Mastoiditis and Tegmen Tympani Defect Leading to Intracranial Abscess with Actinomyces odontolyticus
A B S T R A C T
Introduction: Central nervous system (CNS) actinomycosis typically presents from the local spread of infection via the ear, sinus, or cervicofacial region, resulting most commonly in abscesses. Only one other case report reports on cerebral abscess with Actinomyces odontolyticus.
Presentation of Case: A 60-year-old male presented with cognitive impairment and speech difficulties. Imaging revealed a cerebral abscess in the left temporal lobe causing significant mass effect and uncal herniation. Bony erosion was noted along the middle cranial fossa with fluid attenuation of the middle ear and mastoid. An emergent surgery was performed with neurosurgery and otolaryngology. Initially, a left craniotomy was performed in order to obtain access to the left temporal lobe. A vascularized flap was harvested from the fascia of the temporalis in order to repair any defects along the middle cranial fossa. The abscess was drained using ultrasound guidance. A mastoidectomy was then performed for source control. Cultures revealed Actinomyces odontolyticus for which intravenous antibiotics were administered. The patient developed postoperative seizures requiring monitoring and anti-epileptic medication. Follow-up revealed continued improvement in the patient’s cognition.
Discussion: Cerebral abscess in the temporal lobe along the floor of the middle cranial fossa can be due to direct extension of infection from the middle ear or mastoid which requires a multidisciplinary approach to surgical treatment. Actinomycosis is a rare pathogen for CNS infection with only one other case report of CNS Actinomyces odontolyticus. Postoperative care in regards to antibiotic treatment and follow-up are also reviewed.
Conclusion: The case highlights the urgency of treatment and surgical decision making made intraoperatively by both neurosurgery and otolaryngology in regards to drainage, repair of the defect, and treatment of infectious source.
Keywords
Cerebral abscess, Actinomyces odontolyticus
Introduction
Actinomyces species are non-spore-forming Gram-positive strict or facultative anaerobic bacteria among the commensal flora of the oropharynx, gastrointestinal tract, and female genitourinary tract. It is characterized by abscess formation and frequently causes infections of the oral mucosa, face/neck, lungs, gastrointestinal tract, and a wide range of other sites [1]. Infections of the central nervous system (CNS) are rarely diagnosed given that Actinomycotic bacteria are difficult to culture; they have to be taken to the laboratory immediately under strict anaerobic conditions [2]. CNS involvement is often the result of hematogenous spread to the brain parenchyma but can also result from contiguous spread from a cervicofacial lesion. A review of 70 cases of CNS actinomycosis found that the most common lesion type was brain abscess (67%), and that these often develop from contiguous foci (ear, sinus, and cervicofacial region) [3]. Of the currently published case reports to date involving CNS Actinomycosis, only one depicts cerebral abscess caused by Actinomyces odontolyticus [4]. This case report highlights a unique pathology and pathogen and the necessary multidisciplinary approach in treatment.
Case Presentation
A 60-year-old, immunocompetent male presented with worsening mental status and speech difficulties in the days preceding admission. On examination, the patient displayed receptive aphasia, and with no family at bedside, past medical history was limited. Imaging revealed a left temporal lobe mass suspicious for an abscess with significant mass effect and vasogenic edema with the involvement of the left middle ear and mastoid. The patient was taken to the operating room with neurosurgery and otolaryngology for a left side craniotomy for drainage of the abscess, repair of the middle fossa defect, and mastoidectomy. The patient was started on broad-spectrum antibiotics until intraoperative cultures allowed for tailoring to a specific regimen. Postoperatively, the patient was found to be in focal status by electroencephalogram which resolved with anticonvulsant therapy. The patient was kept approximately two weeks as an inpatient, where he continued to recover neurologically with improvements in speech and cognition. Ultimately, he was discharged with long term intravenous antibiotics and outpatient follow-up with infectious diseases, neurosurgery, and otolaryngology.
Diagnostic Tests
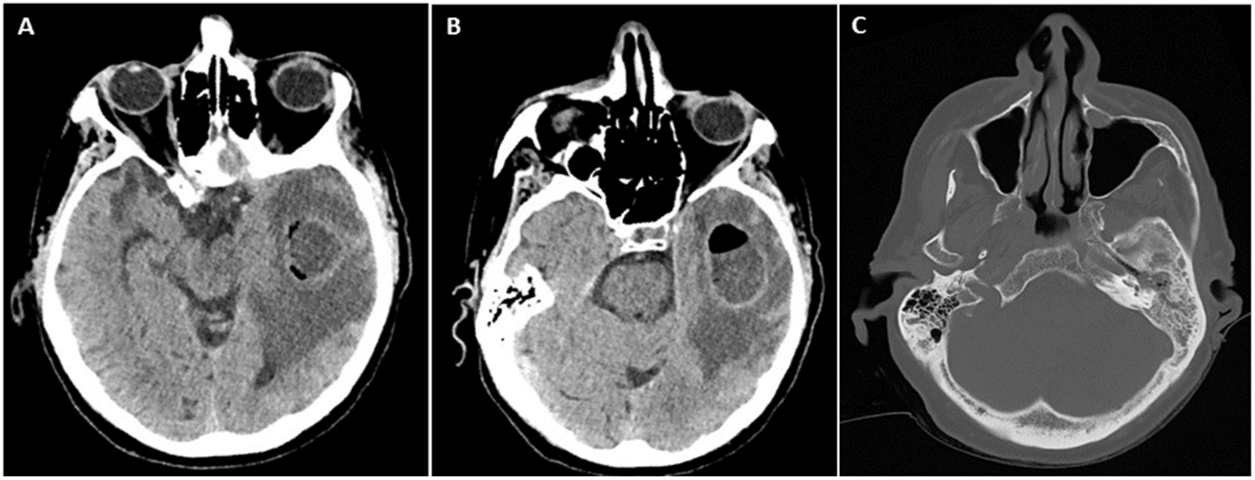
Initial examination with findings of receptive aphasia and altered mental status were pertinent in obtaining computed tomography (CT) of the head. The non-contrasted CT head showed a number of findings. A large mass within the left temporal lobe with associated vasogenic edema along with uncal herniation and midline shift was identified. The contents of the mass, including gas, as well as the location, was highly suspicious for infectious etiology. The erosion of bony anatomy and fluid-filled attenuation of the middle ear, temporal bone, and mastoid were suspicious for the source of infection and route of inoculation (Figure 1). Methicillin-resistant Staphylococcus aureus (MRSA) nares polymerase chain reaction test was obtained for surveillance purposes upon admission to the intensive care unit; results were negative and aided in empiric antibiotic de-escalation along with gram stain results from abscess culture. Blood and intraoperative abscess cultures (including fungus and acid-fast bacilli) were also obtained. There was no growth in blood cultures. All other pending microbiology tests remained without growth, except for the brain abscess bacterial culture, which grew Actinomyces odontolyticus (implied penicillin-susceptible, MIC ≤ 0.5) and Fusobacterium nucleatum [5].
Figure 1: A) A pre-operative non-contrasted CT head axial cut displays a mass in the left temporal lobe with significant vasogenic edema and mass effect resulting in uncal herniation. B) An air-fluid level identified within the mass suspicious for a gas-producing bacterium. C) The left mastoid has fluid attenuation and signs of bony erosion.
Surgical Intervention
The rapid neurologic decline and signs of uncal herniation on CT mandated urgent surgical decompression. A combined approach with neurosurgery and otolaryngology was pursued with an initial evaluation of the external acoustic meatus which revealed necrotic bone along the anterior inferior portion of the canal. A left-side craniotomy was performed to allow for access to the left temporal lobe as well as repair of any possible bony defect in the middle cranial fossa. The fascia of the temporalis was harvested with preservation of the pedicle to allow for a vascularized flap to be used in the repair of a tegmen defect in a potentially infected region. After removing the bone flap, an ultrasound was used to identify the location of the mass and a small opening made in the dura through which a ventricular catheter was passed to about 3.5 cm. Immediately air filled a syringe and then approximately 15 mL of pus was removed. The catheter was left in place and tunneled subcutaneously, exiting posterior to the incision.
The dura was then dissected away from the middle cranial fossa. Granulation tissue and a small encephalocele were identified. Multiple bony defects were identified along the floor of the middle cranial fossa. A small piece of bone taken from the initial craniotomy was used to cover the bony defect. The harvested temporalis fascia was then used as an underlay between the dura and middle cranial fossa, with the small, harvested bone acting as a buttress to avoid a secondary encephalocele and/or cerebrospinal fluid leak into the middle ear. Prosthetic material (dural substitutes) was avoided in this repair as well as non-vascularized flaps because of the fear of creating further possible infectious sources, which would not be penetrable by intravenous antibiotics. Fluid attenuation in the left mastoid was seen on the CT, so the decision was made by ENT to perform a mastoidectomy as part of source control of the patient’s infectious treatment.
Postoperative Course
Postoperatively the patient had a fluctuating level of cognition suspicious for seizures which was confirmed by video EEG. He was treated with IV fosphenytoin, which broke his seizures. The patient had been empirically started on vancomycin, cefepime and metronidazole. Once intraoperative brain abscess bacterial cultures were finalized and the pathogens identified, antibiotic therapy was narrowed to penicillin G 20 million units IV given as a continuous infusion for coverage of Actinomyces odontolyticus. In regards to Fusobacterium nucleatum, it can have increased resistance to penicillin due to the production of beta-lactamases. This resistance could be overcome with the addition of a beta-lactamase inhibitor antibiotic and it is well known that CNS penetration of these is poor. As such, it was decided to continue metronidazole 500 mg given every 8 hours for treatment of this pathogen.
Outcome and Follow-up
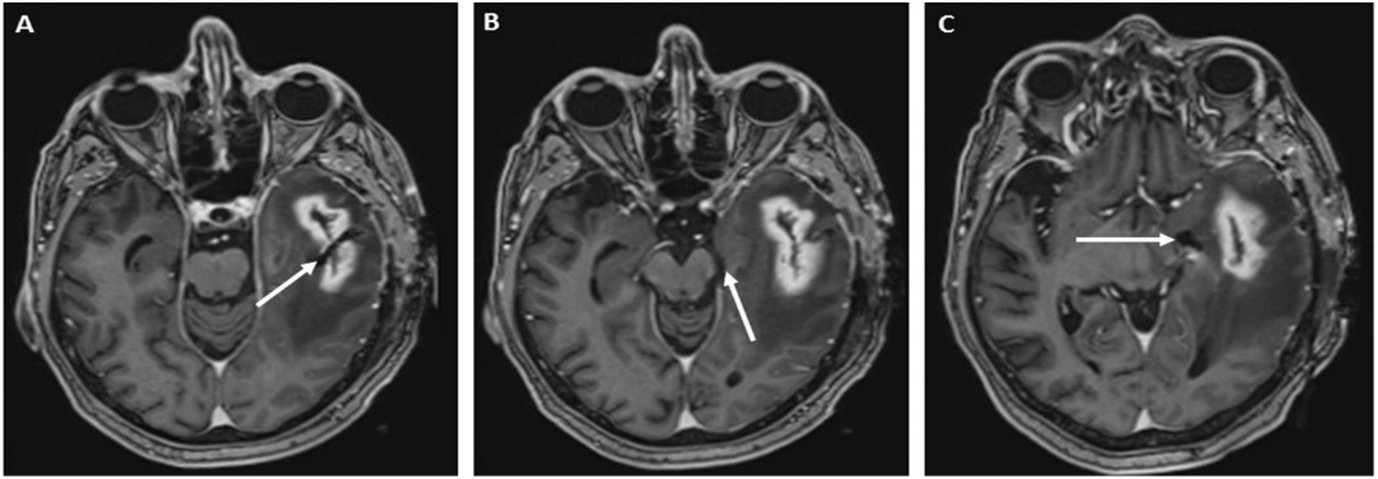
Immediately postoperatively, an MRI was obtained which showed a decrease in the size of the abscess with the placement of a drain within the abscess cavity. The previously noted uncal herniation was resolved (Figure 2). By the end of the patient’s inpatient stay, which was approximately 12 days, the patient had improved in his level of awareness and receptive aphasia. Infectious disease was consulted and recommendations were made to treat for a total of six weeks of intravenous therapy, with a transition to oral penicillin VK at the completion of intravenous antibiotics for chronic suppression secondary to the presence of Actinomyces species in the brain. As such, the patient qualified for outpatient parenteral antibiotic therapy (OPAT) clinic follow-up. Upon record review at the first OPAT clinic follow-up, it was noted the brain abscess bacterial cultures had been updated after hospital discharge and were showing additional growth of Capnocytophaga species. This organism is known to produce beta-lactamases and was not being appropriately covered with the current regimen. Thus, the antibiotic regimen was switched to monotherapy with meropenem 2 grams given every 8 hours, as it has activity against all isolated pathogens, is stable against beta-lactamases, and has excellent CNS penetration.
At two months follow-up, the patient showed continued improvement with the ability to follow simple commands and improved orientation but still had difficulty in recollecting the events of his hospitalization or recent medical care.
Figure 2: A) A postoperative MRI with contrast identifies evacuation of the previously identified abscess with persistent ring enhancement around abscess capsule as well as a linear hypo-intensity secondary to the catheter that was left within the abscess. B) Uncal herniation previously seen on the CT is resolved with the opening of the ambient cistern. C) The left temporal horn is now seen and there is no signs of contrast enhancement or restricted diffusion within the ventricle to signify ventriculitis, a poor prognostic sign.
Discussion
CNS involvement in actinomycosis infection is rare with a 5% prevalence [6]. It can present as meningitis, subdural empyema, epidural abscess, and/or intraparenchymal abscess, with cerebral abscess accounting for 75% of CNS actinomycotic lesions [3]. The site of the infection within the CNS can help in locating a source. The most common subtype is Actinomyces israelii [7]. The majority of infections spread via hematogenous route; however, a direct extension of the cervicofacial disease can occur. This case reports on a temporal lobe abscess that arose from direct extension of the middle ear and mastoid. The size of the abscess and mass effect on the brainstem called for emergent drainage of the cerebral abscess. However, radiographic findings, including the location of the abscess, mastoiditis and bony erosion of the temporal bone, prompted exploration of the underlying skull base of the middle cranial fossa to identify a possible defect and source for the cerebral abscess. A combined surgical approach with neurosurgery and ENT allowed for drainage of the abscess, repair of the tegmen defect as well as source control of the infection by performing a mastoidectomy. The repair of the tegmen defect was done with a vascularized temporalis fascial graft so as to avoid the use of a prosthetic graft which could be colonized and become yet another source of infection.
Conclusion
Actinomycosis is a rare invasive infection, which makes diagnosis difficult and can pose life-threatening complications such as cerebral abscess, meningitis, or meningoencephalitis. Invasive actinomycosis treatment usually consists of surgical intervention with long-term adjunctive therapy with penicillin antibiotics. A temporal lobe abscess along the middle cranial fossa should raise concern for a direct inoculation from the middle ear or mastoid. A multidisciplinary surgical approach with Neurosurgery and ENT should be formed early so as to treat the abscess, any middle cranial fossa defect, and source of infection. In regards to repair, a vascularized flap (i.e. temporalis fascia or temporalis) should be used in lieu of prosthetic grafts when repairing defects so as not to introduce a foreign body that could then become a source of infection.
Conflicts of Interest
None.
Funding
None.
Consent
There is no identifying data in this case report; nonetheless, written consent to publish was obtained.
Article Info
Article Type
Case ReportPublication history
Received: Wed 18, Nov 2020Accepted: Wed 02, Dec 2020
Published: Mon 14, Dec 2020
Copyright
© 2023 Omar S. Akbik. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.04.02
Author Info
Omar S. Akbik M. Gabriela Cabanilla Bradley P. Pickett Christian B. Ricks
Corresponding Author
Omar S. AkbikDepartment of Neurosurgery, University of New Mexico Hospital, Albuquerque, New Mexico, USA
Figures & Tables
References
- Valour F, Senechal A, Dupieux C, Karsenty J, Lustig S et al. (2014) Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist 7: 183-197. [Crossref]
- Moazzam AA, Rajagopal SM, Sedghizadeh PP, Zada G, Habibian M (2015) Intracranial bacterial infections of oral origin. J Clin Neurosci 22: 800-806. [Crossref]
- Smego RA Jr (1987) Actinomycosis of the central nervous system. Rev Infect Dis 9: 855-865. [Crossref]
- Hutton RM, Behrens RH (1979) Actinomyces odontolyticus as a cause of brain abscess. J Infect 1: 195-197.
- CLSI, editor (2018) Methods for antimicrobial susceptibility testing of anaerobic bacteria. 9th ed. Wayne, PA: Clinical and Laboratory Standards Institute.
- Rolfe R, Steed LL, Salgado C, Kilby JM (2016) Actinomyces meyeri, a Common Agent of Actinomycosis. Am J Med Sci 352: 53-62. [Crossref]
- Russo TA (2015) Agents of Actinomycosis. In: Bennett JE, Mandell GL, Douglas (2015) Bennett's Principles and Practice of Infectious Disease. 8th ed. Philadelphia, PA: Churchill Livingstone Elsevier 2: 2864-2873.
