Nonsurgical Root Canal Treatment of a Mandibular First Premolar with Taurodontism Managed with Minimally Invasive Endodontics: A Case Report
A B S T R A C T
A 67-year-old male patient was referred for further treatment of a mandibular left first premolar. The tooth presented with slight percussion tenderness and the periodontal probing depth was normal. There was no soft tissue swelling. The radiographic image exhibited a temporary restoration in the previously initiated access cavity of the mandibular left first premolar. The diagnosis of the mandibular left first premolar was previously initiated therapy associated with symptomatic apical periodontitis. The tooth presented four root canals and the characteristics of taurodontism. Two buccal root canals bifurcated at the apical third. The pulpal floor was examined under a dental operating microscope and four canal orifices were identified. TruNatomy Glider was used for glide path preparation. TruNatomy Prime file was selected for final root canal preparation in order to maximally preserve the radicular dentin. Root canal irrigation was achieved by using RC-Prep and 2.5% NaOCl between each file application. Canal blockage was avoided by multiple recapitulations with K-files (#10) between changing each rotary file. Obturation of the canals were performed by using TruNatomy Conform Fit® Gutta-Percha cones and AH Plus® root canal sealer via the warm lateral condensation technique. CBCT was arranged for confirmation after root canal treatment of the mandibular left first premolar and showed a good outcome. The clinical procedures and instruments could provide the practitioners for reference while managing such a difficult case.
Keywords
Canal bifurcation, mandibular first premolar, minimally invasive endodontics, nonsurgical root canal treatment, TruNatomy, taurodontism
Aim
To illustrate root canal management of a mandibular first premolar with complex root canal configuration in a Chinese patient using a new single-file rotary system.
Key Learning Points
i. The technologies of Ni-Ti rotary instruments and dental operating microscope are essential tools in the strategy of minimally invasive endodontics.
ii. Mandibular first premolar may exhibit a complex root canal system and even a taurodontism.
Introduction
The strategies for Minimally Invasive Endodontics (MIE) include minimal tissue loss and respect of the original tooth structure [1, 2]. Tooth structure integrity plays an important role in the prognosis of an endodontically treated tooth. Location and amount of tooth structure also determine the modality of restoration and long-term outcome [3]. Thus, MIE aims to preserve as much intact coronal and radicular dentin as possible. The area of so-called pericervical dentin located 4mm above and below the crestal bone was also pointed out to be critical [4, 5]. MIE relates to clinical procedures from diagnosis, treatment planning, and design of root canal treatment to post-restoration [1, 6].
The first step and cornerstone of root canal treatment is the preparation of a suitable access cavity. In traditional endodontic cavities, straight-line access preparation from the cavity to the coronal third of the canal and complete removal of the pulp chamber roof were emphasized. However, both of the concepts appeared to be de-emphasized in contracted endodontic cavities [7]. Protecting the anatomic structures and minimizing the tooth structure loss were proposed. The development of new Nickel-Titanium (Ni-Ti) material, cone beam computed tomography (CBCT) radiographic imaging, dental operating microscopes and ultrasonic instruments are essential tools in proceeding MIE during clinical practice [6].
The root canal configuration of premolars appears to vary widely; indeed, the most complex variations appear to be found in mandibular first premolars [8]. According to the literature review of Cleghorn et al., which contained over 6700 mandibular first premolars, the percentage of different root morphologies were 98% with a single root, 1.8% with two roots, 0.2% with three roots and less than 0.1% with four roots. One canal was discovered in 75.8% of the teeth, while 24.2% of the teeth showed two or more canals. About 21.1% of the teeth presented two or more apical foramina [9]. The possibility of more than one canal was reported even more frequent in ethnic Chinese patients. Walker found 36% and Lu et al. proposed 22% of the mandibular first premolar with two or more than two canals [10, 11]. Circumferential or C-shaped canals were also illustrated in 24% of the cases [11]. The complicated anatomies may lead to increased root canal treatment failure [12, 13]. Thus, root canal treatment of the mandibular first premolar could be challenging.
Taurodontism is characterized by a vertically elongated pulp chamber, apically displaced pulpal floor with bifurcation or trifurcation of the roots [14, 15]. The cause of taurodontism is due to the Hertwig’s epithelial root sheath failure to invaginate at the proper level [14, 16]. The prevalence ranged from 0.1%~48% depending on different diagnostic methodologies and racial predilection [14]. MacDonald-Jankowski and Li reported a relatively higher prevalence of taurodontism in ethnic Chinese females [17]. Most of the taurodontism occurred in permanent mandibular molars [14, 15, 17]. Madeira et al. mentioned the prevalence of taurodontism in mandibular first premolar to be 0.42% based on an in vitro study [18]. A taurodont tooth may also present a variety of root canal configurations which are difficult to manage [14].
The purpose of this case report was to illustrate root canal management of a mandibular first premolar with complex root canal configuration in a Chinese patient. The tooth presented four root canals and the characteristics of taurodontism. Two buccal root canals bifurcated at the apical third. The technologies of Ni-Ti rotary instruments and dental operating microscope were applied combining with the strategy of MIE in this case. CBCT image analysis was also available.
Case Report
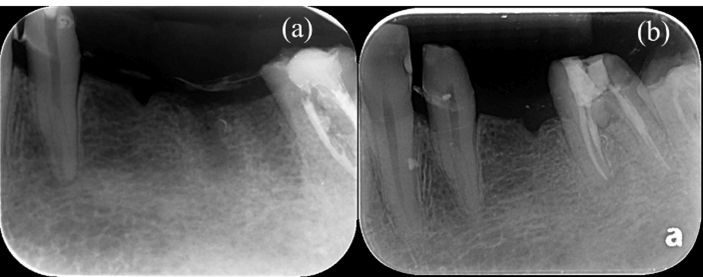
A 67-year-old male patient was referred with a chief complaint of “I felt severe pain in my mandibular left posterior tooth which I had received the emergency treatment recently. The dentist told me that the tooth needed further root canal treatment.” Medical history was non-contributory, and the patient denied any major systemic disease and drug allergies. Clinical examination showed that the mandibular left first premolar had a temporary restoration that was placed 3 weeks ago. The tooth presented with slight percussion tenderness and the periodontal probing depth was normal. There was no soft tissue swelling. The radiographic image exhibited a temporary restoration in the previously initiated access cavity of the mandibular left first premolar. Based on clinical and radiographic findings, the diagnosis of the mandibular left first premolar was previously initiated therapy associated with symptomatic apical periodontitis. An unusual root canal morphology was noted from the initial radiograph. Taurodontism and a complex root canal system in the middle to the apical third of the root were observed (Figures 1a & 1b).
Figure 1: a) Initial intraoral periapical radiograph of mandibular left first premolar with temporary filling material in the previously initiated access cavity. b) Initial intraoral periapical radiograph displayed an unusual canal configuration in the root of mandibular left first premolar.
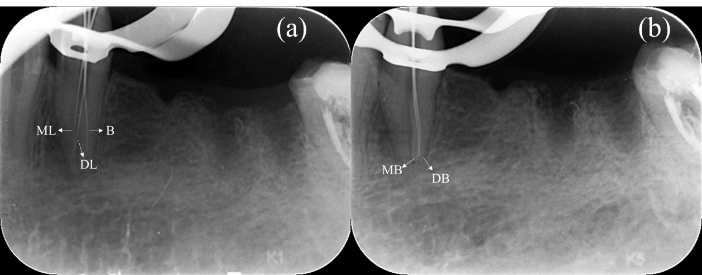
Local infiltration anaesthesia was administered using 2% lidocaine with 1:100,000 adrenaline and followed by dental dam isolation of the mandibular left first premolar. The temporary restoration was removed, and the access cavity preparation was performed with high-speed round burs. The pulp chamber was then irrigated with 2.5% sodium hypochlorite (NaOCl). The pulpal floor was then examined under a dental operating microscope (KAPA Karl Kaps, Asslar, Germany) and probed with an endodontic explorer (Hu-Friedy DG16) to locate the orifices of the buccal (B), mesio-lingual (ML) and disto-lingual (DL) canals. The mesio-buccal (MB) and disto-buccal (DB) canal bifurcated at the apical third. Size #8 and #10 stainless steel K-files (Mani, Tochigi, Japan) were used with 15% ethylenediaminetetraacetic acid (EDTA) root canal preparation paste (RC-Prep; Premier Dental Products, Plymouth Meeting, PA, USA) to establish an initial glide path to the working length (Figures 2a & 2b).
Figure 2: a) Two lingual canals and one buccal canal within the mandibular left first premolar was detected and confirmed via periapical radiograph (White arrows indicated the B, ML and DL canals). b) Two buccal canals within the mandibular left first premolar were further identified and checked by the periapical radiograph (White arrows indicated the MB and DB canals).
The initial negotiation and scouting of the canals were performed with size #8 file (Dentsply Maillefer, Ballaigues, Switzerland) in order to reach the position slightly short from the radiographic apex. Then the file was attached to a reciprocating handpiece (M4 Safety, Kerr, West Collins Orange, CA, USA); 15% EDTA was deposited into the canal and the M4 Safety Handpiece was manipulated back and forth with an amplitude of 1 to 2mm for approximately 10 seconds in each root canal. A larger stainless-steel K-file (.02/#10) was inserted for coronal flaring to reduce the risk of canal blockage. Canal orifices were relocated and opened coronally with the TruNatomy Orifice Modifier before negotiating the root canal to full working length. Working length was subsequently determined by using an electronic apex locator (ProPex Pixi Apex Locator; Dentsply Maillefer). A reproducible glide path was established in all four root canals using size #08 and #10 K-Files (Dentsply Maillefer) before using the TruNatomy Glider.
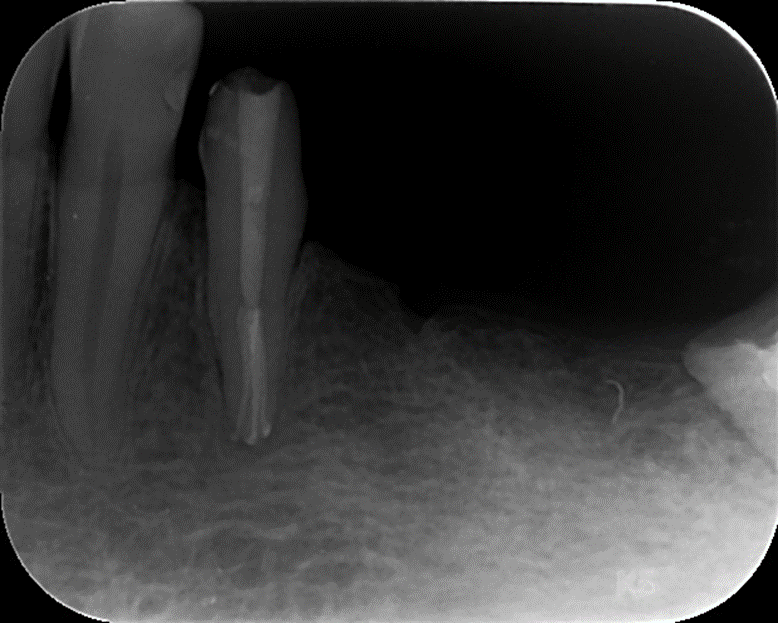
Taking into account that there were four canals within a single root, the TruNatomy Prime file was selected for final root canal preparation in order to maximally preserve the radicular dentin. Root canal irrigation was achieved by using 15% EDTA root canal preparation cream (RC-Prep; Premier Dental Products, Plymouth Meeting, PA, USA) and 2.5% NaOCl between each file application. Canal blockage was avoided by multiple recapitulations with K-files (#10) between changing each rotary file. The canals were rinsed thoroughly with 15% EDTA solution for 3-5 minutes and dried with size #25 sterile paper points. Obturation of the canals was achieved by using TruNatomy Conform Fit® Gutta-Percha cones and AH Plus® root canal sealer (Dentsply Maillefer) via the warm lateral condensation technique.
Figure 3: Periapical radiograph of mandibular left first premolar after root canal obturation. Note the maximum preservation of the pericervical and radicular dentin.
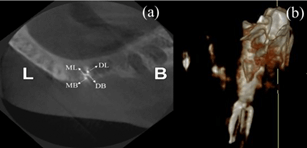
A thin sterilized cotton pellet was placed in the pulp chamber; the access cavity was temporarily sealed with IRM (Dentsply DeTrey, Konstanz, Germany) (Figure 3). CBCT was arranged for confirmation after root canal treatment of the mandibular left first premolar and showed a good outcome (Figures 4a & 4b). The patient was without any symptoms and signs and eventually returned to the previous dentist for the final restoration. The information of the treatment procedure is shown in (Table 1).
Figure 4: a) The axial section of the CBCT image exhibited four main canals of the mandibular left first premolar with a root canal filling material. b) Reconstructed CBCT image of mandibular left first premolar after root canal obturation.
Table 1: Information of the working length, final preparation size, sealer and obturation method.
|
Root canal |
Working length |
Final preparation size |
RCF sealer |
Obturation method |
|
MB |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
ML |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
DB |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
DL |
18.5 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
Discussion
MIE aims to minimize the removal of healthy tooth structure during treatment and thus maintain the dental hard tissue as much as possible. Preserving specifically as much as possible the cervical tooth structure around the canal orifice is important in this strategy [1]. It is recognized that no restorative materials or techniques are capable of replacing the pericervical dentin, which provides resistance to tooth fracture [7]. Removing the pericervical tooth structure is irreversible and caution should be taken while proceeding with root canal treatment. New Ni-Ti materials, advanced imaging system and microscopic magnification are beneficial in performing MIE.
Tooth integrity is crucial in determining the outcome of an endodontically treated tooth [19]. The fracture resistance of an endodontically treated tooth has been shown to be directly related to the amount of the tooth structure preserved. Some researchers had advocated the cervical dentin was more important than the occlusal structure in maintaining a tooth’s longevity and ideal function [4, 20]. In the presented case, the access cavity of the mandibular left first premolar had been prepared by the initial treatment provider. No further enlargement of the access cavity was designed. Under magnification of the microscope, tooth structure and pericervical dentin were preserved as much as possible. The coronal preparation was carried out with the TruNatomy Orifice Modifier instead of using traditional Gates Glidden drills in order to maintain the dentin around the orifices.
Apical preparation size between #20~#40 was proposed to be desirable for preserving radicular dentin [1]. Some clinicians supported larger apical preparation to potentially achieve better shaping and disinfecting of the root canal [21-23]. Others suggested minimal preparation of the root canal to avoid the weakening of the radicular dentin and overfilling of the root canal obturation material. Smaller apical preparation also created a tight apical seal and a more conservative strategy [24, 25]. It appears that there is no singular ideal apical preparation size because it may be related to a variety of considerations. A minimally tapered rotary instrument should not have a taper larger than .06 [1]. Based on the ex vivo investigation of Sabeti et al., they designed three groups (.04 taper, .06 taper and .08 taper) for assessment of the fracture resistance of endodontically treated teeth. The groups with .04 and .06 taper both showed significantly higher fracture resistance when compared with .08 taper group. Thus, the authors concluded that increasing the taper of the root canal during instrumentation could decrease the fracture resistance [26].
The study of Zandbiglari et al., confirmed that larger taper instruments would significantly weaken the tooth structure owing to a greater amount of dentin removal [27]. Thus, the apical and tapering preparation of the mandibular left first premolar in this case was relatively conservative. The final preparation size and taper was #26/.04 (TruNatomy Prime file) which fulfilled the criteria of minimal preparation. TruNatomy had also been reported to successfully treat radix entomolaris, S-shaped root canals, teeth with separated instrument and calcific metamorphosis [28].
A taurodont, usually at first glance, looks like a normal tooth as their unique anatomy mainly lies below the alveolar bone. The diagnosis of taurodontism is only confirmed by the radiographic image [14]. The radiographic features include a relatively rectangular pulp chamber extending into the elongated tooth and shortened roots with the bifurcation or trifurcation near the root apex [29]. There was still no consensus about the classification of taurodontism due to the various morphologic changes and different inclusion criteria. Some researchers categorized premolars into groups [30, 31]. However, the others excluded premolars and questioned their existence. According to the study of Shifman & Chanannel (1978), taurodontism was defined based on the ratio of the distance between the chamber roof to floor and the chamber roof to root apex as greater than 0.2. The distance between the pulp chamber floor and cementoenamel junction (CEJ) should show a number greater than 2.5mm. Based on the value, in this case, the ratio was 0.59 and the distance from the pulp chamber floor to CEJ was 7.8mm which met the requirements described for taurodontism. The mandibular first premolar in this study accorded with the above-described criteria and was therefore classified as a taurodont [32].
Based on the classic work by Shaw (1928), the ratio value of this case indicated a hypertaurodont. A hypertaurodont presented the feature of a large pulp chamber which almost reached the root apex and then separated into several pathways [33]. In a research which included 247 male patients, 2.8% of the cases were hypotaurodontism, 0.4% were mesotaurodontism and no hypertaurodontism was noted [34]. Hypertaurodontism was relatively rare and uncommon in tooth anatomy. Most of the hypertaurodontism was discovered in the mandibular third molars [32, 34]. So, the type of the taurodontism in this study was absolutely unique which occurred in a mandibular left premolar that had never been reported.
A taurodont tooth usually presented various types of root canal configurations, different severity of canal obliteration and proximity between the canal orifices. The apically positioned canal orifices or bifurcated near the root apex posed a perplexing condition to the clinicians. A dental operating microscope must be applied in assisting such a complicated clinical situation [14, 15]. The difficulties in managing the root canal treatment of a taurodontism had been addressed in past studies. Due to the irregular and voluminous pulpal space within the taurodont, 2.5% NaOCl was suggested to apply as an irrigant to chemical debridement [35]. Adequate instrumentation and preparation of the whole root canal system were considered very difficult to achieve. Thus, the combination of using NaOCl was suggested to dissolve as much necrotic tissue as possible [14]. In this case, the procedures of the root canal treatment were carried out under the microscope. Not only manual files but also rotary instruments were used to achieve a better mechanical debridement. Continuously flushing the root canals with 2.5% NaOCl irrigant was also performed as a complement.
Based on the categories of root canal configurations proposed by Sert & Bayirli (2004), the canal system of the mandibular first premolar in this study belonged to type XXIII (3-4). Before chemomechanically preparing such a complicated root canal, a glide path should be provided first [36]. Glide path was defined as a smooth route or pathway created from canal orifice to the apical foramen and centered within the original physiological anatomy [37]. The glide path could be created by manual instruments or engine driven small tapered rotary files [36]. A glide path should be prepared until a #15 K-file fits without tightness [38]. The presence of a glide path enables the reduction of frictional forces, torsional stress and threading-in effect of the Ni-Ti rotary instruments [39, 40]. In this case, the glide path preparation was initiated with size #8 and #10 ISO stainless steel K-file used manually. As the tactile sensation of the root canal was confirmed, the files were attached to a reciprocating handpiece (M4 Safety, Kerr, West Collins Orange, CA, USA) and followed by the application of TruNatomy Glider as a rotary file for establishing a definitive glide path.
According to the Endodontic Case Difficulty Assessment Form and Guidelines proposed by the American Association of Endodontists, the mandibular first premolar in this study could be categorized into great difficulty. The challenging criterion, in this case, contained mandibular premolar with more than one root canal, canal bifurcation near the middle or apical third and vague canal pathways.
Conclusion
This case report describes a highly challenging nonsurgical root canal treatment of a mandibular first premolar with four root canals and the feature of taurodont with the use of the TruNatomy system (Dentsply Sirona). The clinical procedures and instruments could provide the practitioners for reference while managing such a difficult case. The concept of minimally invasive endodontics should be investigated with more clinical implications.
Article Info
Article Type
Case ReportPublication history
Received: Fri 09, Oct 2020Accepted: Mon 23, Nov 2020
Published: Fri 04, Dec 2020
Copyright
© 2023 Ling-Chang Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRDOB.2020.01.02
Author Info
Ling-Chang Shen Wan-Chuen Liao O. A. Peters
Corresponding Author
Ling-Chang ShenInstitute of Oral Medicine & Department of Stomatology National Cheng Kung University Hospital, Tainan, Taiwan
Figures & Tables
Table 1: Information of the working length, final preparation size, sealer and obturation method.
|
Root canal |
Working length |
Final preparation size |
RCF sealer |
Obturation method |
|
MB |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
ML |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
DB |
19 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
|
DL |
18.5 mm |
TruNatomy Prime .04/#26 files |
AH Plus® sealer |
TruNatomy Conform Fit® with warm lateral condensation |
References
- Gutmann JL (2013) Minimally invasive dentistry (Endodontics). J Conserv Dent 16: 282-283. [Crossref]
- Nový BB, Fuller CE (2008) The material science of minimally invasive esthetic restorations. Compend Contin Educ Dent 29: 338-347. [Crossref]
- Tang W, Wu Y, Smales RJ (2010) Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod 36: 609-617. [Crossref]
- Clark D, Khademi JA (2010) Case studies in modern molar endodontic access and directed dentin conservation. Dent Clin North Am 54: 275-289. [Crossref]
- Bóveda C, Kishen A (2015) Contracted endodontic cavities: the foundation for less invasive alternatives in the management of apical periodontitis. Endodontic Topics 33: 169-186.
- Yuan K, Niu C, Xie Q, Jiang W, Gao L et al. (2016) Comparative evaluation of the impact of minimally invasive preparation vs. conventional straight-line preparation on tooth biomechanics: a finite element analysis. Eur J Oral Sci 124: 591-596. [Crossref]
- Gluskin AH, Peters CI, Peters OA (2014) Minimally invasive endodontics: challenging prevailing paradigms. Br Dent J 216: 347-353. [Crossref]
- Slowey RR (1979) Root canal anatomy. Road map to successful endodontics. Dent Clin North Am 23: 555-573. [Crossref]
- Cleghorn BM, Christie WH, Dong CCS (2007) The Root and Root Canal Morphology of the Human Mandibular First Premolar: A Literature Review. J Endod 33: 509-516. [Crossref]
- Walker RT (1988) Root canal anatomy of mandibular first premolars in a southern Chinese population. Endod Dent Traumatol 4: 226-228. [Crossref]
- Lu TY, Yang SF, Pai SF (2006) Complicated Root Canal Morphology of Mandibular First Premolar in a Chinese Population Using the Cross Section Method. J Endod 32: 932-936. [Crossref]
- Baisden MK, Kulild JC, Weller RN (1992) Root canal configuration of the mandibular first premolar. J Endod 18: 505-508. [Crossref]
- England MC, Hartwell GR, Lance JR (1991) Detection and treatment of multiple canals in mandibular premolars. J Endod 17: 174-178. [Crossref]
- Jafarzadeh H, Azarpazhooh A, Mayhall JT (2008) Taurodontism: a review of the condition and endodontic treatment challenges. Int Endod J 41: 375-388. [Crossref]
- Rao A, Arathi R (2006) Taurodontism of deciduous and permanent molars: Report of two cases. J Indian Soc Pedod Prev Dent 24: 42-44. [Crossref]
- Hamner JE, Witkop CJ, Metro PS (1964) Taurodontism: Report of a case. Oral Surg Oral Med Oral Pathol 18: 409-418. [Crossref]
- Macdonald Jankowski DS, Li TT (1993) Taurodontism in a young adult Chinese population. Dento Maxillofac Radiol 22: 140. [Crossref]
- Madeira MC, Leite HF, Niccoli Filho WD, Simões S (1986) Prevalence of taurodontism in premolars. Oral Surg Oral Med Oral Pathol 61: 158-162. [Crossref]
- Nagasiri R, Chitmongkolsuk S (2005) Long-term survival of endodontically treated molars without crown coverage: A retrospective cohort study. J Prosthet Dent 93: 164-170. [Crossref]
- Pierrisnard L, Bohin F, Renault P, Barquins M (2002) Corono-radicular reconstruction of pulpless teeth: a mechanical study using finite element analysis. J Prosthet Dent 88: 442-448. [Crossref]
- Weiger R, Bartha T, Kalwitzki M, Lost C (2006) A clinical method to determine the optimal apical preparation size. Part I. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102: 686-691. [Crossref]
- Shuping GB, Orstavik D, Sigurdsson A, Trope M (2000) Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod 26: 751-755. [Crossref]
- Siqueira JF Jr, Lima KC, Magalhaes FA, Lopes HP, de Uzeda M (1999) Mechanical reduction of the bacterial population in the root canal by three instrumentation techniques. J Endod 25: 332-335. [Crossref]
- Buchanan LS (2000) The standardized-taper root canal preparation--Part 1. Concepts for variably tapered shaping instruments. Int Endod J 33: 516-529. [Crossref]
- Buchanan LS (2001) The standardized-taper root canal preparation--Part 2. GT file selection and safe handpiece-driven file use. Int Endod J 34: 63-71. [Crossref]
- Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A et al. (2018) Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. J Endod 44: 1402-1406. [Crossref]
- Zandbiglari T, Davids H, Schafer E (2006) Influence of instrument taper on the resistance to fracture of endodontically treated roots. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: 126-131. [Crossref]
- van der Vyver PJ, Vorster M, Peters OA (2019) Minimally invasive endodontics using a new single-file rotary system. Int Dent Afr Ed 9: 6-20.
- Terezhalmy GT, Riley CK, Moore WS (2001) Clinical images in oral medicine and maxillofacial radiology. Taurodontism. Quintessence Int 32: 254-255. [Crossref]
- Llamas R, Jimenez Planas A (1993) Taurodontism in premolars. Oral Surg Oral Med Oral Pathol 75: 501-505. [Crossref]
- Tiku A, Damle SG, Nadkarni UM, Kalaskar RR (2003) Hypertaurodontism in molars and premolars: management of two rare cases. J Indian Soc Pedod Prev Dent 21: 131-134. [Crossref]
- Shifman A, Chanannel I (1978) Prevalence of taurodontism found in radiographic dental examination of 1,200 young adult Israeli patients. Community Dent Oral Epidemiol 6: 200-203. [Crossref]
- Shaw JC (1928) Taurodont Teeth in South African Races. J Anat 62: 476-498.1. [Crossref]
- Keene H (1966) A morphologic and biometric study of taurodontism in a contemporary population. Am J Physical Anthropol 25: 208-209.
- Prakash R, Vishnu C, Suma B, Velmurugan N, Kandaswamy D (2005) Endodontic management of taurodontic teeth. Indian J Dent Res 16: 177-181. [Crossref]
- Burklein S, Schafer E (2015) Minimally invasive endodontics. Quintessence Int 46: 119-124. [Crossref]
- Gambarini G, Plotino G, Sannino G, Grande NM, Giansiracusa A et al. (2015) Cyclic fatigue of instruments for endodontic glide path. Odontology 103: 56-60. [Crossref]
- Bolanos OR, Sinai IH, Gonsky MR, Srinivasan R (1988) A comparison of engine and air-driven instrumentation methods with hand instrumentation. J Endod 14: 392-396. [Crossref]
- Hulsmann M, Peters OA, Dummer PMH (2005) Mechanical preparation of root canals: shaping goals, techniques and means. Endodontic Topics 10: 30-76.
- Kirchhoff AL, Chu R, Mello I, Garzon AD, dos Santos M et al. (2015) Glide Path Management with Single- and Multiple-instrument Rotary Systems in Curved Canals: A Micro-Computed Tomographic Study. J Endod 41: 1880-1883. [Crossref]
