Management of Stained Fluorotic Teeth by Combined Minimal Invasive Esthetic Procedure – Case Series
A B S T R A C T
Objective: Esthetic management of stained fluorotic teeth mainly depends on clinical presentation of the condition. Clinical presentation of fluorotic teeth is varied and clinician must be able to appreciate this and choose the appropriate treatment option.
Clinical Considerations: Contemporary esthetic procedures allow these teeth to be restored to have appearance similar to normal healthy teeth in the most minimalistic invasive manner. This case report aims to highlight the three-treatment combination for esthetic correction of fluorotic teeth. Also, inform about the advantages, drawbacks of various treatment choices and apprise the clinician of the appropriate esthetic conservative management protocol for dental fluorosis with diverse clinical appearance.
Conclusion: The combination of microabrasion, dentist supervised at-home bleaching and resin infiltration is the most minimalistic invasive treatment option for changing the appearance of stained fluorotic teeth to normal healthy teeth.
Keywords
At-home bleaching, brown stains, dental fluorosis, in-office bleaching, microabrasion, resin infiltration, white patches
Introduction
Dental fluorosis is a condition that affects the enamel, caused by overexposure to fluoride during tooth formation. Hypermineralized and hypomineralized areas appear in the enamel that is being formed. Resulting in whitish opaque discolorations ranging from yellow to brown with or without porosities in the enamel surface [1, 2]. Fluorosis staining of anterior teeth constitute esthetic problem which has been shown to have psychological impact and also have adverse impact on the academic performance among the affected individuals [3, 4]. Thus conservative esthetic management of dental fluorosis not only improves the smiles but also greatly enhances the self-esteem of the affected individuals. Geological crust of India, especially South India, has fluoride-rich bearing minerals which can contaminate underground drinking water resources [5]. In the Madurai district of Tamil Nadu, where this study was conducted,fluorosis is endemic with fluoride level in drinking water ranging from 1.5 to 5.0 ppm [6].
The management of dental fluorotic stain is accomplished by three strategies: i. removing the stained enamel, ii. bleaching the enamel surface or iii. covering the stained enamel surface [7]. These strategies are either done separately or in combination. Microabrasion has been reported in a previous study from the authors’ department to receive high level of patients’ acceptance without tooth sensitivity [8]. One drawback noted in this trial was the color change (ΔE) that is greater than 3.7 units, and it was recommended that microabrasion needs to be followed up with other bleaching procedures and resin infiltration to achieve better values [8].
Meanwhile some case reports / studies published on management of stained fluorotic teeth recommended selective mega-abrasion, microabrasion, in-office / home bleaching, resin infiltration and direct composite veneers [9-13]. No clear consensus guidelines are presently available in the scientific literature regarding the most conservative and esthetic management for stained fluorotic teeth. This case series present esthetic management of five cases with dental fluorosis by a two or three minimal invasive treatment protocol and also highlight the potential drawbacks in these procedures and other alternative treatment options. The secondary objective of this report is to allow the clinician to select the appropriate treatment option for management of fluorotic teeth.
Clinical Case Report
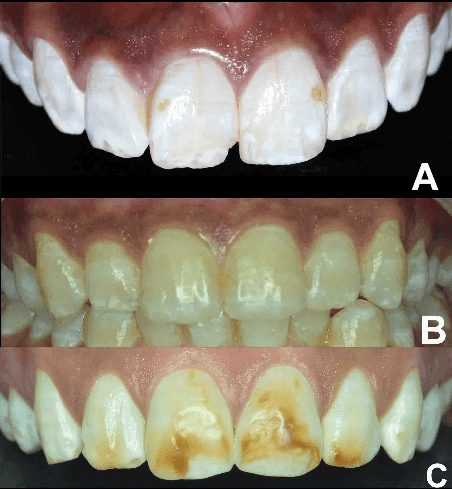
Patient reporting for improvement in appearance of fluorotic teeth can present with varying degrees of stains and / or whitish opaque areas (Figure 1). This presentation of teeth will depend upon the severity of dental fluorosis although influenced by individuals’ dietary or hygienic habits. This requires modification of treatment approach depending upon the clinical appearance of teeth [7]. Very rarely we have seen adult patients seek for esthetic management of dental fluorosis with just whitish opaque areas. In the present management report five cases of non-pitted fluorotic teeth with different clinical presentation is discussed. The desired treatment outcome from patient’s point of view for fluorotic teeth management varies according to their socio-cultural economic background [8]. Recent advances in the treatment options for fluorotic teeth has allowed for these teeth to be restored and have an appearance of a normal healthy tooth / enamel in a minimalistic invasive manner. The esthetic management procedures suggested in the present article aim to achieve normal healthy appearance for the fluorotic teeth. Some of the cases in this presentation are part of ongoing clinical trial (CTRI/2019/07/020003, CTRI/2020/03/024108) to evaluate the immediate and long-term results of microabrasion, combined with dentist supervised at-home bleaching and resin infiltration in management of stained fluorotic teeth and have signed on the informed consent form. None of the patients in the present article had any previous treatment to correct their fluorotic teeth.
Figure 1: A-C) Different grades in appearance of dental fluorosis with whitish opaque patches mild yellow to brown stains.
Case I
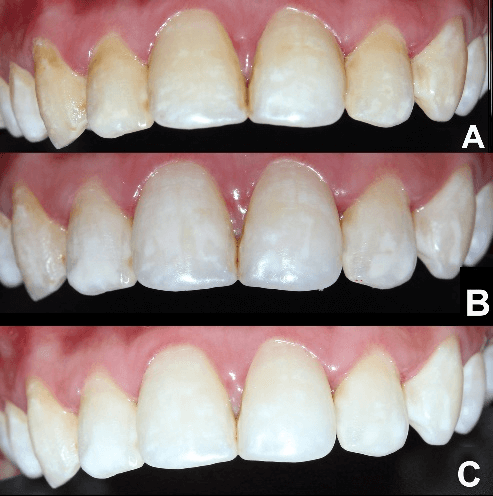
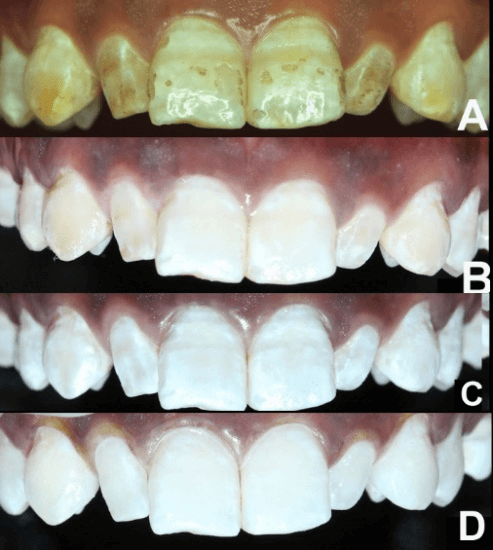
A 20-year-old female patient reported to our conservative dentistry department for want of change of appearance of her maxillary anterior teeth, her marriage was fixed in one-month time (Figure 2). Clinical assessment showed that there were mild diffused yellow stains present in her maxillary and mandibular teeth from premolar to premolar. Considering her imminent marriage arrangement, she was suggested for two weeks at home bleaching with 22% carbamide peroxide (Pola Night, SDI, Victoria, Australia) followed by resin infiltration procedure for the maxillary and mandibular stained teeth. Patient opted only for at home bleaching procedure because of financial constraint. At home bleaching tray time wear time recommended was 4 hours overnight daily.
Figure 2: A) Pre-operative view of the maxillary anterior teeth. B) Post-at home bleaching for 1 week with 22% carbamide peroxide Pola Night. C) Post-at home bleaching for 2 weeks with 22% carbamide peroxide Pola Night.
Figure 3: A) Case I, Pre-operative mild yellow stains B) that was resistant to microabrasion C) Case II, Mild yellow stains D) did not respond to microabrasion procedure and E) in-office bleaching (35% hydrogen peroxide, Pola Office, SDI, Victoria, Australia)
We did not include microabrasion for removing the yellow stains for this patient; as our previous experience in fluorotic teeth with mild yellow stains showed that these stains are resistant to microabrasion procedure and also in-office bleaching (Figure 3). Post-treatment appearance (Figure 2C) of the teeth after two weeks and its significance will be discussed in the next case of the manuscript to have a better understanding of the effect of each treatment procedure on the teeth appearance.
Case II
A 22-year-old male patient sought to department for changing the appearance of maxillary and mandibular anterior teeth. Clinical examination showed generalized whitish opaque patches and diffused mild yellow staining of his maxillary and mandibular teeth (Figure 4). Treatment plan suggested was at-home bleaching with 10% carbamide peroxide (Opalescence, Ultradent Inc., Utah, United States) for four weeks of maxillary and mandibular teeth involving his first premolars followed by resin infiltration. At-home bleaching tray time suggested was 6 – 8 hrs overnight. As observed in case I (Figure 2C) in this case also after completion of bleaching treatment procedure the teeth has whitened significantly but the evenness of shade was not there (Figure 4B) because the whitish opaque areas present pre-operatively due to sub-surface enamel porosity still existed and appeared pronouncedly. This would be observed as areas of scattered whitish patches in the lightened tooth surface. Resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) allows for a low viscosity, low contact angles and high surface tension resin to infiltrate the enamel porosities. And because of the similar refractive indices of resin and enamel surface would improve white opaque appearance and reduce the original contrast between the pores and enamel caused by light scattering and providing a more esthetic appearance of the tooth [9].
Figure 4: A) Pre-operative view of maxillary incisors. B) After 2 weeks of at-home bleaching with 10% carbamide peroxide Opalescence PF. C) Post-resin infiltration.
Four weeks following completion of at-home bleaching procedure resin infiltration was taken up for patient’s maxillary and mandibular teeth till first premolar. Resin infiltration procedure was done in accordance to manufacturers’ instructions. The etchant was applied 2 to 3 times until the whitish opaque appearance of the lesion significantly diminished upon application of the recommended drying protocol. This was followed by the application of the resin infiltrant for 3 mins followed by light curing for 40s. Second application of resin infiltrant was for 1 min followed by light curing for 40s. Immediate polishing was done using Super Snap (Shofu Inc., Kyoto, Japan) composite polishing discs. After resin infiltration, patients in this case reports were instructed to use white-colored fluoridated toothpaste for their routine oral hygiene.
An obstacle we faced following the completion of resin infiltrant procedure was the immediate staining of the tooth surface from the lunch taken by patient following treatment procedure. This was in-spite of giving advice to patient to avoid stainable food substances like coffee, aerated drinks and using white colored toothpaste. But we overlooked the effect of turmeric stain a common ingredient of South-Indian foods. This stain was removed without much difficulty using composite polishing discs (Super Snap, Shofu Inc., Kyoto, Japan) in the subsequent appointment.
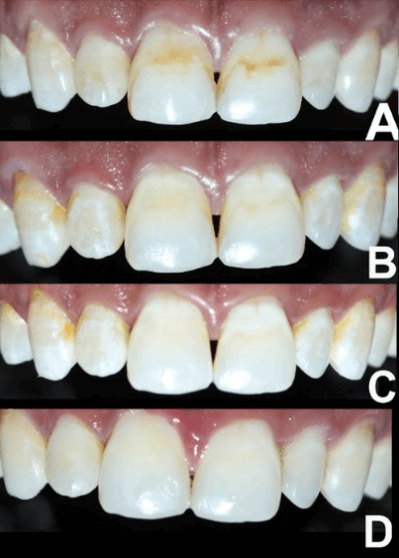
Case III
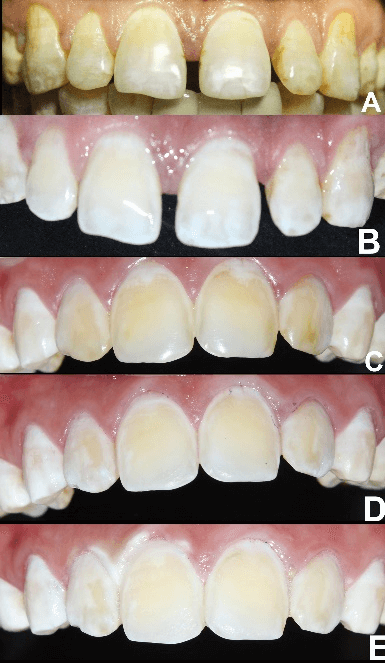
A 20-year-old male patient came to the department for complaint of unaesthetic appearance of his tooth. Upon clinical examination it was observed that his maxillary anterior teeth had brown staining with whitish opaque patches and mandibular anterior teeth with whitish opaque patches (Figure 5). Treatment plan suggested was microabrasion with Opalustre (Ultradent Products Inc, South Jordan, UT, USA), at-home bleaching with 16% carbamide peroxide (Pola Night, SDI, Victoria, Australia) for 6-8 hrs tray wear time each night. Each arch was advised for bleaching 2 weeks with 4 x 1.3gms syringes. This was followed by resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) after waiting period for two weeks.
Figure 5: A) Pre-operative view of maxillary incisors; B) Post-microabraded maxillary incisors with acquired extrinsic stains after microabrasion; C) After two weeks of bleaching with 4 syringes of at-home bleaching for each arch; D) Post- resin infiltration appearance of maxillary incisors.
Enamel Microabrasion
Light-cure resin gingival barrier (SDI, Victoria, Australia) was used to protect the gingival tissues. Microabrasion was conducted using Opalustre (Ultradent Products Inc, South Jordan, UT, USA) applied onto the stained areas of the teeth. The microabrasion technique was performed according to the manufacturer’s instructions. Briefly, a fine-grit diamond abrasive bur was used initially for 5 to 10 seconds on the stained areas of the tooth to help the microabrasion slurry penetrate into the enamel. This was followed by drying of the teeth and application of the microabrasion slurry of approximately 1- 3mm thickness onto the stained regions of the teeth. The slurry-coated surfaces were microabraded using rubber prophy cups (OpalCups, Ultradent Products Inc) attached to a gear reduction handpiece at a speed of approximately 4000 rpm with a slight pressure for 60 seconds. The teeth were rinsed with water between slurry applications. Upon assessing the stain reduction microabrasion was repeated for upto 3 times for the maxillary teeth and 1 time for mandibular teeth during the same appointment to achieve the desired result. Enamelast (Ultradent Products Inc), a flavored fluoride varnish with 5% sodium fluoride in a resin carrier, sweetened with xylitol, were applied onto the tooth surfaces and left for three minutes.
After 15 days gap at-home bleaching procedure (16% carbamide peroxide (Pola Night, SDI, Victoria, Australia)) as described earlier was initiated. In this mean time patients’ teeth got significantly stained (Figure 5B). Reason for staining could not be ascertained. As cited in case II, at the end of bleaching procedure the teeth exhibited whitish opaque patches in-spite of shade lightening (Figure 5C). Resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) was conducted as mentioned for the earlier case to mask this appearance.
Case IV
A 22-year-old female reported to department for change in appearance of her teeth and also her marriage was dependent upon on the esthetic correction of her teeth (Figure 6). On clinical examination it was observed that her maxillary and mandibular anterior teeth had brown discoloration and whitish opaque patches. She was advised for microabrasion, at-home bleaching finishing with resin infiltration for her maxillary and mandibular teeth till first premolar. Microabrasion procedure was carried out as mentioned earlier, 3 applications of Opalustre gel was needed. This was followed by at-home bleaching (16% carbamide peroxide (Pola Night, SDI, Victoria, Australia)) with earlier mentioned protocols. Two weeks after completion of bleaching protocol resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) was taken up for the maxillary and mandibular teeth till first premolar.
Figure 6: A) Pre-operative, B) post-microabrasion, C) Post- bleaching, and D) after resin infiltrated appearance of maxillary incisors.
Case V
A 35-year-old female came to the department for complaints of discoloration in her maxillary anterior teeth (Figure 7). Clinical examination showed brownish discoloration in her maxillary anterior teeth. She was advised for microabrasion with rubber dam isolation, at-home bleaching (16% carbamide peroxide (Pola Night, SDI, Victoria, Australia)) and completed with resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) procedure. Microabrasion procedure was repeated for 3 times. Resin infiltration was done for maxillary teeth till the canines two weeks after at-home bleaching completion.
Figure 7: A) Pre-operative view, B) Post-microabrasion view with acquired extrinsic stains after microabrasion, C) Post-bleaching view after two weeks with 4 syringes of at-home bleaching for each arch, And D) Post- resin infiltration viewof maxillary incisors.
Discussion
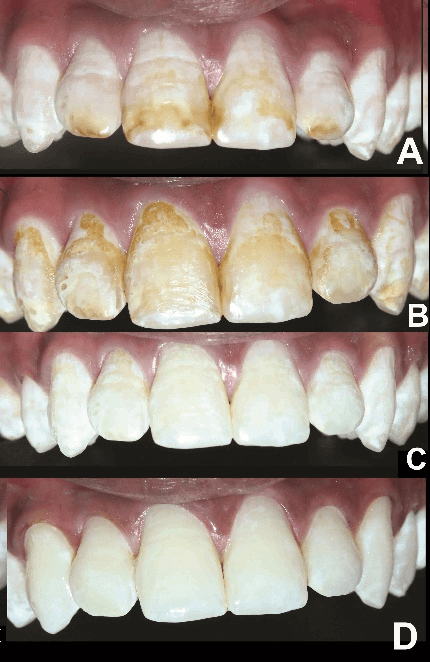
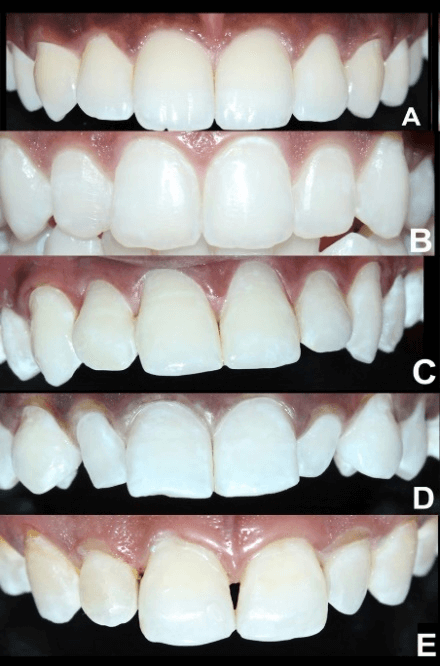
In present case report all five cases were managed by at-home bleaching with 10 or 15 or 22% carbamide peroxide in combination with / without microabrasion and resin infiltration. Cardenas et al. [14]. concluded in his systematic review that at-home bleaching improved the color change than compared to in-office bleaching. This is in agreement with our experience with in-office bleaching procedure for stained fluorotic teeth management. Figure 8 depicts the inferior post-bleaching results obtained with two products of in-office bleaching in our department for dental fluorosis management compared to at-home bleaching. Resistant of fluorotic yellow stain to in-office bleaching (35% hydrogen peroxide (Pola Office, SDI, Victoria, Australia) even after microabrasion was earlier depicted in (Figures 3C-3E). In addition, the in-office bleaching require more elaborate chair time and bleaching light to enhance the color changing effect. In-office bleaching was the suggested management protocol in authors’ department for fluorotic teeth color change from the year 2010 till 2018.
Authors’ association with management of stained dental fluorosis by minimal invasive treatment options dates back to the year 2010 and before [7]. Results demonstrated with these earlier choices were inferior and not completely satisfactory. Present outcome with at-home bleaching followed by resin infiltration (with / without microabrasion) is the least invasive treatment to change the tooth appearance. Figure 9 shows that the post-resin infiltrated fluorotic teeth appearance closest to normal healthy teeth, and the objective color evaluation using CIE L*a*b scale noticed that the L*, b* and ΔE (CIEDE2000 formula in an online delta E calculator (Link) values were similar to normal healthy enamel [8]. This finding is in agreement with a systematic review conducted by Di Giovanni et al. in 2018, the greatest esthetic improvement in the treatment of mild and moderate fluorosis, was resin infiltration combined with microabrasion or dental bleaching [15]. Also, patient acceptance of treatment results were satisfactory and except for bleaching with 22% carbamide peroxide none of patients experienced tooth sensitivity. This sensitivity was stimulus based and reduced along the duration of the treatment.
Figure 8: A-F) Cases managed by at-office bleaching with Pola Office (SDI, Victoria, Australia) (35% hydrogen peroxide). Case I, A) Before & B) after bleaching, Case II, C) Before & D) after bleaching, and Case III, E) Before & F) after bleaching. Case IV, G) Before and H) afterin-office bleaching with Opalescence BOOST (Ultradent Inc., UT, United States) (40% hydrogen peroxide). Post-bleaching result not as satisfactory compared to at-home bleaching procedure.
Figure 9: A) Normal healthy teeth of a young South Indian female. B-E) Post-resin infiltrated teeth following at-home bleaching (cases described in the manuscript) having resemblance similar to normal healthy teeth.
The shift in treatment option from in-office bleaching / composite veneers to microabrasion / dentist supervised at-home bleaching / resin infilitration has allowed for a minimal invasive procedure (without any significant tooth structure removal) to modify the appearance of fluorotic teeth to normal healthy teeth.
Garg et al. in a 12-months case report concluded about satisfactory color stability following in-office bleaching (Pola Office + (SDI, Victoria, Australia)) and resin infiltration (Icon™, DMG Chemisch-PharmazeutischeFabrik GmbH, Hamburg, Germany) for management mild to moderate fluorotic teeth with perceptible white and few brown spots [13]. Wang et al. also a 12-months case report observed the stable results following mega / microabrasion combined with in-office and at-home bleaching (Opalescence Boost and Opalescence 10%, Ultradent Inc, UT, United States) and resin infiltration for fluorotic with severe brown discoloration, tray time for at-home bleaching was not mentioned [8].
Llena et al. reported on 42-months color stability achieved with 16% carbamide peroxide (Pola Night, SDI, Victoria, Australia) with tray time of 90-mins for a period of 4-weeks in normal teeth. Celik et al. [16, 17]. combined microabrasion and in-office bleaching (Opalescence Boost, Ultradent Inc., UT, United States) for management of stained fluorotic teeth and reported about the immediate post-treatment improvement. Schoppmeier et al. used in-office light activated 25% hydrogen peroxide bleaching (ZOOM, Discus Dental, Rotterdam, Netherlands) combined with resin infiltration for management of fluorotic teeth and suggested a significant improvement and stability in masking of fluorotic opacities at 6-months after treatment [10]. Gugnani et al. combined in-office bleaching (Pola Office SDI, Victoria, Australia) and resin infiltration for management fluorosis opacity and stains in children between 6 to 12-yrs and observed improved immediate esthetic result [18].
Dentist supervised at-home bleaching is the most frequent bleaching option exercised for color change because it requires less clinical time, affords satisfactory outcome and less risk than in-office bleaching procedure [16, 19]. But most of literatures cited above have utilized in-office bleaching procedure for management of dental fluorosis. In addition, the scientific evidence cited above have utilized different methods for color change evaluation like visual analog scale, spectrophotometer and photographic assessment, which compounds to difficulty in assessing the results across different studies. Conclusions in recent review and meta-analysis on comparing the efficiency of dentist supervised at-home and in-office bleaching has been varied and has called for well-planned randomized controlled clinical trials [19, 20]. Geus et al. observed in his meta-review that the general concept of at-home bleaching being more effective cannot be established because of high variations in protocols used for each treatment procedures [19].
Literature search did not show any evidence on objective evaluation of interim or long-term clinical color stability results for at-home bleaching combined with resin infiltration and microabrasion for management of stained fluorotic teeth. One report by Celik et al. was a three-year post-treatment subjective evaluation for the stability of the color change achieved with enamel microabrasion and at-home bleaching (10% carbamide peroxide, Opalescence, Ultadent Inc, UT, United States) for fluorotic teeth [21]. It was concluded that there was significant relapse in esthetic improvement and brown stains recurrence [21]. Some of the cases in the present report are part of the clinical trial aimed to assess the long-term objective assessment of color stability achieved with at-home bleaching combined with microabrasion and resin infiltration.
Conclusion
Microabrasion allows for the stained fluorotic teeth to be more receptive for at-home bleaching along with improvement of the lightness of tooth color and removal of brown stains; at-home bleaching whitened the tooth structure along with reduction in the yellowness shade of the tooth and resin infiltration produced a homogeneous whiteness of tooth with removal of whitish opaque patches. Thus this combination of three treatment options is the most minimalistic invasive treatment option for changing the appearance of stained fluorotic teeth to normal healthy teeth.
Clinical Significance
The combination of microabrasion, dentist supervised at-home bleaching and resin infiltration is the most minimalistic invasive treatment option for changing the appearance of stained fluorotic teeth to normal healthy teeth.
Acknowledgement
We thank SDI, Victoria, Australia and DMG Chemisch-Pharmazeutische Fabrik GmbH, Hamburg, Germany for providing Pola Night 16% carbamide peroxide bleaching gel and Icon respectively for managing these patients and also for the clinical trial proceeding in the department.
Article Info
Article Type
Case SeriesPublication history
Received: Tue 12, May 2020Accepted: Sat 23, May 2020
Published: Fri 05, Jun 2020
Copyright
© 2023 Anand Sherwood. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDOA.2020.01.03
Author Info
Anand Sherwood B. Divyameena B. Rahul Bennett T. Amaechi Carmen Llena V. Nivedha
Corresponding Author
Anand SherwoodProfessor and Head, Department of Conservative Dentistry and Endodontics, CSI College of Dental Sciences, Madurai, India
Figures & Tables


References
- Pendrys DG, Stamm JW (1990) Relationship of total fluoride intake to beneficial effects and enamel fluorosis. J Dent Res 69: 529-538. [Crossref]
- Celik EU, Yildiz G, Yazkan B (2013) Clinical evaluation of enamel microabrasion for the aesthetic management of mild-to-severe dental fluorosis. J Esthet Rest Dent 25: 422-430. [Crossref]
- Sujak SL, Abdul Kadir R, Dom TN (2004) Esthetic perception and psychosocial impact of developmental enamel defects among Malaysian adolescents. J Oral Sci 46: 221-226. [Crossref]
- Niveditha B, Sabina NTM, Safoora SA, Divyadharshini C, Kalaivani K et al. (2020) Prevalence and perception of dental fluorosis among the school-going children and its impact on academic performance. Ind J Dent Sci 12: 1-6.
- Handa BK (1975) Geochemistry and genesis of fluoride containing ground waters in India. Ground Water 13: 275-281.
- Meenakshi, Maheswari RC (2006) Fluoride in drinking water and its removal. J Hazard Mater 137: 456-463. [Crossref]
- I Anand Sherwood (2010) Fluorosis varied treatment options. J Conserv Dent 13: 47-53. [Crossref]
- Divyameena B, Sherwood IA, S Rathna Piriyanga, G Deepika (2020) Clinical performance of enamel microabrasion for esthetic management of stained dental fluorosis teeth. Oper Dent.
- Wang Y, Sa Y, Liang S, Jiang T (2013) Minimally invasive treatment for esthetic management of severe dental fluorosis: a case report. Oper Dent 38: 358-362. [Crossref]
- Sundfeld RH, Franco LM, Gonçalves RS, de Alexandre RS, Machado LS et al. (2014) Accomplishing esthetics using enamel microabrasion and bleaching-a case report. Oper Dent 39: 223-227. [Crossref]
- Schoppmeier CM, Derman SHM, Noack MJ, Wicht MJ (2018) Power bleaching enhances resin infiltration masking effect of dental fluorosis. A randomized clinical trial. J Dent 79: 77-84. [Crossref]
- Sekundo C, Frese C (2020) Underlying resin infiltration and direct composite veneers for the treatment of severe white color alterations of the enamel: Case report and 13-month follow-up. Oper Dent 45: 10-18. [Crossref]
- Garg SA, Chavda SM (2020) Color masking white fluorotic spots by resin infiltration and its quantitation by computerized photographic analysis: A 12-month follow-up study. Oper Dent 45: 1-9. [Crossref]
- Cardenas AFM, Maran BM, Araújo LCR, de Siqueira FSF, Wambier LM et al. (2019) Are combined bleaching techniques better than their sole application? A systematic review and meta-analysis. Clin Oral Investig 23: 3673-3689. [Crossref]
- Di Giovanni T, Eliades T, Papageorgiou SN (2018) Interventions for dental fluorosis: A systematic review. J Esthet Rest Dent 30: 502-508. [Crossref]
- Llena C, Villanueva A, Mejias E, Forner L (2020) Bleaching efficacy of at home 16% carbamide peroxide. A long-term clinical follow-up study. J Esthet Rest Dent 32: 12-18. [Crossref]
- Celik EU, Yıldız G, Yazkan B (2013) Comparison of enamel microabrasion with a combined approach to the esthetic management of fluorosed teeth. Oper Dent 38: E134-E143. [Crossref]
- Gugnani N, Pandit IK, Gupta M, Gugnani S, Soni S et al. (2017) Comparative evaluation of esthetic changes in nonpitted fluorosis stains when treated with resin infiltration, in-office bleaching, and combination therapies. J Esthet Rest Dent 29: 317-324. [Crossref]
- J L de Geus, L M Wambier, S Kossatz, A D Loguercio, A Reis (2016) At-home vs in-office bleaching: A systematic review and meta-analysis. Oper Dent 41: 341-356. [Crossref]
- Eachempati P, Kumbargere Nagraj S, Kiran Kumar Krishanappa S, Gupta P, Yaylali IE (2018) Home-based chemically induced whitening (bleaching) of teeth in adults. Cochrane Database Syst Rev 12: CD006202. [Crossref]
- Celik EU, Yazkan B, Yildiz G, Tunac AT (2017) Clinical performance of a combined approach for the esthetic management of fluorosed teeth: Three-year results. Niger J Clin Pract 20: 943-951. [Crossref]
