Nasopalatine Duct Cyst: A Case Report and Review of Literature
A B S T R A C T
Nasopalatine duct cyst is the most common developmental non-odontogenic cysts seen in the midline region of anterior maxilla. An epithelial remnant of the nasopalatine ducts remain in the incisive canal is the most common etiology. Nasopalatine duct cysts are generally asymptomatic and infrequently produce a swelling and associated pain in the anterior palate if secondarily infected. On radiograph it presents with a well-defined round, oval or heart shaped radiolucency. Histopathologically it shows non-keratinized epithelium typically with neurovascular bundles in the connective tissue capsule. Surgical enucleation is the treatment of choice. In the present case report clinical features, diagnosis and management of nasopalatine duct cyst in a 23-year-old male in the anterior maxillary palatal region is discussed.
Keywords
Jaw cysts, nasopalatine duct cyst, non-odontogenic cysts
Introduction
The nasopalatine duct cyst (NPDC) was described first in 1914 by Meyer. NPDC is also called by other names such as anterior midline cyst, middle palatine cyst, maxillary midline cyst and incisive duct cyst. According to the classification of WHO, it is now regarded as epithelial, developmental, non-odontogenic cysts of the anterior maxilla. NPDC is commonly asymptomatic, but sometimes can produce swelling [1, 2]. It comprises about 1.7-11.9% of all oral and maxillofacial region cysts and it is most common non-odontogenic cysts of the oral cavity [3, 4]. NPDC is almost three times more common in males as compared to females [5]. The greatest occurrence is seen between 40 and 60 years of age [6]. This case report deals with clinical features, diagnosis and management of NPDC in a 23-year-old male patient.
Case Report
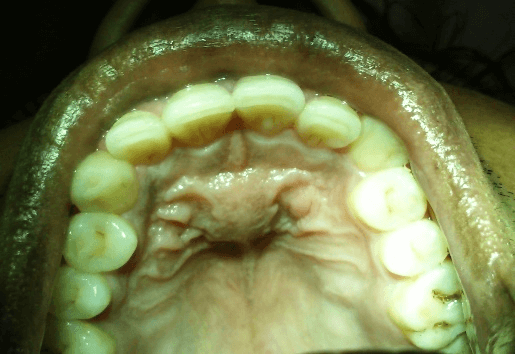
A 23-year-old male patient came to the department of oral pathology and microbiology with a chief complaint of swelling in anterior palatal region since 5-8 months. On clinical examinations, the swelling was present on anterior mid-palatal region of 2.0 x 1.5 cm in size and roughly round to oval in shape. The swelling had well-defined borders, smooth surface and normal pinkish in colour (Figure 1). The swelling was asymptomatic. The swelling was non-compressible, hard in consistency, non-pulsatile and non-reducible. The patient was not any history of trauma or infection. The vitality testing of permanent maxillary central and lateral incisors of left and right side showed that these were vital teeth.
Figure 1: Clinical intraoral picture of the patient showing well defined swelling in the anterior region of the palate.
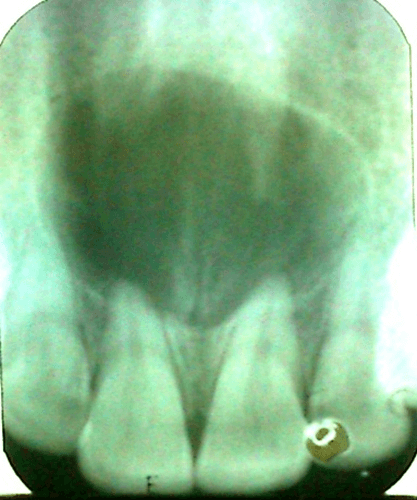
On radiographical examination, the IOPA showed well-defined round to oval unilocular radiolucency at periapical region of right and left permanent maxillary central and lateral incisors. There was divergence of the roots of the central incisors with no resorption (Figure 2). On the basis of clinical and radiological examination a provisional diagnosis of nasopalatine duct cyst was made.
Figure 2: IOPA showing round to oval unilocular radiolucency extending from permanent maxillary lateral incisor of right side to the permanent maxillary lateral incisor of left side.
The excisional biopsy with extensive curettage was done under local anaesthesia and sent for the histopathological examination. The gross specimen was of 2.0 x 1.5 x 0.5 cm in size, soft in consistency and roughly oval in shape (Figure 3).
Figure 3: Excisional biopsy specimen.
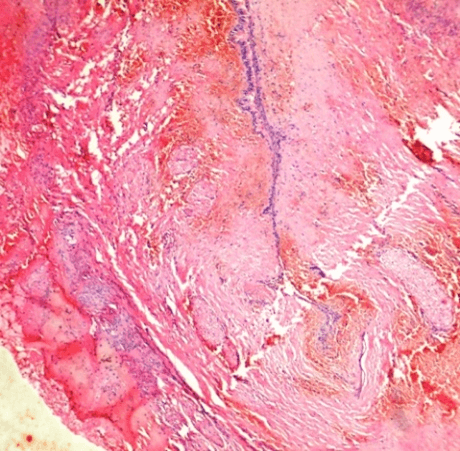
Figure 4: Histopathological picture showing cystic cavity lined by squamous, columnar and at places pseudostratified squamous epithelium. Also note prominently seen nerve bundles in the connective tissue capsule (H and E stain, 40x).
Histopathological examination showed cystic cavity lined by 1-2 layered epithelium with overlying thick fibrous capsule. The cystic lining was single layered lining of squamous cells, columnar cells and at places pseudostratified ciliated columnar epithelium. The connective tissue capsule was fibrocellular with presence of well-defined nerve bundles (Figures 4 & 5). This confirms the diagnosis of nasopalatine duct cyst. After 2 months follow-up the lesional site showed a normal healing.
Figure 5: High power histopathological picture showing pseudostratified squamous epithelium (H and E stain, 100x).
Discussion
NPDC is the most common non-odontogenic cyst and it is unique in that it typically occurring only in a single location within jawbone in the anterior maxillary midline palatal region [1]. NPDCs are generally asymptomatic and mostly discovered on routine radiographs. When occur, the swelling of the anterior palate, drainage and pain is the common presenting symptoms. Rarely a large NPDC produces a “through-and-through” fluctuant expansion of bone involving both the anterior palate and labial mucosa. If it is near the surface, fluctuant swelling with a bluish hue is present. Deeper cysts are usually covered by normal mucosa unless it is ulcerated. Burning sensation and numbness can be present due to pressure on the nasopalatine nerve. Occasionally intermittent discharge with a salty taste seen and displacement of teeth is a rare finding [7]. In the present report the patient was of 23-year-old male patient.
Instead of many studies, the etiology of NPDC is still uncertain. The most common hypothesis is that it develops from the proliferation of the epithelial remnants of the nasopalatine duct [8]. In the anterior maxillary region, the nasopalatine ducts communicates with the nasal cavity [1]. During development, the duct progressively narrows until one or two central clefts are at last produced on the midline of the maxilla. Within the nasopalatine duct the nasopalatine neurovascular bundle is located, and it emerges from through the nasopalatine foramen. As many as 6 different foramina can be present but with only two independent neurovascular bundles (right and left). The nerve and vessel component can emerge separately and the foramina containing completely vascular components are known as Scarpa’s foramina [9].
Progressive degeneration of the nasopalatine ducts generally occurs. However, the epithelial remnants which were persisted may later become the source of epithelia from which NPDC can arise. The proliferation can occur either from spontaneous proliferation or proliferation following trauma (example- removable dentures), bacterial infection or mucous retention [6, 7]. Genetic and racial factors have also been suggested [1, 10]. In the present case there was no history of trauma of infection. Hence, we consider it was of unknown etiology or spontaneous proliferation to be the most plausible explanation. On radiographic features, well defined round, oval or heart-shaped radiolucency can be seen in the midline of anterior maxilla. The heart shape to the lesion can be seen due to nasal septum notching during their expansion or because superimposition of nasal spine on the radiolucent area [4].
In some cases, a prominent incisive canal can be seen as a radiolucent area and mimic NPDC. Most investigators agree that maximum 6 mm should be considered as the upper limit for normal incisive canal radiolucencies and larger than this should consider potentially pathologic and further investigation should be carried out [1]. In this case report, the radiolucency was of round to oval in shape causing divergence of the roots of central incisors.
Histopathologically it shows squamous, columnar, cuboidal, or some combination of these epithelial types and in only 9.8% of cases respiratory epithelium is seen [4]. The presence of different types of epithelia reflects the pluripotential feature of embryonic epithelial remnants. A chronic inflammatory reaction and haemorrhage can be seen in 81% and 71% cases respectively. The important diagnostic feature is the presence of structural elements like peripheral nerves, arteries, veins, mucous glands or adipose tissue in the wall of cyst [10].
In the present case, there was presence of multiple types of epithelia including the respiratory epithelium and also many nerve bundles were present in the connective tissue capsule.
Differential diagnosis: Following differential diagnosis should be considered for NPDC-
i. Odontogenic cysts (e.g. lateral radicular cyst, lateral periodontal cyst, odontogenic keratocyst) [1].
ii. Odontogenic tumors (e.g. ameloblastoma, odontogenic myxoma) [1].
iii. Non-odontogenic tumors (e.g. central giant tumor, brown tumor of hyperparathyroidism, central hemangioma) [1].
A through differential diagnosis should be taken into consideration to avoid needless treatment procedures like root canal treatments in vital permanent maxillary central or lateral incisors. A correct tentative diagnosis can be made on basis of positive dental vitality testing of the nearby teeth provided these teeth do not have other pulp or periodontal problems [1, 2].
The treatment of choice for NPDC is surgical enucleation or in case of larger cysts marsupialization can be done. The highly vascularised structure present near NPDC is the nasopalatine neurovascular bundle which can give rise to profuse bleeding if inadvertently sectioned during surgery. In 10% of cases, the paresthesia of the anterior palatal region is found due to removal of nasopalatine nerve endings along with the membrane of the cyst [4, 10].
Conclusion
NPDC is the most common non-odontogenic cyst of the oral cavity and must be diagnosed properly on the basis of clinical and radiographic examinations. The present case had clinical, radiographic, and histopathological features of a typical NPDC. The importance of this case is in the diagnosis of such lesions which can easily be misinterpreted as radicular cyst and inadvertent endodontic treatment of the nearby teeth can be avoided.
Surgical excision is the treatment of choice and, even with low recurrence rates, postoperative follow-up is imperative for the evaluation and treatment of possible postoperative complications.
Author Contributions
All authors have contributed equally in the treatment, data collection, data analysis or interpretation and writing this paper.
Ethical Approval
None.
Consent
Informed consent was taken.
Competing Interest
None.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Sat 15, Aug 2020Accepted: Wed 23, Sep 2020
Published: Fri 16, Oct 2020
Copyright
© 2023 Kishor Patil. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.02.04
Author Info
Kishor Patil Ashok Patil Suyog Tupsakhare Ketan Saraf Fareedi Mukram Ali
Corresponding Author
Kishor PatilSenior lecturer, Department of Oral Pathology & Microbiology, SMBT Dental College & Hospital, Sangamner, Maharashtra, India
Figures & Tables


References
- Shylaja S, Balaji K, Krishna A (2013) Nasopalatine duct cyst: report of a case with review of literature. Indian J Otolaryngol Head Neck Surg 65: 385-388. [Crossref]
- Allard RH, van der Kwast WA, van der Waal I (1981) Nasopalatine duct cyst: Review of the literature and report of 22 cases. Int J Oral Surg 10: 447-461. [Crossref]
- Oliveira LJ, Leao PLR, Alvareenga RR, Horta MCR, Souza PEA (2017) Nasopalatine duct cyst – diagnosis, treatment and postoperative complications: report of two cases. J Bras Patol Med Lab 53: 407-413.
- Dedhia P, Dedhia S, Dhokar A, Desai A (2013) Nasopalatine duct cyst. Case Rep Dent 2013: 869516. [Crossref]
- Gnanasekhar JD, Walvekar SV, al Kandari AM, al Duwairi Y (1995) Misdiagnosis and mismanagement of a nasopalatine duct cyst and its corrective therapy. A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 80: 465-470. [Crossref]
- Escoda Francolí J, Almendros Marqués N, Berini Aytés L, Gay Escoda C (2008) Nasopalatine duct cyst: Report of 22 cases and review of the literature. Med Oral Patol Oral Cir Bucal 13: E438-E443. [Crossref]
- Aldelaimi TN, Khalil AA (2012) Diagnosis and surgical management of nasopalatine duct cysts. J Craniofac Surg 23: e472-e474. [Crossref]
- Kobashi H, Ishii S, Yakushiji N (2017) Huge nasopalatine duct cyst treatment with the help of cystectomy and bilateral fenestration surgery of the nasal cavity: a case report. Oral Maxillofac Surge Cases 3: 112-115.
- Moss HD, Hellstein JW, Johnson JD (2000) Endodontic considerations of the nasopalatine duct region. J Endod 26: 107-110. [Crossref]
- Baby TK, Pillai RK, Bindhu PR (2018) Nasopalatine duct cyst. J Dent Allied Sci 7: 91-93.
