Multiple Tuberculomas in a Transplanted Liver Mimicking Metastases of Unknown Origin
A B S T R A C T
Liver transplant recipients are immunocompromised patients, and are often susceptible to bacterial, fungal and virus infections. We report the case of liver-only tuberculomas occurring eleven years following a deceased donor liver transplantation, that was initially interpreted as metastases of unknown origin. Interestingly, only a few such cases have been reported, usually within the first two years after transplantation, often when more aggressive immunosuppression is required. Although it is accepted that tuberculosis incidence among solid organ transplant recipients is higher when compared with the general population, its late onset after transplantation is very unusual.
Keywords
Liver transplantation, tuberculosis, solid organ transplant, tuberculomas, liver metastases
Introduction
Liver transplantation (LT) recipients are susceptible to some infectious complications which are very infrequent in the general population. Among immunocompromised patients, tuberculosis (TB) is one of the most relevant opportunistic infections [1, 2]. TB transmission through transplanted kidney, lung and liver grafts has been reported previously [3]. While the occurrence of liver only TB has been described, all patients can develop early infections and clinical symptoms following hepatic transplantation (Table 1). Importantly for these patients, condition awareness and timely suspicion are required to correctly diagnose TB, as there are no outward characteristic clinical features, therefore missed symptoms could delay diagnosis and appropriate antibiotic treatment [3].
We herein report the unusual case of an immunocompromised patient who presented the incidental findings of liver-only disease, initially diagnosed as multiple liver metastases of unknown origin. This occurred 11 years following a successful LT. After investigation, the disease was finally confirmed as hepatic tuberculomas.
Case Description
We describe the case of a 57-year-old asymptomatic female who presented with an incidental finding of multiple liver tumors at a routine ultrasound. She previously had a history of primary biliary cirrhosis, which required a LT with a full-size deceased donor liver graft 11 years ago. Immunosuppression was provided via low tacrolimus doses.
Liver lesions were initially considered as multiple liver metastases of unknown origin (Figure 1). We began searching for the primary tumor using physical and complementary examinations, including bilateral mammography, colonic endoscopy, thorax computed tomography (CT) and analysis of serum digestive tumor markers (i.e. cancer antigen (Ca 19.9) and carcinoembryonic antigen (CEA)). All were normal. After multidisciplinary discussion, a liver nodule biopsy was performed. At the time of CT guided liver biopsy, a decrease in liver lesion size was observed. Due to the anatomic location of these small liver lesions, a biopsy was not possible without a high risk of complication. Therefore, we continued with empiric antibiotic treatment and close follow-up. From our investigations, we considered liver abscesses as a correct diagnosis.
Table 1: Reported Cases of Isolated Hepatic Tuberculosis following Liver Transplantation.
|
Reference (year) |
Indication for LT |
Age |
Gender |
Immunosuppressive based regimen |
Interval LT-TB diagnoses (months) |
Clinical presentation |
|
Kiuchit et al. (1997) [8] |
Biliary Atresia |
10 months |
F |
Tacrolimus |
3 |
Fever |
|
Alothman et al. (2004) [9] |
HCV |
43 years |
M |
Not reported |
18 |
Fever |
|
Berzigotti et al. (2006)[10] |
Cryptogenic |
33 years |
M |
Tacrolimus |
8 |
Fever |
|
Geramizadeh et al. (2013) [11] |
HBV |
59 years |
M |
Tacrolimus/ Sirolimus |
17 |
Fever, night sweat |
|
Present case (2020) |
Primary biliary cirrhosis |
69 years |
F |
Tacrolimus |
135 |
Liver-only multiples solid lesions |
LT: Liver transplantation
Figure 1: Axial computed tomography (CT) of the abdomen demonstrating multiple hypodense images in liver parenchyma.
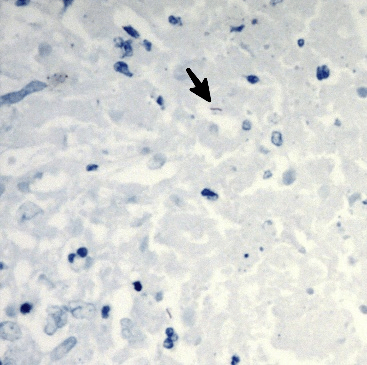
Figure 2: Histopathology section from the allograft liver shows necrotizing granulomatous inflammation with acid-fast bacilli presence (ZN 1000X).
Two months later, a new CT scan showed an increment in liver nodule sizes and numbers. We performed a percutaneous biopsy, with histopathology findings suggesting a necrotizing granulomatous inflammation, with an acid-fast bacilli presence (Figure 2). TB was confirmed, with anti-TB therapy implemented over a 12-months treatment regimen. The therapy consisted of two months on a four-drug regimen; rifampicin, isoniazid, ethambutol and levofloxacin, and 10 months on a two-drug regimen; rifampicin and isoniazid. Since rifampicin administration could decrease levels or the effects of tacrolimus by affecting hepatic/intestinal CYP3A4 enzyme metabolism, tacrolimus doses were monitored and adjusted during therapy to maintain target plasma levels of 4-6 ng/mL. During antibiotic therapy, patient outcomes were uneventful, with a complete disappearance of multiple liver lesions after three months, from initiation of the specific anti-TB therapy. Immunosuppression and liver graft function was managed according to laboratory tests, and the clinical status of the patient. Similarly, there were no episodes of organ rejection and liver drug-toxicity. Currently, two months after completion of TB treatment, and 14 months from diagnosis, the patient continues with standard tacrolimus-based immunosuppression, displaying adequate liver graft function and no indication of TB recurrence.
A retrospective review of the deceased donor history and post-reperfusion liver biopsy did not reveal any evidence of donor-derived TB infection. Organ recipient pre-transplant work-up, including a purified protein derivative test (PPD) and chest X-rays failed to demonstrate any previous infections, with no previous history of TB to suggest future disease recurrence. On the other hand, she has no other non-medical risk factors for TB infection such as Diabetes, alcohol, malnutrition, tobacco smoke, poverty, or close contacts with other persons with known TB disease.
Discussion
To the best of our knowledge, this is the first case of late occurring liver-only TB from a graft LT. Isolated hepatic tuberculoma is only one of several reported clinical presentations for TB (Table 1), and must be included in the differential diagnosis of any patient presenting multiple early or late liver tumors after solid organ transplantation. Due to the absence of characteristic clinical features, an accurate TB diagnosis is very challenging and has the inherent risk of diagnostic delay, causing serious consequences in immunocompromised patients [3]. Therefore, a percutaneous tumor biopsy is a critical diagnostic tool for establishing a final diagnosis [4].
The presence of active TB disease on the transplant candidate contraindicates any organ transplantation surgery [1, 5-7]. The majority of reported TB cases in a solid organ transplantation setting are due to the reactivation of latent infections, as a consequence of an immunosuppressive regimen to prevent organ rejection. Therefore, it is important to assess the serological and epidemiologic status of each organ transplantation candidate, to include active investigations of TB within the family and other social contexts. However, a rare source of infection could potentially stem from the deceased donor. In our case, these two potential sources of infection were retrospectively excluded, and we failed to demonstrate any recent oligosymptomatic pneumonia as a source of this liver-only TB disease. Although it is well-established that patients undergoing solid organ transplantation are vulnerable in developing de novo systemic or localized TB in the transplanted graft, we cannot state in this case how mycobacteria could migrate to the liver without any other organ clinically infected. We can speculate that a subclinical infection occurred in the lungs and this could potentially be the origin of the mycobacteria dissemination towards the liver graft.
Immunosuppression therapy is an additional risk factor for developing post-transplant TB. Interestingly, most cases described in the literature with hepatic-only disease, occurred within two years following LT, when more aggressive immunosuppression was required [8-11]. However, it must be emphasized that TB can occur later in LT patients requiring very low immune-suppressive regimens.
Finally, as clinicians, we must be aware of the pharmacological interactions between immunosuppressive agents and TB treatment antibiotics. Therefore, these patients require strict controls during treatment to avoid hepatotoxicity and organ rejection [2, 7].
Funding
None.
Acknowledgement
We acknowledge the support of the Fundación Argentina Cancer de Hígado.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 06, May 2020Accepted: Mon 18, May 2020
Published: Wed 27, May 2020
Copyright
© 2023 Lucas McCormack. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.03.01
Author Info
Angeramo Agustín Antinucci Florencia Lucas McCormack Ramallo Darío Rodriguez Catán Julieta
Corresponding Author
Lucas McCormackLiver Surgery and Transplantation Unit, Hospital Alemán of Buenos Aires, Argentina
Figures & Tables
Table 1: Reported Cases of Isolated Hepatic Tuberculosis following Liver Transplantation.
|
Reference (year) |
Indication for LT |
Age |
Gender |
Immunosuppressive based regimen |
Interval LT-TB diagnoses (months) |
Clinical presentation |
|
Kiuchit et al. (1997) [8] |
Biliary Atresia |
10 months |
F |
Tacrolimus |
3 |
Fever |
|
Alothman et al. (2004) [9] |
HCV |
43 years |
M |
Not reported |
18 |
Fever |
|
Berzigotti et al. (2006)[10] |
Cryptogenic |
33 years |
M |
Tacrolimus |
8 |
Fever |
|
Geramizadeh et al. (2013) [11] |
HBV |
59 years |
M |
Tacrolimus/ Sirolimus |
17 |
Fever, night sweat |
|
Present case (2020) |
Primary biliary cirrhosis |
69 years |
F |
Tacrolimus |
135 |
Liver-only multiples solid lesions |
LT: Liver transplantation

References
- José María Aguado, Julián Torre-Cisneros, Jesús Fortún, Natividad Benito, Yolanda Meije et al. (2009) Documento de consenso para el tratamiento de la tuberculosis en pacientes con trasplante de órgano sólido. Enfermedades Infecciosas y Microbiología clínica 27: 465-473.
- Santoro-Lopes G, Subramanian AK, Molina I, Aguado JM, Rabagliatti R et al. (2018) Tuberculosis Recommendations for Solid Organ Transplant Recipients and Donors. Transplantation 102: S60-S65. [Crossref]
- Benito N, García-Vázquez E, Horcajada JP, González J, Oppenheimer F et al. (2015) Clinical features and outcomes of tuberculosis in transplant recipients as compared with the general population: a retrospective matched cohort study. Clin Microbiol Infect 21: 651-658. [Crossref]
- Póvoas D, Machado J, Perdigoto R, Morbey A, Veloso J et al. (2017) Tuberculosis in liver transplant recipients: A report of eight cases during a five-year period. Acta Med Port 30: 41-46. [Crossref]
- Yehia BR, Blumberg EA (2010) Mycobacterium tuberculosis infection in liver transplantation. Liver Transpl 16: 1129-1135. [Crossref]
- Ayats-Ardite J, Cisneros-Herreros JM, Pérez-Sáenz JL, de la Torre-Cisneros J (2002) [Infectious disease assessment in solid organ transplant candidates]. Enferm Infecc Microbiol Clin 20: 448-461. [Crossref]
- Holty JE, Gould MK, Meinke L, Keeffe EB, Ruoss SJ (2009) Tuberculosis in liver transplant recipients: a systematic review and meta-analysis of individual patient data. Liver Transpl 15: 894-906. [Crossref]
- Kiuchi T, Inomata Y, Uemoto S, Satomura K, Egawa H et al. (1997) A Hepatic graft tuberculosis transmitted from a living-related donor. Transplantation 63: 905-907. [Crossref]
- Alothman A, Al Abdulkareem A, Al Hemsi B, Issa S, Al Sarraj I et al. (2004) Isolated hepatic tuberculosis in a transplanted liver. Transpl Infect Dis 6: 84-86. [Crossref]
- Berzigotti A, Bianchi G, Dapporto S, Pinna AD, Zoli M (2006) Isolated hepatic tuberculoma after orthotopic liver transplantation: a case report. Intern Emerg Med 1: 314-316. [Crossref]
- Geramizadeh B, Nikeghbalian S, Janghorban P, Malekhosseini SA (2013) Isolated Tuberculosis of Transplanted Liver, a case report and review of literature. Hepat Mon 13: e6691. [Crossref]
