for which it was indicated. In the gastrointestinal tract it can cause damage to the small intestine, known as "radiation enteritis", which can cause intestinal obstruction or blockage of the colon and rectum called "radiation colitis" or "radiation proctopathy" [11].
i Description of Case
An 81-year-old male patient with a history of treatment with RT for prostate carcinoma 15 years ago with a dose of 60 Gray, comes to the emergency department for generalized abdominal pain of 5 days' duration, sudden onset, due to a crisis, of moderate intensity that partially subsides with common analgesics and is accompanied by nausea and vomiting on several occasions of food content initially and later bilious. Feces and gas detention is added to the table 3 days before admission.
Abdominal tomography is also requested, which shows global dilation of the thin loops with a transition zone located between the terminal jejunum and proximal ileum, where parietal thickening is confirmed (Figure 8).
Figure 8: Tomography of the abdomen and pelvis with intravenous contrast, showing dilatation of the thin loops with a transition zone located between the terminal jejunum and proximal ileum.
ii Treatment
Conservative therapy.
Discussion
Small bowel obstruction has been recognized as a life-threatening disease process. Most SBOs develop as a consequence of postoperative adhesions, however, non-surgical etiologies must also be considered. Patients without a surgical history may develop SBO secondary to hernias, radiation, and other miscellaneous causes.
Stable patients should undergo conservative treatment and progress to surgical intervention only after failure of conservative treatment. Other miscellaneous etiologies of SBO should also remain in the differential, including bezoars/foreign bodies, fecal impaction, and parasites, these causes do not usually respond to non-surgical treatment, which is why surgical intervention should not be delayed.
Conclusion
Intestinal occlusion in patients without previous surgeries is a challenge for the Surgeon, who must consider a series of unusual causes as a differential diagnosis, in many cases of surgical resolution and others in which a non-surgical treatment can be performed.
Conflicts of Interest
None.
Funding
None.
Declaration
The work is original. It does not appear in any other scientific journal or media outlet. The journal is not responsible for the content of this article.
Consent
The article was sent with the consent of all the authors for evaluation and publication.
Abbreviation
SBO: Small Bowel Obstruction
CG: Central Guard
CT: Computed Tomography
Article Info
Article Type
Case SeriesPublication history
Received: Thu 03, Nov 2022Accepted: Wed 23, Nov 2022
Published: Thu 08, Dec 2022
Copyright
© 2023 Lucas Garcias. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2022.02.04
Author Info
Corresponding Author
Lucas GarciasService No. 1 of General Surgery, National Clinical Hospital, Córdoba, Argentina
Figures & Tables







References
1.
Lascaratos J,
Marketos S (1999) Intestinal obstruction: a paradigm of earlier influences on
the medicine of late Byzantium. Med Secoli 11: 405-414. [Crossref]
2.
Chiu AS, Jean RA,
Davis KA, Pei KY (2018) Impact of Race on the Surgical Management of Adhesive
Small Bowel Obstruction. J Am Coll Surg 226: 968.e1-976.e1. [Crossref]
3.
Maung AA, Johnson
DC, Piper GL, Barbosa SE, Rowell SE et al. (2012) Evaluation and management of
small-bowel obstruction: an Eastern Association for the Surgery of Trauma
practice management guideline. J Trauma Acute Care Surg 73: S362-S369. [Crossref]
4.
Catena F, Di
Saverio S, Kelly MD, Biffl WL, Ansaloni L et al. (2011) Bologna Guidelines for
Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2010
Evidence-Based Guidelines of the World Society of Emergency Surgery. World J
Emerg Surg 6: 5. [Crossref]
5.
Lee MJ, Sayers AE,
Drake TM, Hollyman M, Bradburn M et al. (2017) UK-based, multisite, prospective
cohort study of small bowel obstruction in acute surgical services: National
Audit of Small Bowel Obstruction (NASBO) protocol. BMJ Open 7: e016796.
[Crossref]
6.
Krielen P, van den
Beukel B, Stommel MWJ, van Goor H, Strik C et al. (2016) In-hospital costs of
an admission for adhesive small bowel obstruction. World J Emerg Surg
11: 49. [Crossref]
7.
Garcias L, Simes S,
Muñoz M, Días I (2022) íleo biliar: Reporte de casos. Prensa Méd Argent
108: 151-156.
8.
Garcias L, Da Rosa
J, Carrizo S (2022) Bezoar: a propósito de un caso. Prensa Méd Argent
108: 247-250.
9.
Garcias L, Alvarez
A, Argüello J (2022) Hernia de Spiegel: a propósito de un caso. Prensa Méd
Argent 108: 293-295.
10. Hachisuka T (2003) Femoral hernia repair. Surg Clin North Am 83: 1189-1205. [Crossref]
11. Sisa C, Godoy R, García LL, Amarilla R (2020) Obstrucción intestinal secundaria a enteritis por radiación. Reporte de caso. An Fac Méd 53: 165-168.
