Necrosis of Tongue: A Sequela of Complications in Organophosphate Poisoning
A B S T R A C T
Organophosphate compounds are mainly used in the agriculture and domestic pesticides. The widespread availability of these pesticides results in the inadvertent usage leading to the main agent used in suicide attempts in the developing countries. The severity of the poisoning greatly depends on the type of exposure, quantity and the product. They can cause life threatening complications mainly by the respiratory depression leading to coma and death. Early identification and appropriate management enable to reduce the morbidity and mortality. Atropine, oximes, intravenous fluids are administered for the successful management. A detailed medline search of the associated complications, although rare, necrosis of tongue is reported in only one case associated with organophosphate poisoning. The etiological factors were not mentioned in the found literature. In this case report, we discuss the sequela of complications associated with the acute poisoning cases and the role of maxillofacial surgeons in the management.
Keywords
Organophosphate, pesticides, tongue, necrosis, complications
Introduction
Organophosphate (OP) compounds are commonly used in pesticides around the world due to their widespread availability, low cost, and relatively rapid degradation following application [1]. OP poisoning remains the frequent reason for admission to hospitals in developing countries. They may be ingested by the oral, respiratory or transdermal routes [2]. According to the world health organization (WHO) and several reports in the medline literature suggested the use of OP pesticides was responsible for majority of suicides in the developing world [3]. Clinical signs and symptoms of OP poisoning are miosis, bradycardia, bronchoconstriction, muscle fasciculation, cramps, weakness, respiratory depression, seizures and unconsciousness [2, 4]. The most lethal complication is the development of respiratory failure that can cause deep coma or death [5]. This may also be seen due to the aspiration of gastric contents, excessive secretions, neuromuscular involvement, intermediate syndrome, septicemia and adult respiratory distress syndrome [6]. Identification of the respiratory failure, early endotracheal intubation and immediate pharmacological management are required for successful management. Development of delayed or rare complications such as toxic pancreatitis, opsoclonus and lingual myoclonus are reported in the literature [7, 8]. Necrosis of tongue is a rare complication following OP poisoning that is reported in a single case report, although the precise etiology remains unknown [9]. In this case report, we aim to discuss the possible occurrence and management of the necrosis of tongue in a patient of organophosphate poisoning.
Case Report
A 32-year-old male patient was brought to the emergency department of the King Abdulaziz Hospital, Makkah, complaining of generalized weakness, dizziness and repeated vomiting for three days. He used the domestic spray pesticides in home as a pest control measure for 3 days. On clinical examination the vital signs were as follows- temperature 38.6ºC, blood pressure 160/84, pulse 102 bpm, dilated pupils with decreased consciousness. In intraoral examination, there was no evidence of foreign objects and oral complications. The endotracheal intubation was performed to manage the respiratory distress. The pharmacological management included the immediate administration of atropine, pralidoxime and intravenous fluids. Upon satisfactory improvement of the vital signs, extubation was performed on the second day. On the third day, the patient complaints of bleeding, tenderness in the tongue and fetid odor from the mouth.
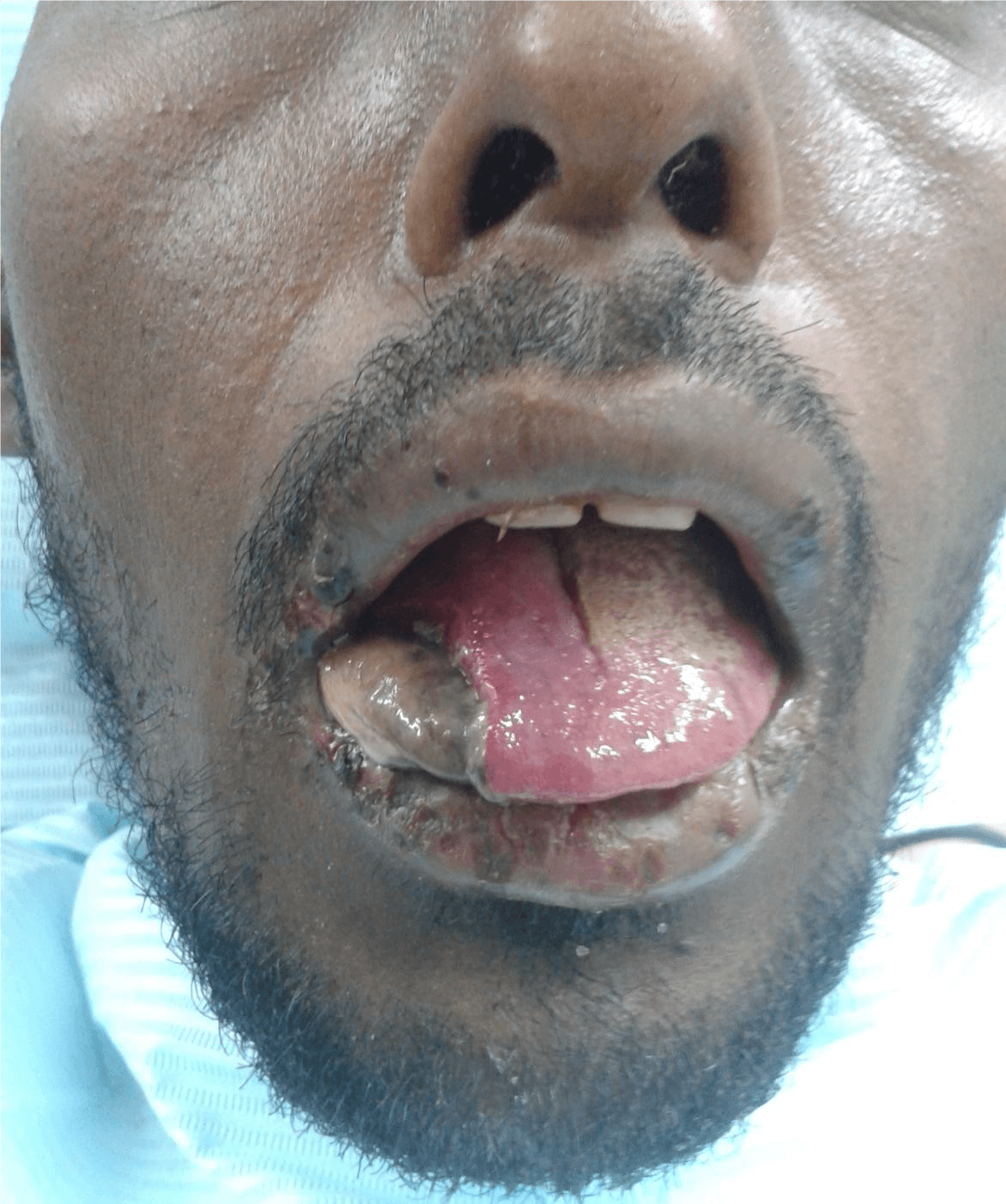
On examination, the right lateral side of the tongue was found discoloured with clear demarcation from the healthy tissues (Figure 1). The necrotic tongue tissue was measuring approximately 8 centimeters long (Figure 2). The debridement of the necrotic tissue was performed under local anaesthesia (Figure 3). The healthy raw area of the tongue was sutured to prevent bleeding (Figure 4). 0.2% chlorhexidine gluconate mouth rinse was used vigorously for 10 days. The exposed raw area was healed without any signs of necrosis. The tongue motility and the sensation on the right side remained unaffected. The patient was discharged on the 10th day since he recovered completely from the effects of OP poisoning and its associated complications. Further, he was advised for a regular follow up after one month to identify the late complications, but the patient failed to attend.
Figure 1: Necrosis of tongue with clear demarcation from the healthy tissue over the dorsum of the tongue.
Figure 2: Lateral view of the Necrosis of tongue with clear demarcation seen over the entire lateral surface of tongue.
Figure 3: Debrided necrotic tissue from the tongue measuring approximately 8 centimeters in length.
Figure 4: Healthy raw tongue tissue margins approximated and sutured using absorbable polyglactin 910 sutures following thorough debridement of necrotic tissue from the lateral border of the tongue.
Discussion
Organophosphate compounds (OPC) are used as major suicidal products that accounts for 40-60% of all poisoning cases in African countries and the Indian subcontinent [2]. The suicidal poisoning rates are higher than accidental exposure while the oral ingestion is the major route of intake. The WHO described the pesticide hazard class (I, II or III) as a graded system that dictates the nature and extent of clinical manifestations and toxicity. While class I is being the most toxic and the least class III [5]. The risk of mortality decreases with prolonged duration of survival [6]. Accidental exposure is the main cause of mild poisoning that can progress to severe forms as seen in our case. OPCs inactivates the acetylcholinesterase enzyme causing accumulation of acetylcholine. This initial overstimulation leads to cessation of cholinergic synaptic transmission at various receptor and ganglionic sites in the body causing nausea, vomiting, blurring of vision, miosis, salivation, diarrhea, urinary incontinence, fever, lacrimation, severe bradycardia, hyperglycemia, hypotension, muscle paralysis, fasciculation, mental confusion, seizures, coma, acute renal failure and respiratory failure [2, 4].
Clinical presentations vary according to the specific agent, quantity and the type of exposure. The mortality is mainly due to acute respiratory depression and renal failure in prolonged cases. Motor and sensory deficits are observed as delayed complications [6]. In this case report, the patient had accidental aerosol exposure of the domestic pesticide leading to the slow onset, mild severity of complications. Hyperglycemia, leukocytosis, impaired liver function tests, high lactate dehydrogenase and increased serum amylase levels were observed in the laboratory investigations [2]. Late complications are commonly encountered following initial or inadequate management. Intermediate syndrome is a late complication also known as a syndrome of muscular paralysis, occurs in 24-96 hours after exposure and resolution of acute cholinergic syndrome [2]. It is characterized by the weakness of the muscles of head and neck, limbs and the respiratory muscles causing ventilatory failure. Although unclear, persistent excess acetylcholine at the neuromuscular junction could be the etiology [10].
The management of OP poisoning is aimed at immediate decontamination, reversal of muscarinic symptoms by atropine, regeneration of acetylcholinesterase using oxime compounds such as pralidoxime, and supportive pulmonary care [4]. The respiratory symptoms consistently develop during the first 24 hours alarming the need for endotracheal intubation [4]. Inadequate atropinization may lead to higher rates of aspiration pneumonia and death [10]. OP poisoning is associated with rare complications such as acute pancreatitis, opsoclonus, lingual myoclonus and necrosis of tongue [7-9]. Circulatory disturbances and necrosis of the tongue are extremely rare because of its rich vascularity. The ischemic lingual necrosis is most often due to temporal arteritis and systemic lupus in elderly women [9]. It is seen as slight discolouration leading to massive necrosis with associated bleeding and fetid odor. Failure to identify the necrotic area can lead to the loss of tongue structure and foul smell.
A clear demarcation of the necrotic tissue in our case was evident on the right side of the tongue. Immediate debridement of the necrotic tissue was performed to prevent its progression. Based on the histopathological changes of the tissue samples exposed to OPC, Sener et al., found OPC may cause muscle fiber degeneration and necrosis. They suggested the careful application of the endotracheal intubation that may jeopardize the clinical condition of the oral structures [9]. Rajasekharan et al., reported the association of opsoclonus and lingual myoclonus in a case of OP poisoning. Lingual myoclonus is the uncontrolled repetitive and rhythmic jerks of the tongue in semiconscious or unconscious patients. It is uncommonly seen in the late complications of the intermediate syndrome following OP exposure management [7]. The precise etiology for the necrosis in this case could not be established. Based on the various reports and our experience the etiology for tongue necrosis could have resulted by the prolonged inadvertent intubation exacerbated by the muscle fiber degeneration and lingual myoclonus making the tongue prone to injury.
Conclusion
OP poisoning is a life threating condition that requires immediate diagnosis and treatment. Early initiation of pharmacological and supportive therapy significantly decreases the mortality rate. This report emphasizes the occurrence of tongue necrosis as a rare complication in organophosphate poisoning. The protection of the oral tissues and identification of the associated complications is an essential aspect in the management. Although rare, failure to identify the necrosis of tongue can cause significant morbidity.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 15, Jun 2020Accepted: Thu 25, Jun 2020
Published: Thu 02, Jul 2020
Copyright
© 2023 Irfan Mohammed. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.04.02
Author Info
Irfan Mohammed Sajid A. Sanadi
Corresponding Author
Irfan MohammedSpecialist Oral & Maxillofacial Surgeon, Department of Oral & Maxillofacial Surgery, King Abdulaziz Hospital, Makkah, Saudi Arabia
Figures & Tables



References
- Singh G, Khurana D (2009) Neurology of acute organophosphate poisoning. Neurol India 57: 119-125. [Crossref]
- Sungur M, Guven M (2001) Intensive care management of organophosphate insecticide poisoning. Crit Care 5: 211-215. [Crossref]
- Kumar MR, Vignan KGP, Babu PR, Kumar SS, Subrahmanyam BV et al. (2014) A retrospective analysis of acute organophosphorus poisoning cases admitted to the tertiary care teaching hospital in South India. Ann Afr Med 13: 71-75. [Crossref]
- Eddleston M, Buckley NA, Eyer P, Dawson AH (2008) Management of acute organophosphorus pesticide poisoning. Lancet 371: 597-607. [Crossref]
- Coskun R, Gundogan K, Sezgin GC, Topaloglu US, Hebbar G et al. (2015) A retrospective review of intensive care management of organophosphate insecticide poisoning: Single center experience. Niger J Clin Pract 18: 644-650. [Crossref]
- Faiz MS, Mughal S, Memon AQ (2011) Acute and Late Complications of Organophosphate Poisoning. J Coll Physicians Surg Pak 21: 288-290. [Crossref]
- Rajasekharan C, Renjith SW, Jayapal T (2012) Opsoclonus and Lingual Myoclonus Due to Organophosphate Poisoning: Images in Clinical Medicine. BMJ Case Rep 2012: bcr2012007043. [Crossref]
- Yoshida S, Okada H, Nakano S, Shirai K, Yuhara T et al. (2015) Much caution does no harm! Organophosphate poisoning often causes pancreatitis. J Intensive Care 3: 21. [Crossref]
- Sener EB, Guneren E (2004) Can Organophosphates Facilitate Acute Tongue Necrosis? Anesth Analg 99: 1871-1882.
- Peter JV, Sudarsan TI, Moran JL (2014) Clinical features of organophosphate poisoning: A review of different classification systems and approaches. Indian J Crit Care Med 18: 735-745. [Crossref]
