Journals
Microleakage in chemomechanical and chemotherapeutic approaches to Atraumatic Restorative Treatment
A B S T R A C T
Objective:
Atraumatic Restorative Treatment (ART) was developed to increase access to restorative dental care and utilizes hand instrumentation and typically glass ionomer (GI) to restore frank carious cavitation. This study examined microleakage in primary molars treated via ART, augmented either with papain-enzyme agent for caries removal or silver diamine fluoride (SDF) for caries arrest.
Methods:
Sixty extracted primary molars with frank, carious proximo-occlusal cavitations were divided into three ART groups (spoon excavator caries removal and GI restoration): 1) control, 2) pre-treatment with papain-enzyme agent and 3) pre-treatment with SDF. Specimens were thermocycled and then immersed in 2% fuchsin dye for 24 hours. After sectioning, microleakage was determined by visual examination of dye penetration at occlusal and gingival margins via stereomicroscope (20x magnification). Data was analyzed with ordinal logistic regression and Fisher’s exact test.
Results:
No significant differences in microleakage rates were observed between any of the groups for complete dye penetration (p=0.80), at the occlusal margin (p=0.19) or gingival margin (p=0.42); gingival margin above or below the CEJ did not make a difference (p=0.78). A significant effect of microleakage at the gingival margin was detected (p=7.46 x 10-6).
Conclusions:
Neither papain-enzyme or SDF in this study adversely affected microleakage in ART restorations, although case selection may favor occlusal-only restorations. If clinical presentation indicates possible benefit to use of either of these modalities, the practitioner can likely proceed without increasing marginal leakage.
K E Y W O R D S
ART, atraumatic restorative, treatment, caries, glass ionomer, microleakage, papain, silver diamine fluoride
I N T R O D U C T I O N
Contemporary operative caries management in pediatric populations tends to depend upon complicated equipment such as rotary handpieces and hydraulic dental chairs; such technology aids the practitioner in carious tissue removal and restoration with modern materials. There are scenarios, however, where access to care limitations and/or patient non-acceptance of conventional operative intervention call for modified approaches to achieve similar goals. Atraumatic Restorative Treatment (ART) combines hand instrument caries excavation and adhesive restorative materials (typically glass ionomer), most often in the absence of local anesthesia, to treat cavitated lesions. It has been suggested that ART restorations have similar survival rates when compared with conventional restorations, although other investigations call into question the quality of the current evidence [1, 2]. Regardless, ART continues to be adapted and incorporated globally in caries management regimens.
Over the years, chemomechanical (CM) adjuncts have been developed to aid the hand instrument excavation of frank cavitations into dentin. These CM agents are generally liquid/gel formulations that are applied to the infected dentin; via this interaction, the dentin is further softened through chemical breakdown, facilitating instrument excavation.3 The first CM adjuncts were sodium hypochlorite-based, but subsequent products have alternatively emphasized the fruit-derived proteolytic enzyme papain [3]. Brix 3000 (Brix SRL, Carcarana, Argentina) is one of the most recent papain-based CM adjuncts.
In recent years there has also been interest in chemotherapeutic (CT) approaches to the arrest of dental caries, namely via silver diamine fluoride (SDF). SDF, especially in its most common 38% concentration, appears to lead to the arrest of active dentinal caries lesions and prevent the occurrence of new lesions, presumably through the synergistic action of silver and fluoride ions [4, 5]. A therapy combining ART with SDF pre-treatment – silver modified atraumatic restorative technique (SMART), is being employed by dentists and thought leaders in the practice community, with accompanying anecdotal reports of enhanced patient acceptance and caries arrest success [6].
Thus, ART is a well-established approach to managing frank cavitated carious lesions. CM adjuncts such as Brix 3000, and CT therapies like SDF, may work in conjunction with ART. Generally speaking, glass ionomer (GI) restorations in primary teeth seem to exhibit lower rates of secondary caries, and demonstrate similar presentations of marginal adaptation and discoloration, when compared to composite resin [7]. It is currently unknown how pre-treatment of dentin with papain-based CM agents or SDF will affect the marginal seal of GI restorations in primary teeth, particularly in frank carious lesions that have been solely hand-excavated (as in the case of ART). Therefore, the aim of this study was to assess the effect of a papain-based CM agent and SDF on microleakage of GI restorations, when applied to frank, cavitated occluso-proximal lesions in primary molars that have been only hand-excavated.
Materials and Methods
Sixty extracted primary molars with frank, carious proximo-occlusal cavitations into dentin were collected and stored in 0.25% sodium azide (NaN3) solution at room temperature for use within six months. Institutional Review Board approval from The University of Texas Health Science Center at Houston was received (HSC-DB-17-0459), with a determination of exempt status.
The teeth divided into three groups, each group with twenty specimens. Gingival margin placement, above or below cemento-enamel junction (CEJ), of each specimen was accounted for to avoid creating a biased distribution amongst the groups. Thirty-nine teeth presented with gingival margin above CEJ (Subgroup A: enamel margin) and twenty-one teeth presented with gingival margin below the CEJ (Subgroup B: dentin margin). 13 specimens in Subgroup A and 7 specimens in Subgroup B were randomly assigned to each of the following three study groups (Table 1): (1) Control group: Infected dentin removal using hand instrument with a blunt spoon excavator, (2) CM group: Brix 3000 was applied to carious lesion for 2 minutes followed by infected dentin removal using blunt spoon excavator, (3) SDF group: Infected dentin removal using hand instrument followed by 1-minute application of 38% SDF (Advantage Arrest, Elevate Oral Care, LLC, West Palm Beach, FL, USA).
Table 1: Frequency of dye penetration at the occlusal wall
|
Score |
||||||
|
Groups |
N |
0 |
1 |
2 |
3 |
Complete leakage (not scored) |
|
1: Control group |
20 (33%) |
11 (55%) |
1 (5%) |
4 (20%) |
0 |
4 (20%) |
|
2: BRIX 3000 group |
20 (33%) |
8 (40%) |
5 (25%) |
1 (5%) |
0 |
6 (30%) |
|
3: SDF group |
20 (33%) |
10 (50%) |
5 (25%) |
1 (5%) |
0 |
4 (20%) |
|
Fisher’s Exact Test |
P-value = 0.19 |
|
||||
Dye penetration score for marginal leakage along the occlusal wall (modified from Radhika et al. 2010):
0- No dye penetration
1- Dye penetration into enamel only
2- Dye penetration at or beyond dentinoenamel junction
3- Dye penetration reaching the pulpal wall
Infected dentin removal was evaluated with tactile confirmation, which was defined as no “tug-back” sensation with a blunted explorer (Hu-Friedy TU#17/23, Chicago, USA). When ready for restoration, the samples were conditioned with 20% polyacrylic acid for 10 seconds, rinsed with water for 10 seconds, and air dried for five seconds. The cavities were then restored with GI cement (GC Fuji IX GP®, GC Corporation, Tokyo, Japan) and then GC Fuji varnish (GC America, Tokyo, Japan) was applied and light cured followed by contouring and finishing. The restorative margins were coated with GC Fuji varnish again and light cured as recommended by the manufacturer. The restored teeth were stored (37°C, 95% humidity) for 24 hours.
The teeth were then subjected to thermocycling for 500 cycles at a temperature range of 5°C and 55°C, with immersion time of 15 seconds. After thermocycling, sticky wax was placed to cover the apices of the teeth and two coats of nail varnish were applied to cover the surfaces of the tooth except within 1 mm of the periphery of the restoration to eliminate unwanted dye penetration. The specimens were then immersed in 2% fuchsin dye solution for 24 hours, removed and rinsed with water and air dried. The teeth were embedded in a chemically-activated acrylic resin and sectioned longitudinally in mesiodistal direction with a low speed diamond disk through the center of the carious lesion with aqueous irrigation. Individual sections were examined under stereomicroscope at 20x magnification.
Marginal leakage measurement
Microleakage was noted via qualitative scoring from both the occlusal and proximal surfaces, separately (Figure). The deepest point of dye penetration from both occlusal and gingival direction were recorded. In the event of complete dye penetration throughout the entire tooth-restoration interface, such result was noted and also analyzed. Dye penetration score for marginal leakage along the occlusal wall (modified from Radhika et al. 2010): (0) No dye penetration, (1) Dye penetration into enamel only, (2) Dye penetration at or beyond dentinoenamel junction, (3) Dye penetration reaching the pulpal wall [8].
Dye penetration score for marginal leakage along the gingival wall (modified from Arora et al. 2012)9: (0) No dye penetration, (1) Dye penetration up to one-third of the gingival wall, (2) Dye penetration beyond one-third up to two-third of the gingival wall, (3) Dye penetration beyond two-thirds up to full length of the gingival wall, (4) Dye penetration beyond full length of the gingival wall and reaching the axial wall.
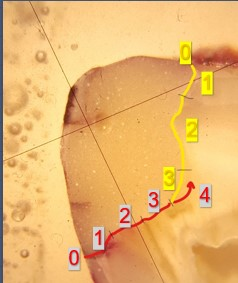
Yellow: occlusal wall; Red: gingival wall
Statistical Analysis
Ordinal logistic regression was used to analyze the effects of treatment (control and two agents) on marginal leakage (ordered categorical response variable) using polr function in the MASS package of R statistical software (R Core Team 2017). Fisher’s exact test was used to evaluate the relative frequency of dye penetration score as an indicator of marginal microleakage.
Results
Table 1 summarizes the raw microleakage scores at the occlusal margin for the groups. 55% of group 1 (control), 40% of group 2 (Brix 3000), and 50% of group 3 (SDF) demonstrated a microleakage score of 0. Overall, 52% of the primary molars in this study demonstrated leakage at the occlusal margin. There was no statistically significant difference in the microleakage scores at the occlusal margin between the three groups (p=0.19).
Table 2 shows the microleakage scores at the gingival margin for the groups. At the gingival margin, 70% of group 1 (control), 80% of group 2 (Brix 3000), and 90% of group 3 (SDF) showed some form of microleakage. When accounting for any microleakage at the gingival margin, including 1-4 and the complete dye penetration, overall microleakage was evident at the gingival margin in 80% of specimens. There was no significant difference in the marginal leakage scores between the three groups at the gingival margins (p=0.42).
Table 2: Frequency of dye penetration scores at the gingival wall
|
Score |
|||||||
|
Groups |
N |
0 |
1 |
2 |
3 |
4 |
Complete leakage (not scored) |
|
1: Control group |
20 (33%) |
6 (30%) |
2 (10%) |
2 (10%) |
1 (5%) |
5 (25%) |
4 (20%) |
|
2: BRIX 3000 group |
20 (33%) |
4 (20%) |
1 (5%) |
1 (5%) |
1 (5%) |
7 (35%) |
6 (30%) |
|
3: SDF group |
20 (33%) |
2 (10%) |
4 (20%) |
0 |
4 (20%) |
6 (20%) |
4 (20%) |
|
Fisher’s Exact Test |
P-value = 0.42 |
|
|||||
Dye penetration score for marginal leakage along the gingival wall (modified from Arora et al. 2012):
0- No dye penetration
1- Dye penetration up to one-third of the gingival wall
2- Dye penetration beyond one-third up to two-third of the gingival wall
3- Dye penetration beyond two-thirds up to full length of the gingival wall
4- Dye penetration beyond full length of the gingival wall and reaching the axial wall
Table 3 presents the leakage scores at the gingival margin, with a special focus on location of the margin (above vs below the CEJ). In group 1 (control) with gingival margin above CEJ, 38.5% showed no microleakage as opposed to only 14.3% showing no microleakage below CEJ. The same trend was observed in group 2 (Brix 3000): 23.1% showed no microleakage above CEJ and 14.3% showed no microleakge below CEJ. By contrast, in group 3 (SDF), only 7.7% of the specimens showed no microleakage above CEJ and 14.3% of the specimens showed no microleakage below CEJ. Overall there was no significant difference in leakage scores between enamel and dentin at the gingival margin (p=0.78).
Table 3: Frequency of dye penetration scores at the gingival wall with gingival margin subgroups
|
|
Score |
|||||||
|
Groups |
Subgroups |
N |
0 |
1 |
2 |
3 |
4 |
Complete leakage |
|
1: Control group |
Above CEJ |
13 (65%) |
5 (38.5%) |
1 (7.7%) |
2 (15.4%) |
1 (7.7%) |
3 (23.1%) |
1 (7.7%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
0 |
2 (28.6%) |
3 (42.9%) |
|
|
2: BRIX 3000 group |
Above CEJ |
13 (65%) |
3(23.1%) |
0 |
1 (7.7%) |
0 |
5 (38.5%) |
4 (30.8%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
1 (14.3%) |
2 (28.6%) |
2 (28.6%) |
|
|
3: SDF group |
Above CEJ |
13 (65%) |
1 (7.7%) |
3 (23.1%) |
0 |
3 (23.1%) |
4 (30.8%) |
2 (15.4%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
1 (14.3%) |
2 (28.6%) |
2 (28.6%) |
|
|
Fisher’s Exact Test |
P-value = 0.78 |
|
||||||
Dye penetration score for marginal leakage along the gingival wall (modified from Arora et al. 2012):
0- No dye penetration
1- Dye penetration up to one-third of the gingival wall
2- Dye penetration beyond one-third up to two-third of the gingival wall
3- Dye penetration beyond two-thirds up to full length of the gingival wall
4- Dye penetration beyond full length of the gingival wall and reaching the axial wall
Complete microleakage was seen in four specimens (20%) from group1, six specimens (30%) from group 2, and four specimens (20%) from group 3 (Table 4). There was no significant difference in complete dye penetration amongst the three groups (p=0.80).
The raw data for either the presence of or absence of microleakage at the gingival margin and at the occlusal margin are shown in (Table 5). This comparison indicated that occlusal and gingival margin dye penetration are not independent, as the Fisher’s exact test p-value was marginal at 0.054. There was a statistically significant difference (p=7.46 x 10-6) at the gingival margin when analysis of deviance table (Type II) was performed. This indicated that there is a significant effect of microleakage at the gingival margin.
Table 5: Dye penetration at the occlusal and gingival margin
|
|
Occlusal [Yes or No] |
|
|
Gingival [Yes or No] |
No |
Yes |
|
No |
9 |
3 |
|
Yes |
20 |
28 |
|
Fisher’s Exact Test |
P-value = 0.054 |
|
|
Analysis of Deviance Table (Type II Test) |
||
|
Gingival [Yes or No] |
P- value = 7.46 x 10-6 * |
|
|
Occlusal [Yes or No] |
P-value = 0.80 |
|
* Statistically significant (P<0.05)
Discussion
ART utilizes hand instrumentation alone for cavity excavation, followed by restoration primarily with traditional GI. This in vitro study attempted to simulate clinical ART by limiting tooth preparation of frank cavitated primary molars to a spoon excavator. The aim was to report on microleakage occurrence in GI restorations in teeth prepared in this way, with especial focus on augmentation of the technique with either CM agents like the papain-based Brix 3000 or CT agents like SDF. Several of the results of this study will be of interest to the clinician utilizing ART.
This study found no significant difference in microleakage of GI restorations at the occlusal margin between groups (p=0.19). Similarly, no significant difference in microleakage was observed at the gingival margin between groups (p=0.42), even when accounting for the margin being on enamel vs dentin (p=0.78). Additionally, there was no significant different between groups regarding observation of complete dye penetration of the GI restorations (p=0.80). Thus, in general, the results of this study suggest that neither CM caries-removal agents like Brix 3000 or CT caries-arrest agents like SDF have an adverse effect on microleakage rates of GI restorations in spoon-excavated primary molars.
Also, of interest to the clinician will be the finding that there was a strong association between microleakage and the gingival margin in this study (p=7.46 x 10-6). With this in mind, if the practitioner has concern about microleakage, selection of ART-cases may exclude Class II type restorations, since they by definition have gingival margins.
The appeal of restorative approaches like ART is at least two-fold: 1) ART does not require electric or other complex equipment to implement – it demonstrates portability, and 2) ART eliminates the use of local anesthesia and the rotary handpiece (traditional sources of dental anxiety) – it potentially increases patient acceptability [10]. Aiding caries excavation with CM agents or caries arrest with CT agents may add extra appeal for clinicians wishing to improve patient access to care [6, 11]. Considering this paradigm serves to highlight the value of this study, which examined a restorative property (microleakage) of GI as it relates to two technique modifications (Brix 3000 and silver diamine fluoride).
The existing literature regarding microleakage in ART restorations provides further context for the present study. GI restorations of ART-prepared teeth seem to have comparable microleakage rates to traditional amalgam restorations in primary molars [12]. The use of hand instrumentation (ART) versus rotary handpiece does not seem to adversely affect GI microleakage [13-14]. Outside of these few studies, the authors did not encounter others in the widely disseminated literature that specifically examined microleakage in hand-instrumented primary teeth.
Similarly, there is a dearth of literature regarding microleakage in teeth treated with CM or CT agents. For CM agents, the most common comparison is CM versus rotary handpiece caries removal. The 2017 study found that papain-based CM did not result in significantly different microleakage rates in composite resin restorations, while a 2015 study reported that papain-based CM resulted in greater occurrence of pulpal-floor depth penetration microleakage in GI restorations [15, 16]. The authors are aware of one published manuscript regarding silver diamine fluoride and microleakage; a 2013 study of rotary handpiece-prepared, non-carious third molars found that 38% SDF did not adversely affect microleakage in composite resin restorations [17].
Thus, as far as the authors know, the present study is the first to 1) report on SDF’s effect on microleakage of GI restorations, in particular those teeth prepared by hand instrumentation alone, and 2) compare microleakage of GI restorations prepared with papain-based CM agent versus solely hand instrumentation. With hand instrumentation (traditional ART) as the control, neither SDF or papain-based CM agent adversely affected microleakage in GI restorations. This might provide some measure of confidence for clinicians who elect to incorporate these agents into their ART approach.
In reflection, the authors note a few limitations of this study, which in turn may lead to further investigation. For simplicity, only one hand instrument (spoon excavator) was used in the preparation of the specimens. While generally effective for removal of infected dentin, this instrument was not as useful for smoothing margins and removing unsupported enamel. The ART technique allows for the use of additional enamel hatchets to refine margins; this might have resulted in more favorable microleakage rates. Also, restorative material in this study was limited to traditional GI. Acknowledging the regular use in dentistry of other related materials, especially resin-modified GI and other formulations of GI, future studies may incorporate a diversity of materials in experimental groups to inform best practices.
Acknowledgements
The authors would like to thank Dr. Nat Holland for his statistical assistance, and Dr. Mustafa Abu al Tamn for his guidance in laboratory specimen preparation. There were no funding sources for this study.
Article Info
Article Type
Case ReportPublication history
Received 29 November, 2018Accepted 20 December, 2018
Published 31 December, 2018
Copyright
© 2018 Ryan L. Quock. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository. All rights reserved.DOI: 10.31487/j.ORD.2018.01.002
Author Info
Corresponding author
Ryan L. QuockDepartment of Restorative Dentistry & Prosthodontics, University of Texas School of Dentistry, 7500 Cambridge, Houston.
Figures & Tables
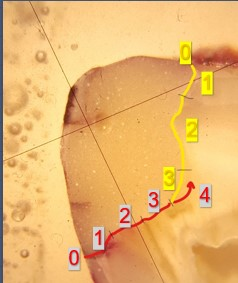
Yellow: occlusal wall; Red: gingival wall
Table 1: Frequency of dye penetration at the occlusal wall
|
Score |
||||||
|
Groups |
N |
0 |
1 |
2 |
3 |
Complete leakage (not scored) |
|
1: Control group |
20 (33%) |
11 (55%) |
1 (5%) |
4 (20%) |
0 |
4 (20%) |
|
2: BRIX 3000 group |
20 (33%) |
8 (40%) |
5 (25%) |
1 (5%) |
0 |
6 (30%) |
|
3: SDF group |
20 (33%) |
10 (50%) |
5 (25%) |
1 (5%) |
0 |
4 (20%) |
|
Fisher’s Exact Test |
P-value = 0.19 |
|
||||
Dye penetration score for marginal leakage along the occlusal wall (modified from Radhika et al. 2010):
0- No dye penetration
1- Dye penetration into enamel only
2- Dye penetration at or beyond dentinoenamel junction
3- Dye penetration reaching the pulpal wall
Table 2: Frequency of dye penetration scores at the gingival wall
|
Score |
|||||||
|
Groups |
N |
0 |
1 |
2 |
3 |
4 |
Complete leakage (not scored) |
|
1: Control group |
20 (33%) |
6 (30%) |
2 (10%) |
2 (10%) |
1 (5%) |
5 (25%) |
4 (20%) |
|
2: BRIX 3000 group |
20 (33%) |
4 (20%) |
1 (5%) |
1 (5%) |
1 (5%) |
7 (35%) |
6 (30%) |
|
3: SDF group |
20 (33%) |
2 (10%) |
4 (20%) |
0 |
4 (20%) |
6 (20%) |
4 (20%) |
|
Fisher’s Exact Test |
P-value = 0.42 |
|
|||||
Dye penetration score for marginal leakage along the gingival wall (modified from Arora et al. 2012):
0- No dye penetration
1- Dye penetration up to one-third of the gingival wall
2- Dye penetration beyond one-third up to two-third of the gingival wall
3- Dye penetration beyond two-thirds up to full length of the gingival wall
4- Dye penetration beyond full length of the gingival wall and reaching the axial wall
Table 3: Frequency of dye penetration scores at the gingival wall with gingival margin subgroups
|
|
Score |
|||||||
|
Groups |
Subgroups |
N |
0 |
1 |
2 |
3 |
4 |
Complete leakage |
|
1: Control group |
Above CEJ |
13 (65%) |
5 (38.5%) |
1 (7.7%) |
2 (15.4%) |
1 (7.7%) |
3 (23.1%) |
1 (7.7%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
0 |
2 (28.6%) |
3 (42.9%) |
|
|
2: BRIX 3000 group |
Above CEJ |
13 (65%) |
3(23.1%) |
0 |
1 (7.7%) |
0 |
5 (38.5%) |
4 (30.8%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
1 (14.3%) |
2 (28.6%) |
2 (28.6%) |
|
|
3: SDF group |
Above CEJ |
13 (65%) |
1 (7.7%) |
3 (23.1%) |
0 |
3 (23.1%) |
4 (30.8%) |
2 (15.4%) |
|
Below CEJ |
7 (35%) |
1 (14.3%) |
1 (14.3%) |
0 |
1 (14.3%) |
2 (28.6%) |
2 (28.6%) |
|
|
Fisher’s Exact Test |
P-value = 0.78 |
|
||||||
Dye penetration score for marginal leakage along the gingival wall (modified from Arora et al. 2012):
0- No dye penetration
1- Dye penetration up to one-third of the gingival wall
2- Dye penetration beyond one-third up to two-third of the gingival wall
3- Dye penetration beyond two-thirds up to full length of the gingival wall
4- Dye penetration beyond full length of the gingival wall and reaching the axial wall
Complete microleakage was seen in four specimens (20%) from group1, six specimens (30%) from group 2, and four specimens (20%) from group 3 (Table 4). There was no significant difference in complete dye penetration amongst the three groups (p=0.80).
Table 5: Dye penetration at the occlusal and gingival margin
|
|
Occlusal [Yes or No] |
|
|
Gingival [Yes or No] |
No |
Yes |
|
No |
9 |
3 |
|
Yes |
20 |
28 |
|
Fisher’s Exact Test |
P-value = 0.054 |
|
|
Analysis of Deviance Table (Type II Test) |
||
|
Gingival [Yes or No] |
P- value = 7.46 x 10-6 * |
|
|
Occlusal [Yes or No] |
P-value = 0.80 |
|
* Statistically significant (P<0.05)
References
- Tedesco TK, Bissoto Calvo AF, Lenzi TL, Hesse D, Brandao Gugliemi CA, et al. (2017) ART is an alternative for restoring occlusoproximal cavities in primary teeth – evidence from an updated systematic review and meta-analysis. Int J Paediatr Dent 7: 201-209. [Crossref]
- Dorri M, Martinez-Zapata MJ, Walsh T, Marinho VC, Sheiham Deceased A, et al. (2017) Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database Systematic. [Crossref]
- Hamama H, Yiu C, Burrow M (2014) Current update of chemomechanical caries removal methods. Aust Dent J 59: 446-456. [Crossref]
- Mei ML, Lo ECM, Chu CH (2018) Arresting dentine caries with silver diamine fluoride: What’s behind it? J Dent Res 97: 751-758. [Crossref]
- Rosenblatt A, Stamford TC, Niederman R (2009) Silver diamine fluoride: A caries “silver-fluoride bullet.” J Dent Res 88: 116-125. [Crossref]
- Alvear Fa B, Jew JA, Wong A, Young DA (2016) Silver modified atraumatic restorative technique (SMART): An alternative caries prevention tool. Stomatol Edu J 3: 243-249.
- Dias AGA, Magno MB, Delbem ACB, Cunha RF, Maia LC, et al. (2018) Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: A systematic review and meta-analysis. J Dent 73: 1-13. [Crossref]
- Radhika M, Sajjan GS, Kumaraswamy BN, Mittal N (2010) Effect of different placement techniques on marginal microleakage of deep class-II cavities restored with two composite resin formulations. J Conserv Dent 13: 9-15. [Crossref]
- Arora R, Kapur R, Sibal N, Juneja S (2012) Evaluation of microleakage in Class II cavities using packable composite with and without use of liners. Int J Clin Pediatr Dent 5: 178-184. [Crossref]
- Asl AM, Shokravi M, Jamali Z, Shirazi S (2017) Barriers and drawbacks of the assessment of dental fear, dental anxiety and dental phobia in children: A critical literature review. J Clin Pediatr Dent 41: 399-423. [Crossref]
- Deng Y, Feng G, Hu B, Kuang Y, Song J (2018) Effects of Papacarie on children with dental caries in primary teeth: A systematic review and meta-analysis. Int J Paediatr Dent 28: 361-372. [Crossref]
- Mijan MC, Leal SC, Bronkhorst EM, Frencken JE (2018) Are clinically successful amalgam and ART restorations in primary molars microgap free? J Adhes Dent 20: 25-32. [Crossref]
- Wadenya RO, Yego C, Mante FK (2010) Marginal microleakage of alternative restorative treatment an conventional glass ionomer restorations in extracted primary molars. J Dent Child (Chic) 77: 32-35. [Crossref]
- Wadenya R, Mante FK (2007) An in vitro comparison of marginal microleakage of alternative restorative treatment and conventional glass ionomer restorations in extracted permanent molars. Pediatr Den 29: 303-307. [Crossref]
- Hafez MA, Elkateb M, El Shabrawy S, Mahmoud A, El Meligy O (2017) Microleakage evaluation of composite restorations following papain-based chemo-mechanical caries removal in primary teeth. J Clin Pediatr Dent 41: 43-61. [Crossref]
- Kitsahawong K, Seminario AL, Pungchangchaikul P, Rattanacharoenthum A, Pitiphat W (2015) Chemomechanical versus drilling methods for caries removal: An in vitro study. Braz Oral Res 29: 1-18. [Crossref]
- Uzel I, Ulukent O, Cogulu D (2013) The effect of silver diamine fluoride on microleakage of resin composite. J Int Dent Med Res 6: 105-108. [Crossref]
