Journals
Management of a severely curved canal with Proglider and WaveOne gold compounded with a separated instrument
I N T R O D U C T I O N
Anatomical disparities of the root canal system such as severe canal dilacerations may compromise the objectives of biomechanical preparation leading to severe iatrogenic errors, such as root canal transportation or unanticipated instrument separation [1, 2]. A separated instrument inside an infected root canal system is a sabotage to the attainment of root canal treatment objectives and can compromise the treatment outcome [3].
Feasible adjuncts to overcome the difficulties posed by canal curvatures include: tomographic detection and diagnosis of the multiplanar direction of the dilacerations, revised access cavity designs, pre-flaring, pre-curvature of stainless-steel hand files, evasion of NiTi rotary instrumentation, calcium hydroxide dressings mixed with glycerine and thermoplasticized gutta-percha filling techniques [4]. A glide path is a smooth and reproducible radicular tunnel extending from the root canal orifice to the radiographic canal terminus or exit as registered by an electronic apex locator [5]. Glide path preparation reduces torsional stresses and improves the life span of a rotary instrument by up to six times [6]. Patino et al. found out that the prevalence of instrument separation was significantly reduced in canals in which preparation was preceded by appropriate glide path preparation [7]. Another study revealed a higher incidence of distortion and separation of nickel-titanium (NiTi) files in the absence of preliminary glide path preparation [8].
Currently, single-file rotary glide path preparation systems like the WaveOne Gold Glider (Dentsply Sirona), ProGlider (Dentsply Sirona) and One G (Micro-Mega, Besancon Cedex, France) have been invented. Glide path preparation with the WaveOne Gold Glider before final canal preparation with WaveOne Gold might result in a reduction of clinical chair time [9]. Manual glide path preparation is also recommended by several authors who advocate the use of K-files with a 2% taper [5, 6, 10, 11]. However, more time is taken to prepare glide path using stainless steel K-files compared to the use of rotary glide path preparation techniques [12, 13].
Recently, files manufactured with gold or blue technology improve material properties that increase their fatigue resistance and flexibility in comparison to the superelastic nickel-titanium files [14, 15]. WaveOne Gold (Dentsply Sirona) is a reciprocating file with the GOLD alloy technology. The file is heated and then slowly cooled, rather than the M-Wire technology involving heat treatment before the manufacturing. In this way manufacturer claims improved flexibility through this new heat treatment method [16]. WaveOne Gold has a parallelogram cross sectional structure with two cutting edges making it more flexible. It has an off-centre design that is also seen in Protaper Next files (Dentsply Sirona). The significant modification of WaveOne Gold is in its metallurgy: the alteration of alloy from M-Wire to GOLD alloy which delivers greater flexibility than NiTi and M-wire files [17]. Instruments employing reciprocating motion have heightened resistance to instrument separation [18]. Reciprocation of these NiTi systems mitigates stress on the instrument by the counter clockwise (cutting action) and clockwise (release of the instrument) movements, thereby prolonging their durability and increasing their resistance to cyclic fatigue in contrast with systems that employ continuous rotation motion [19].
This case report presents management of a severely curved canal with Proglider and WaveOne gold compounded with a separated instrument that was successfully managed by the microsonic technique.
Case Report
A 24-year-old female presented to the Department of Endodontics, University of the East, with severe toothache on an upper right premolar. Past dental history revealed mild sensitivity to cold stimuli which progressed into mild pain.
Therefore, she visited a dentist in 2011 (7 years prior to consultation) who did a tooth coloured restoration, and this alleviated the pain. In 2017, she felt sensitivity on cold stimulus which increased in intensity. One month prior to consultation, she reported severe pain which was lingering, and she could rate it as 7. It lasted for 15-20 seconds, was nocturnal in nature but it was not associated with any concomitant symptoms. It was initially aggravated by any cold stimulus and later by chewing on the right side of the jaw. To relieve the pain, she took 4 tablets of Mefenamic acid 500mg for two days and also stopped chewing on the right side of the jaw. Her medical history was non-contributory.
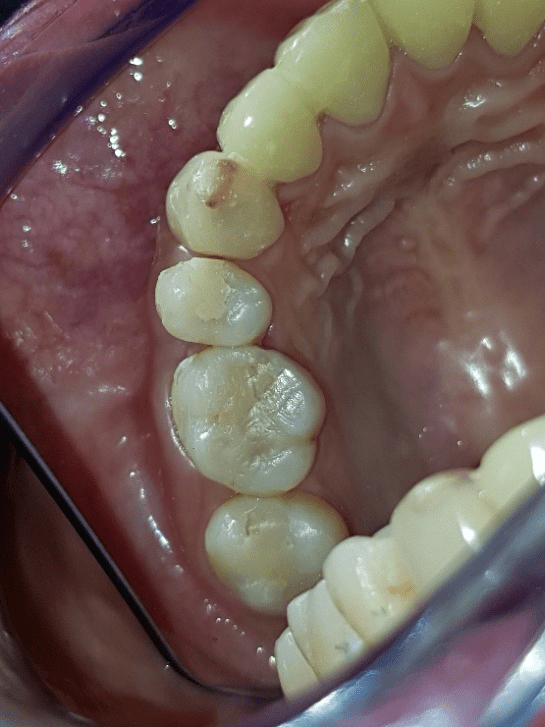
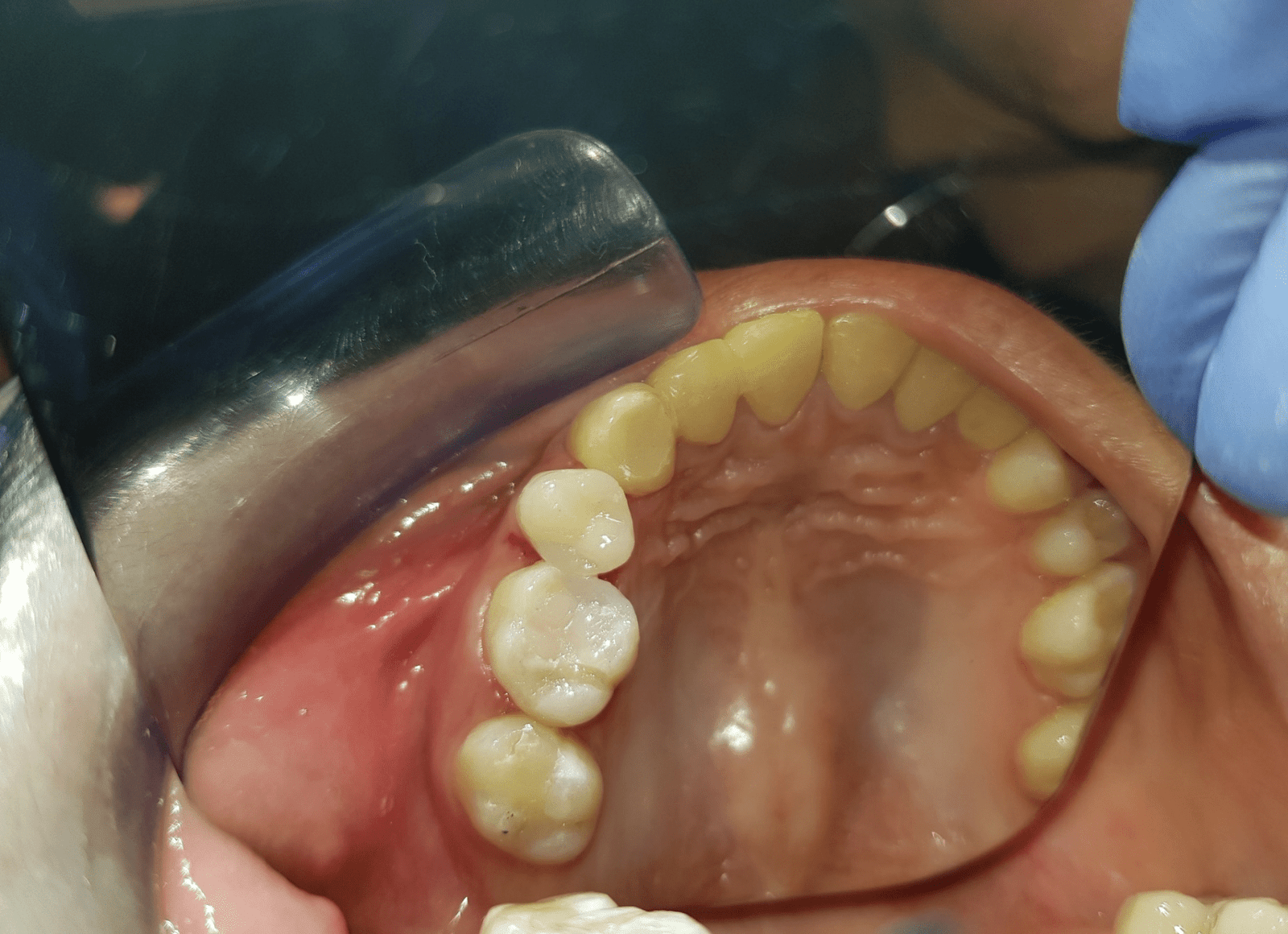
On examination, there was a composite class II restoration on mesio-occlusal surface of the offending tooth (number 15) with irregular open margins around it. The adjacent tooth (number 13) had an almost pulp exposure just beneath the acrylic crown. The patient was also missing the second premolar (Figure 1). When questioned about the missing second premolar, she revealed that her mother, a dentist, had informed her that it was congenitally missing.
Periodontal examination revealed normal probing depths (Table 1).
Table 1: Periodontal examination findings of tooth no. 15
|
MB |
1.5mm |
B |
1.0mm |
DB |
1.0mm |
|
MP |
1.5mm |
P |
1.0mm |
DP |
1.0mm |
Cold testing on tooth no. 15 with Friljet (Pierre Rolland) elicited sharp lingering pain that lasted for 10 seconds after the removal of the cold stimulus. There was an exaggerated response to percussion but a normal response to palpation. The 13 had a lingering response to cold and positive to percussion.
The contralateral tooth number 25 had normal response to all diagnostic tests (Table 2).
Table 2: Results of diagnostic testing.
|
Diagnostic Test |
Contralateral tooth no. 25 |
Offending tooth no. 15 |
Another offending tooth no. 13 |
|
Cold Test |
1:2sec |
1sec:10sec |
2sec:14sec |
|
Percussion |
- |
+++ |
+ |
|
Mobility |
Normal |
Normal |
Normal |
|
Palpation |
- |
- |
- |
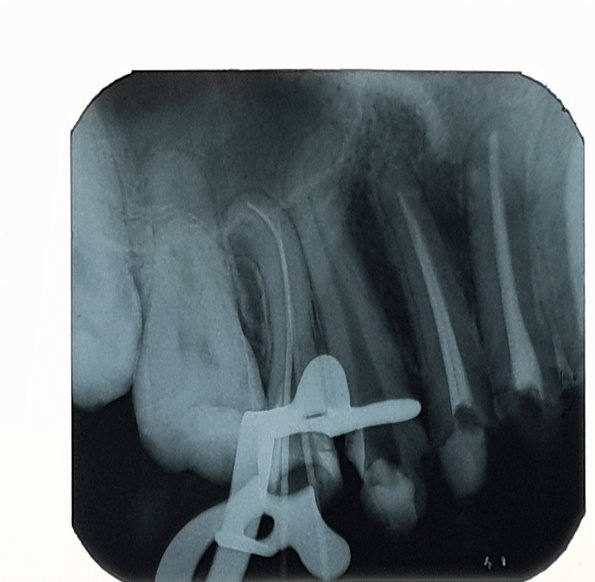
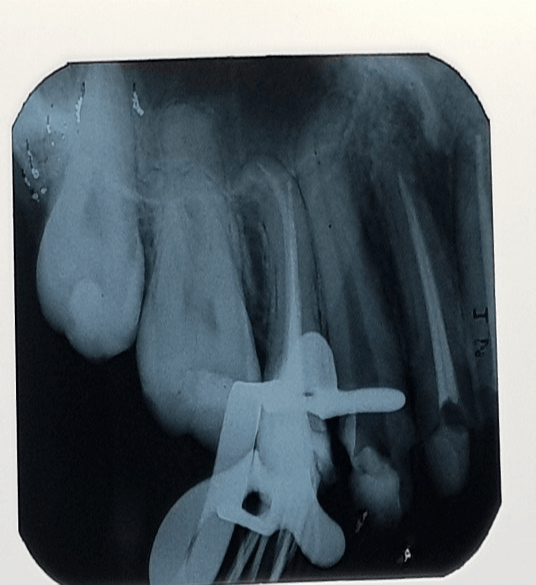
A panoramic radiograph had been taken by the referring dentist which revealed radiolucency beneath the composite restoration and on the distal aspect of the offending tooth number 15 consistent with dental caries. The root was distally dilacerated, and the patient was missing tooth number 15 (Figure 2).

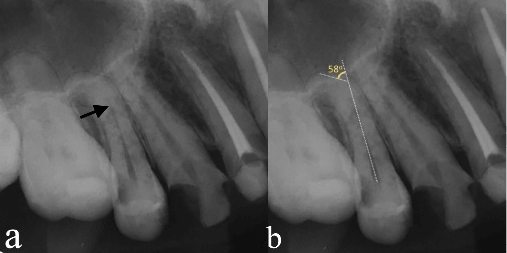
An intraoral periapical radiograph was prescribed, and it confirmed the findings on the panoramic radiograph. The lamina dura was intact and the radiolucency on the distal aspect of 15 had encroached the pulp (Figure 3a). Schneider’s method was used to determine the root curvature by drawing two lines using the apical foramen as a reference point [20]. The buccal root canal presented with a 580 curvature which was classified as severe (Figure 3b).
The pulpal diagnosis was consistent with symptomatic irreversible pulpitis, and the periapical diagnosis was consistent with symptomatic apical periodontitis of both 15 and 13. Root canal treatment was scheduled.
Treatment procedure
After obtaining signed consent from the patient, local anaesthesia was administered via the right middle superior alveolar nerve block with buccal infiltration of 15 and labial infiltration of 13 using 1.8 ml of 2% Lignocaine with 1: 100,000 epinephrine. Multiple tooth rubber dam isolation was achieved, and removal of the defective composite restoration and dental caries was done using a straight fissure bur mounted on a high seed handpiece. There was a carious exposure on distal pulp of 15 (Figure 4).
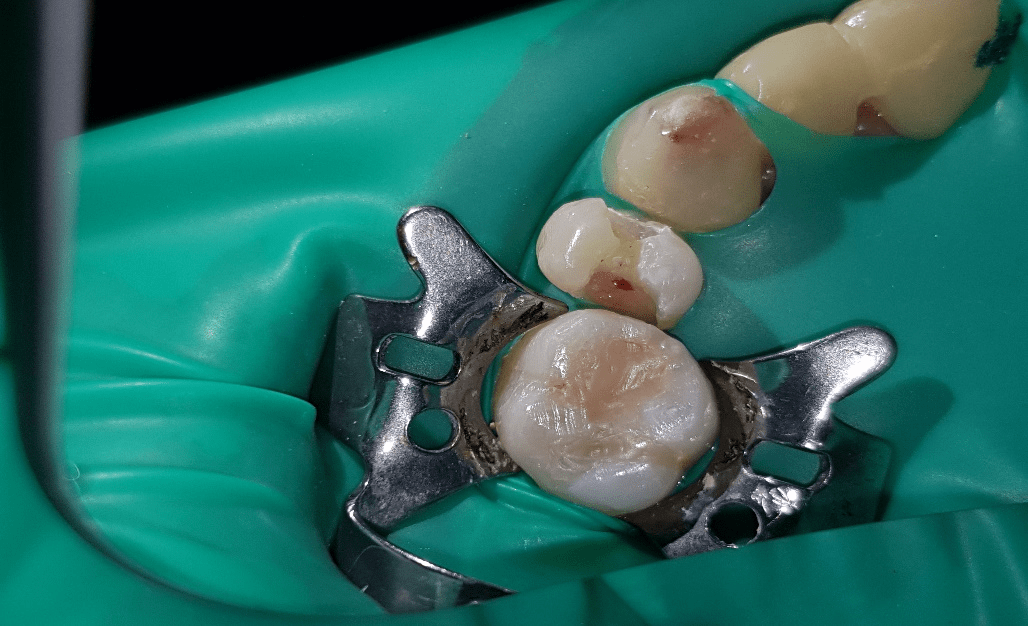
Coronal access preparation of both 13 and 15 was achieved using endo-access bur (Dentsply Sirona). The enamel and dentin of the prepared cavity was cleaned and etched with 37% phosphoric acid for 30 and 15 seconds, respectively; rinsed for 30 seconds with a water/air spray; and gently air dried to avoid desiccation. A light-polymerizing primer bond adhesive was applied; gently air thinned and exposed to a light-emitting diode polymerization for 30 seconds. The teeth were build-up using SDR composite restoration (Dentsply Sirona) as a dentine replacement which was covered on the occlusal aspect with a resin composite (BEAUTIFILL II, Shofu Dental Corporation) as per the manufacturer's instructions. Two canal orifices were identified for tooth number 15 and one canal for 13 (Figure 5).
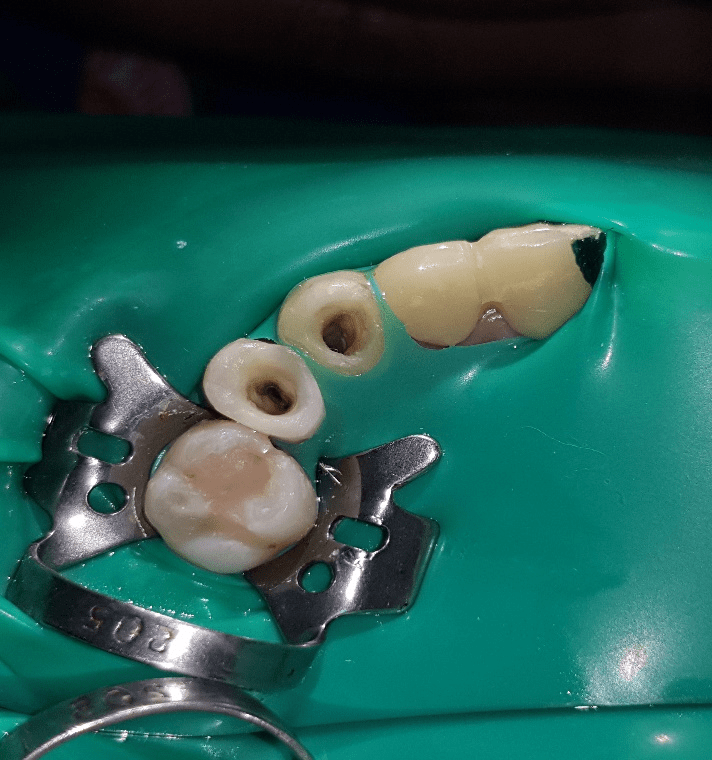
The first attempt to scout and negotiate the apical third of the curved buccal root of 15 with an ISO size 6 M-Access file (Dentsply Sirona) was hindered at the level of the first abrupt curvature that resulted in an unanticipated instrument separation. A radiograph was taken to establish its location (Figure 6).
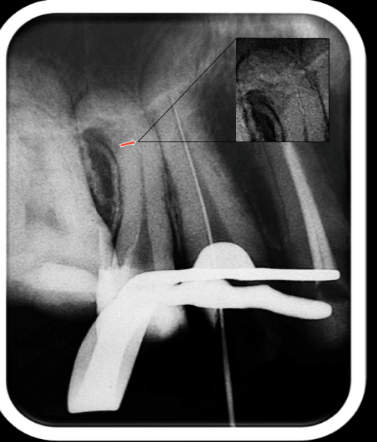
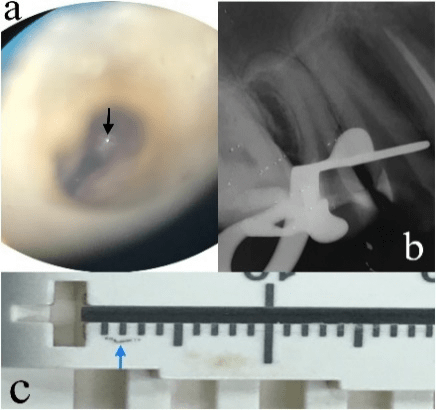
The distance from the buccal cusp to the point of the instrument separation was recorded and demarcated as the coronal zone. Removal of the separated instrument was achieved via the microsonic technique. The instrument was identified in the buccal canal (Figure 7a) under magnification and enhanced illumination via a dental operating microscope (Global Surgical Corporation).
A staging platform was then prepared at the most coronal aspect of the separated instrument using a modified Gates Glidden bur #3 (Dentsply Sirona) as described by Ruddle [21]. A fine ultrasonic tip (ET25; Acteon) was used in a counter clockwise direction to trephine dentin 1 mm deep on the inside of the curve canal wall to unlock the fragment and free it from the canal [22-24]. After 40 minutes, the instrument was successfully removed, and a radiograph was taken to confirm that there were no obstructions in the canal (Figure 7b). The separated instrument measured 2mm on a Mini Endo Bloc (Dentsply Sirona) (Figure 7c).
To attain patency to length through the curved root canal, a size 06 M-Access file (Dentsply Sirona) was pre-curved 2 mm from its tip with a tweezer and guided through the coronal zone to the level of the first abrupt curvature. The second attempt to scout and negotiate the canal was achieved by turning the file slowly with slight apical pressure below the first abrupt curvature and proper orientation was recorded. A watch-winding/pull motion was employed in order to advance the file to length. Working length was registered with Root ZX II apex locator (J. Morita, Japan) (Table 3).
Table 3: Working length measurements of the two canals.
|
Canal |
File Size |
Working Length |
Reference Point |
|
Buccal |
06 |
18.0mm |
Buccal Cusp Tip |
|
Palatal |
06 |
20.5mm |
Palatal Cusp Tip |
In this case, a manual glide path was sequentially established using ISO file numbers 06, 08, 10 up to size 15 M-Access files (Dentsply Sirona) which was confirmed on a periapical radiograph (Figure 8). The three-dimensional anatomy of the curved canal was replicated by the plastic deformation of the files. A temporary restoration (IRM- DENTSPLY Sirona) was used as a temporary restoration.
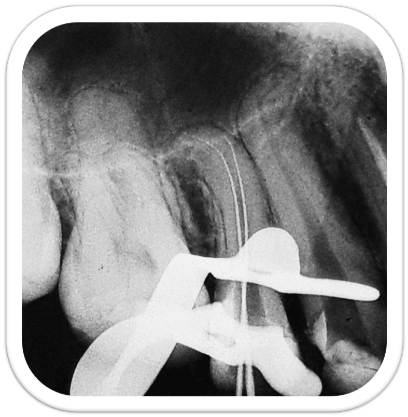
On the second appointment, ProGlider (size 16, variable taper between 2% and 8% along the shaft) (Dentsply Sirona) was mounted on the handpiece of the X-Smart Plus Endodontic motor (Dentsply Sirona) and glide path preparation was accomplished following the manufacturer’s instructions.
Biomechanical preparation was done using the Small (20/.07) followed by the Primary (25/.07) Wave One Gold rotary files (Dentsply Sirona) mounted on the X-Smart Plus endodontic motor (Dentsply Sirona) as per the manufacturer's instructions. Chemical disinfection was achieved using positive syringe irrigation with 2.5% of sodium hypochlorite as irrigant (25–28). A concentration of 15% ethylenediaminetetraacetic acid (EDTA, Glyde, Dentsply Sirona) was used as a lubricant (29–31). Gauging was done with 0.02% taper K-Flexo files (Dentsply Sirona) to determine the master apical file and a periapical radiograph was taken to confirm their fit (Figure 9).
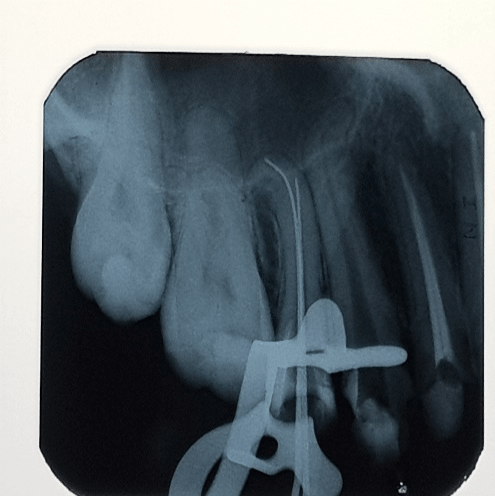
After the corresponding gutta-percha points were fitted to length, the canals were flooded with 17% EDTA solution and manual dynamic agitation of the chelating agent was performed for 1 min (32,33). The solution was flushed out with distilled water and a final rinse, before drying the canals with sterile paper points, final flash was performed with 2.5% sodium hypochlorite (32–34). The standards for obturation were verified and a master cone was placed in the respective canals until there was resistance to displacement (‘tug back’) (35). The master cone fit was confirmed radiographically (Figure 10).
Obturation was accomplished using 2% taper gutta percha cones with AH Plus (Dentsply Sirona) root canal sealer cement employing the cold lateral compaction technique. A radiograph was taken to confirm the quality of obturation (Figure 11).
The excess gutta-percha in the chamber was then seared off and vertically compacted with a heated plugger 1 mm beneath the canal orifices to enhance the coronal seal (36). Glass Ionomer cement, GIC Fuji VII (GC Dental, Japan) was placed on top of the gutta-percha to prevent coronal microleakage (35,37).
Dentine replacement was attained using SDR resin (Dentsply Sirona) with Ceram X Universal shade A2 as a capping composite following the manufacturer's instructions. A final radiograph revealed satisfactory restoration (Figure 12) and a posttreatment picture was taken (Figure 13).

After 4 months recall, the patient was completely asymptomatic both clinically and radiographically (Figure 14).

Discussion
In preparing for highly curved root canals, knowledge of the root morphology is a prerequisite. Root canal systems of human teeth usually have curvatures and aberrations. The abrupt apposition of the canal wall poses difficulty during exploration and negotiation. Such irregularities might block an endodontic hand file introduced early into the root canal during the procedure. The use of pre-curved stainless-steel hand files is essential for initial scouting to negotiate and follow the abrupt curve. The degree of the pre-curvature needed for each instrument relies on the abruptness and the locality of the curvature along the root canal length [4].
Schneider’s method was used to determine the root canal curvature in this case report [20]. It is the easiest method of canal angle measurement since it requires only drawing two lines and using the apical foramen as a reference point. In this method, he classified tooth roots into three curvature classes; straight (≤ 5 degrees), moderate (> 5 degrees, and ≤ 20 degrees), or severe (> 20 degrees). In the present study, the buccal root canal presented with 580 curvature which was classified as severe. Several quantifiable methods have been suggested to standardize root canal curvature measurements on 2D radiographic views: those that rely on the angle of root canal curvature and those that measure the radius of root canal curvature [38-45]. Although this technique also has shortcomings, Schneider’s method has gained popularity and is still in use predicting severity of root canals [46, 47].
In the present case, the first attempt to scout and negotiate the apical third of the curved buccal root of 15 with an ISO size 6 M-Access file (Dentsply Sirona) was hindered at the level of the first abrupt curvature that resulted in an unanticipated instrument separation. Endodontic instruments separate due to cyclic fatigue, torsional fatigue or a combination of both types of fatigue [48-51]. The narrow, constricted and severely curved buccal canal could have contributed to instrument separation in this case study. Cyclic fatigue fracture of the files occurs because of recurring compressive and tensile stresses amassed at the point of highest flexure in a curved canal [52-54]. Torsional failure happens when the tip of the instrument binds but the shank of the file (driven by the handpiece) continues to rotate [49]. The material then undergoes shear fracture when the maximum strength of the material is surpassed [55].
The incidence of separated NiTi files ranges from 0.4% to 23% [42, 56-60]. The location of fragment relative to root canal curvature, canal access angle, and Schneider angle significantly influence the success of instrument removal [47, 61].
Microsonic technique (also known as the Ruddle technique) is a successful method to retrieve separated instruments and therefore, was employed in this case report [21, 61]. This technique combines a dental operating microscope and ultrasonic devices, enhancing visualization and manoeuvring in the root canal system. The technique is grounded on the principle that the design of the ultrasonic instrument permits trephination of dentin around the separated fragment and the transmission of vibration to the fragment, which can be loosened and dislodged consequently [62].
A staging platform was created at the level of the obstruction using modified Gates Glidden burs [21]. Similar to other studies, a fine ultrasonic tip (ET25; Acteon) was used in a counter clockwise direction to trephine dentin around the fragment 1mm deep to unlock it and free it from the canal [23, 24]. The instrument was successfully retrieved after 40minutes. The success rate for removing separated files ranges from 33% to 95% (57,58,63,64) with the time necessary for using ultrasonic techniques varying between 3 to over 60 minutes [65-67].
After successful retrieval of the separated instrument, root canal preparation involved three distinctive stages: initial canal negotiation, creation of a glide path and canal shaping. Before introducing rotary instruments, a sufficient, smooth, secure and reproducible tunnel should be created from the canal orifice to the apical foramen [11].
Prior to the use of NiTi rotary files, that have non-active tip designs, manual instrumentation is highly recommended [68]. Therefore, size 06, 08, 10 and 15 M-Access files (Dentsply Sirona) were pre-curved 2 mm from their tip with a tweezer and sequentially guided through the coronal zone to the level of the first abrupt curvature. The second attempt to scout and negotiate the canal was achieved by turning the files slowly with slight apical pressure below the first abrupt curvature and proper orientation was recorded. A watch-winding/pull motion was employed in order to advance the files to length. It is strongly recommended to use a size 10 file to negotiate the canal to its terminus to create the smooth canal pathway prior to using any NiTi glide path rotary system [69]. However, due to the severity of the canal, manual filing was done to a ‘super loose’ size 15 file to create an effective pathway. An effective glidepath will reduce the chance of instrument separation [70].
Proglider (Dentsply Sirona) was used for glide path preparation. Currently, single-file rotary glide path preparation systems like the WaveOne Gold Glider (Dentsply Sirona), ProGlider (Dentsply Sirona) and One G (Micro-Mega, Besancon Cedex, France) have been invented. The ProGlider file has progressive tapers from 2% to over 8% along its active portion with a diameter of 0.16 mm at D0 and 0.82 mm at D16. A single ProGlider file will create a significantly larger, smoothly tapered pathway than any other dedicated multi-file system [69]. It utilizes the M-Wire technology where it is heat treated prior to machining. NiTi wire may be metallurgically improved through heat treatment pre- or post-machining. Heat treatment prior to machining results in what is commercially termed M-Wire. M-Wire has been shown to considerably increase flexibility and provide a 400% superior resistance to cyclic fatigue [71].
The first available glide path file in the market is the Pathfile system (Dentsply Sirona). It includes three instruments (13 .02, 16 .02 and 19 .02) [71]. Several brands in the market that offer rotary glide path preparation include: Micro Mega G-files (2 instruments), J. Morita EndoWave (3 instruments), FKG Scout-Race (3 instruments) and Clinician A s ChoicetX-Plorer Series (3instruments) [72].
Recently, single-file instruments have been introduced to the dental market for shaping root canal systems using a reciprocating movement with a single file technique [73]. However, this will subject the instrument to high stresses by shaping root canals with only one instrument, and therefore, they should have a good resistance to fracture [74].
The reciprocating movement has been advocated to improve the fracture resistance of endodontic instruments during canal instrumentation [75].
In this case report, biomechanical preparation was done using the Small (20/.07) followed by the Primary (25/.07) Wave One Gold rotary files (Dentsply Sirona). Eighty percent of root canals can be prepared with the Primary file alone but when the Primary WaveOne Gold file doesn’t passively progress to full length, Small file can be used as a bridge file. Though two file method is an exemption, this method is still considered safer and more efficient than other rotary instrument techniques [76].
WaveOne Gold files are built using advanced metallurgy and they are manufactured using gold heat-treatment technology. According to the manufacturer, the gold technology expands the flexibility and strength of the instrument (16,18) as well as enhancing its elasticity [76, 77]. In addition, the superior flexibility of WaveOne Gold instruments could be due to the high Af temperatures and the two-stage precise transformation behaviour which increases the flexibility property [77].
Torsional strength denotes the improved performance of an instrument to twist before fracture which is necessary while preparing constricted and narrow root canals [78]. In one study, WaveOne Gold instruments had a higher torsional resistance compared with the other systems [79]. This finding could be attributed to the WaveOne Gold instruments having a parallelogram-shaped cross-sectional design with an 850 active cutting edge with alternate one and two-point contact [16, 76]. This off-centred parallelogram-shaped cross-sectional design could augment its torsional resistance [79].
Apart from the WaveOne Gold, other files that employ reciprocating motion are the Reciproc Blue (VDW, Munich, Germany), WaveOne (Dentsply Sirona and SmartTrack (Nikinc Dental BV, Eindhoven, the Netherlands). SmartTrack is a recent reciprocating file with heat treatment after manufacturing. The heat treatment enhances the characteristics of NiTi. The manufacturer of the file claims that the file has maximum flexibility and demonstrates reduced risk of ledging and apical canal transportation. They also claim that the file has a high cyclic fatigue resistance [80]. Reciproc Blue, the new generation of single-file Reciproc files, has recently been introduced. The file is claimed to be more flexible and has an even lower fracture risk than the Reciproc file. Because of the superior temperature protocol, the Reciproc Blue file can also be prebent for improved access curved root canals [81].
Chemical disinfection was achieved using positive syringe irrigation using 2.5% of sodium hypochlorite as irrigant [25-28]. A concentration of 15% ethylenediaminetetraacetic acid (EDTA, Glyde, Dentsply Sirona) was used as a lubricant [29-31]. The use of EDTA in combination with NaOCl is advocated and may heighten the cleaning and antimicrobial effects of these solutions when compared with using them alone [82-85].
Obturation was accomplished via lateral compaction technique which is a common method for obturation [86, 87]. It can be used in many clinical conditions because it offers for predictable length control during compaction with comparable clinical treatment outcome to thermafil technique [88-90]. There is no significant statistical difference between the quality of obturation via lateral condensation and warm vertical compaction [89, 91]. Other studies concluded that the sealing ability of cold lateral compaction, warm vertical compaction and GuttaFlow system was comparable [92-94].
AH Plus (Dentsply Sirona) endodontic sealer was used in this case report. It is an epoxy resin amine-based system that comes in two tubes. The epoxide paste tube contains a diepoxide (bisphenol A diglycidyl ether) and fillers as the major ingredients, while the amine paste tube contains a primary monoamine, a secondary diamine, a disecondary diamine, silicone oil, and fillers as the major ingredients. It exhibits a working time of approximately 4 hours [95]. It offers excellent radiopacity, low shrinkage, low solubility, outstanding flow characteristics and it exhibits a significant self-adhesion to dentine [96, 97]. Saleh showed that root canal fillings with AH Plus effectively kills enterococcus faecalis in dentin tubules [98].
After cold lateral compaction, the excess gutta-percha in the chamber was seared off and vertically compacted with a heated plugger 1 mm beneath the canal orifices to enhance the coronal seal [36]. Glass Ionomer cement, GIC Fuji VII (GC Dental, Japan) was placed on top of the gutta-percha to prevent coronal microleakage [35, 37]. GIC can be used as intra-orifice barriers with good resistance to fracture in endodontically treated teeth and offers a higher sealing ability when placed at 1mm and 2mm compared to composite [99, 100].
Given the depth of many endodontic access cavities, the option of bulk-filling cavities is also important in postendodontic treatment [101]. In the present case SDR® (Dentsply Sirona) was used as a dentine replacement in bulk up to 4 mm immediately after the root canal treatment. This bulk fill composite technology has distinctive features: it is self-levelling for tremendous cavity adaptation, it allows dentists to bulk-fill up to 4 mm instead of placing and curing multiple composite layers in Class I and II restorations and it demonstrates extremely low polymerization stress [101-106]. The self-levelling consistency as well as the reduced polymerization shrinkage stress of SDR allows both optimum adaptation and adhesion to the cavity and thus enhancing coronal sealing of the root canal filling [101, 102, 107]. Another gain of this bulk-filling composite is its transparency permitting an easy retrieval of the root canal filling, e.g. in case of a subsequent post placement [101].
The clinical longevity of endodontically treated posterior teeth (molars and bicuspids) is significantly improved with coronal coverage [108-110].
In the present case report, a full-cuspal coverage direct resin composite restoration Ceram X Universal shade A2 was used. Restorations of endodontically treated teeth are designed to guard the remaining tooth from fracture, prevent reinfection of the root canal system, and to replace the missing tooth structure [111].
Conclusion
Root canals containing separated instrument fragments are highly manageable, and microsonic technique is a successful method of instrument retrieval. The pre-bending of M-access files before activation may facilitate the negotiation of severely curved canals. The Proglider and WaveOne Gold are safe, efficient in highly curved canals. Patience, technique, technology and training is fundamental to successful management of severely curved canals.
Financial support and sponsorship
None
Conflict of interest
The authors had full autonomy of investigation and there were no conceivable conflicts of interest.
Acknowledgements
The Authors wish to acknowledge the Department of Endodontics, University of the East for allowing us to conduct this case study.
Article Info
Article Type
Case ReportPublication history
Received 31 December, 2018Accepted 10 January, 2019
Published 28 January, 2019
Copyright
© 2018 Benjamin Simiyu Nyongesa. Quock. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository. All rights.DOI: 10.31487/j.ORD.2018.01.003
Author Info
Corresponding author
Benjamin Simiyu NyongesaBDS, Postgraduate Endodontic Section, College of Dentistry, University of the East, Manila, Philippines.
Figures & Tables
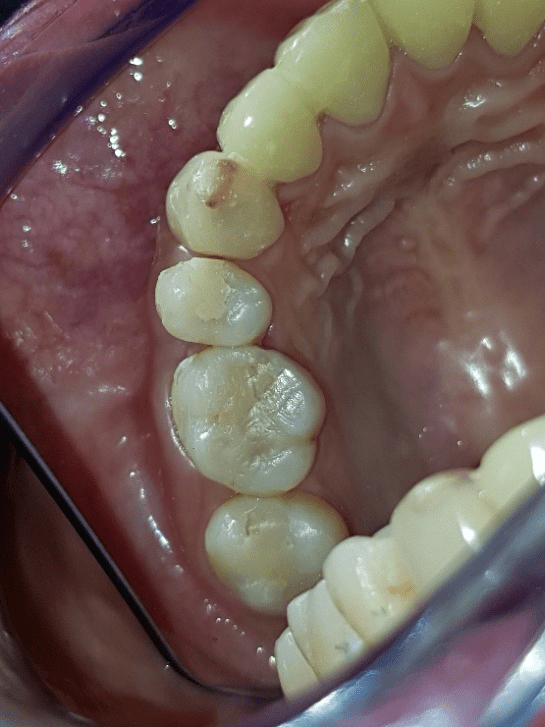

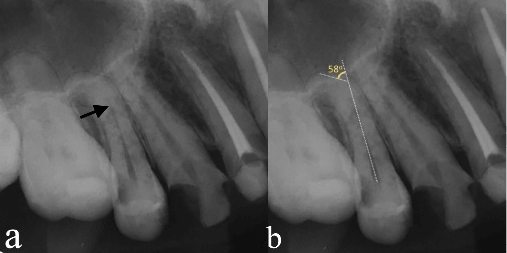
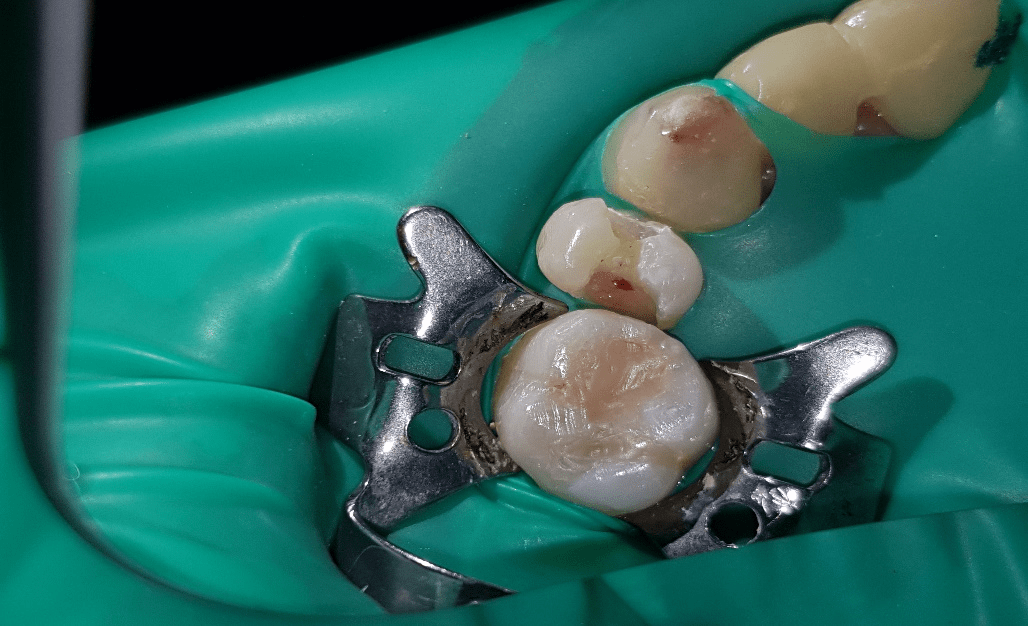
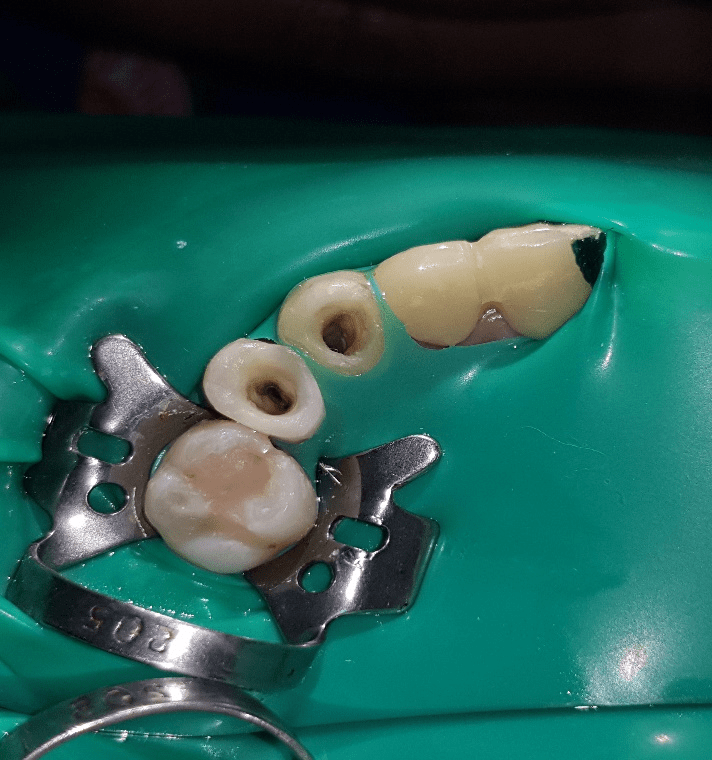
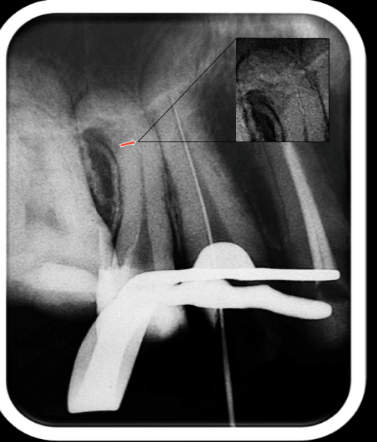
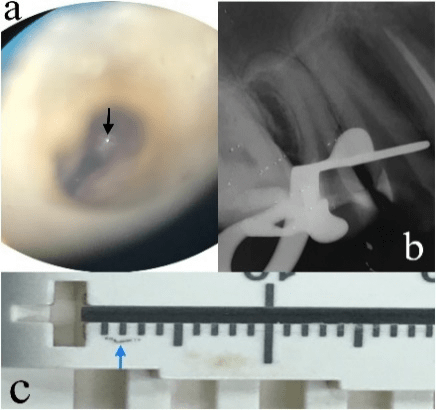
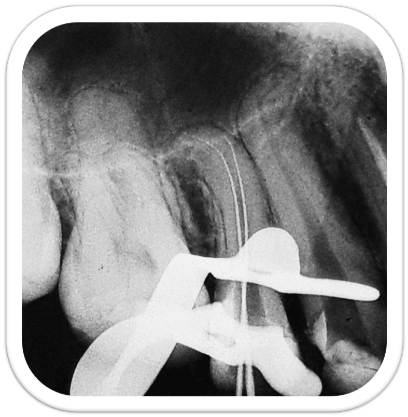
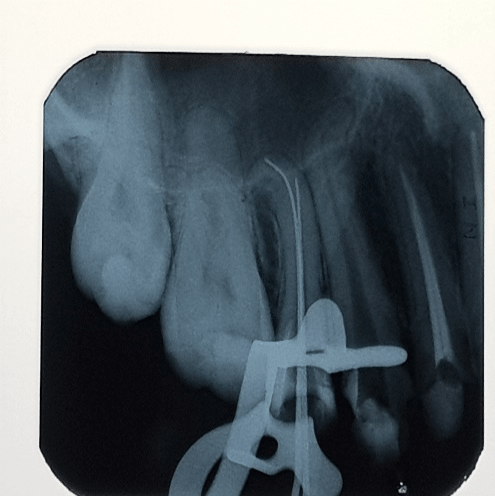
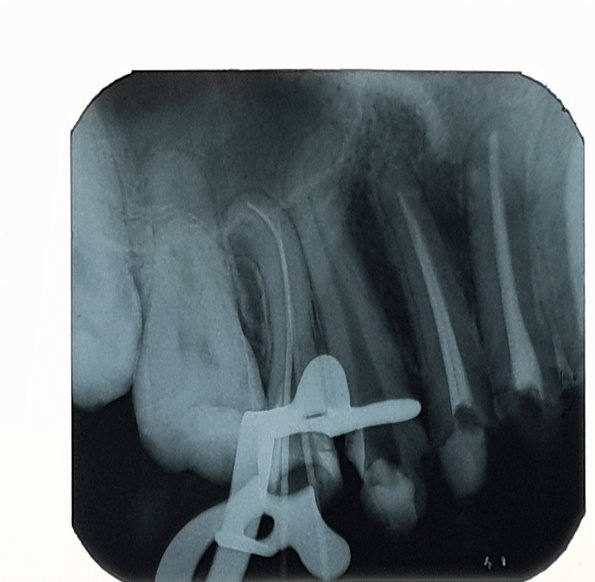
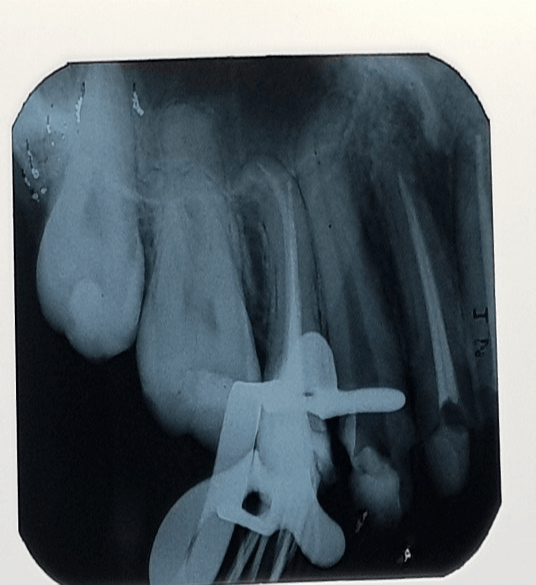

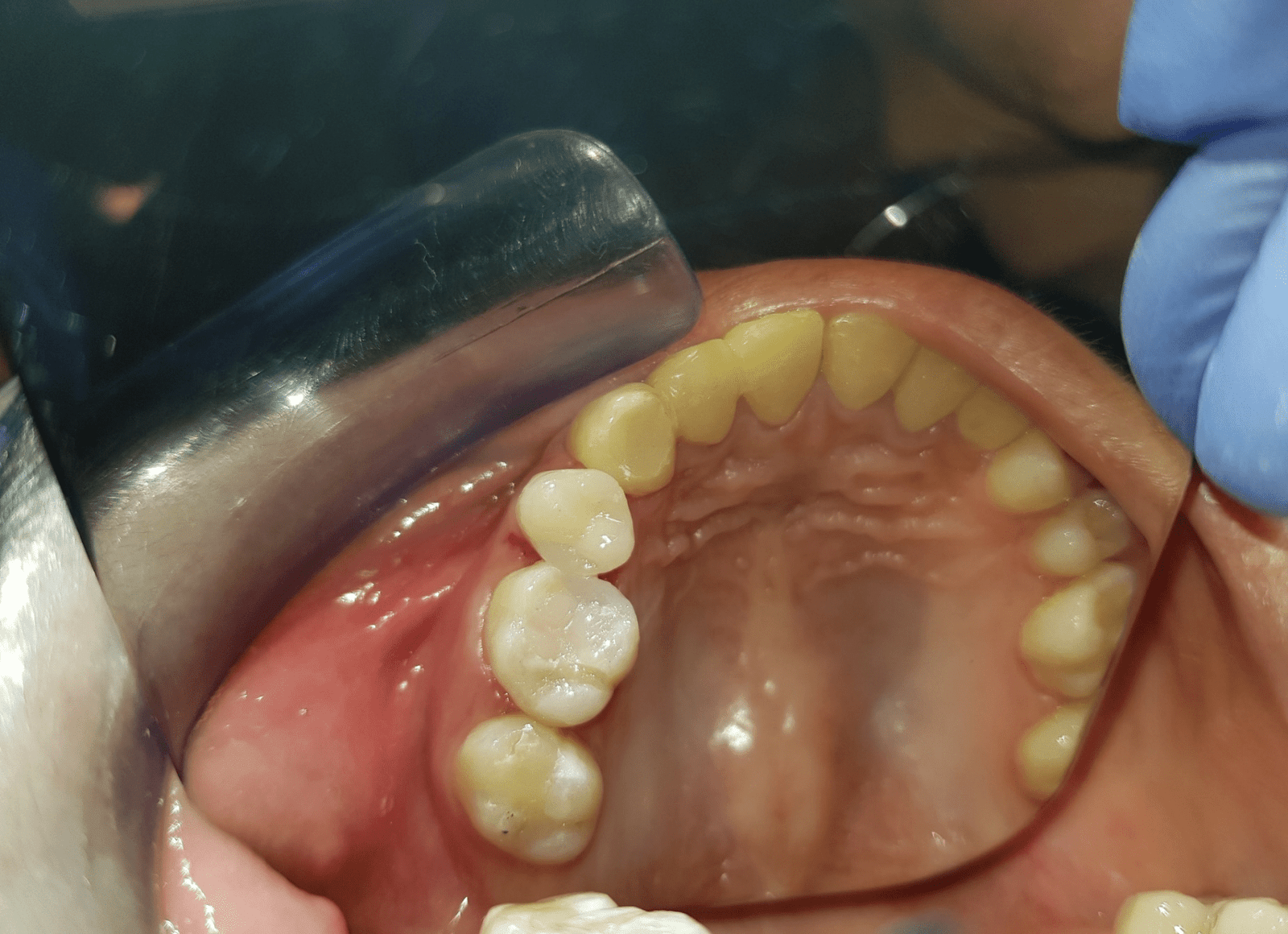

Table 1: Periodontal examination findings of tooth no. 15
|
MB |
1.5mm |
B |
1.0mm |
DB |
1.0mm |
|
MP |
1.5mm |
P |
1.0mm |
DP |
1.0mm |
Table 2: Results of diagnostic testing.
|
Diagnostic Test |
Contralateral tooth no. 25 |
Offending tooth no. 15 |
Another offending tooth no. 13 |
|
Cold Test |
1:2sec |
1sec:10sec |
2sec:14sec |
|
Percussion |
- |
+++ |
+ |
|
Mobility |
Normal |
Normal |
Normal |
|
Palpation |
- |
- |
- |
Table 3: Working length measurements of the two canals.
|
Canal |
File Size |
Working Length |
Reference Point |
|
Buccal |
06 |
18.0mm |
Buccal Cusp Tip |
|
Palatal |
06 |
20.5mm |
Palatal Cusp Tip |
References
- Seago ST, Bergeron BE, Kirkpatrick TC, Roberts MD, Roberts HW, et al. (2015) Effect of repeated simulated clinical use and sterilization on the cutting efficiency and flexibility of Hyflex CM nickel-titanium rotary files. J Endod 41: 725-728. [Crossref]
- Al-Sudani D, Grande NM, Plotino G, Pompa G, Di Carlo S, et al. Cyclic fatigue of nickel-titanium rotary instruments in a double (S-shaped) simulated curvature. J Endod 38: 987-989. [Crossref]
- Cheung GSP (2007) Instrument fracture: mechanisms, removal of fragments and clinical outcomes. Br Dent J 208: 13-13.
- Jafarzadeh H, Abbott PV (2007) Dilaceration: review of an endodontic challenge. J Endod 33: 1025-1230. [Crossref]
- West J (2006) Endodontic update 2006. J Esthet Restor Dent 18: 280-300. [Crossref]
- Berutti E, Negro AR, Lendini M, Pasqualini D (2004) Influence of manual preflaring and torque on the failure rate of ProTaper rotary instruments. J Endod 30: 228-230. [Crossref]
- Patiño PV, Biedma BM, Liébana CR, Cantatore G, Bahillo JG (2005) The influence of a manual glide path on the separation rate of NiTi rotary instruments. J Endod 31: 114-116. [Crossref]
- Shen Y, Haapasalo M, Cheung GS-P, Peng B (2009) Defects in nickel-titanium instruments after clinical use. Part 1: Relationship between observed imperfections and factors leading to such defects in a cohort study. J Endod 35: 129-132. [Crossref]
- Vorster M, van der Vyver PJ, Paleker F (2018) Influence of Glide Path Preparation on the Canal Shaping Times of WaveOne Gold in Curved Mandibular Molar Canals. J Endod 44: 853-855. [Crossref]
- Walsch H (2004) The hybrid concept of nickel-titanium rotary instrumentation. Dent Clin North Am 48: 183-202. [Crossref]
- West JD (2010) The endodontic Glidepath: “Secret to rotary safety”. Dent Today 29: 90-93. [Crossref]
- Jonker CH, Van der Vyver PJ, De Wet FA (2014) The influence of glide path preparation on the failure rate of WaveOne reciprocating instruments. SADJ 69: 266-269. [Crossref]
- Paleker F, van der Vyver PJ (2017) Glide Path Enlargement of Mandibular Molar Canals by Using K-files, the ProGlider File, and G-Files: A Comparative Study of the Preparation Times. J Endod 43: 609-612. [Crossref]
- Plotino G, Grande NM, Cotti E, Testarelli L, Gambarini G (2014) Blue treatment enhances cyclic fatigue resistance of vortex nickel-titanium rotary files. J Endod 40: 1451-1453. [Crossref]
- Topçuoğlu HS, Düzgün S, Aktı A, Topçuoğlu G (2017) Laboratory comparison of cyclic fatigue resistance of WaveOne Gold, Reciproc and WaveOne files in canals with a double curvature. Int Endod J 50: 713-717. [Crossref]
- Dentsply S. Wave One Gold [Internet]. [cited 2018 Jul 30].
- Hieawy A, Haapasalo M, Zhou H, Wang Z-J, Shen Y (2015) Phase Transformation Behavior and Resistance to Bending and Cyclic Fatigue of ProTaper Gold and ProTaper Universal Instruments. J Endod 41: 1134-1138. [Crossref]
- Grande NM, Ahmed HMA, Cohen S, Bukiet F, Plotino G (2015) Current Assessment of Reciprocation in Endodontic Preparation: A Comprehensive Review-Part I: Historic Perspectives and Current Applications. J Endod 41: 1778-1783. [Crossref]
- Plotino G, Grande NM, Testarelli L, Gambarini G (2012) Cyclic fatigue of Reciproc and WaveOne reciprocating instruments. Int Endod J 45: 614-618. [Crossref]
- Schneider SW (1971) A comparison of canal preparations in straight and curved root canals. Oral Surgery, Oral Med Oral Pathol 32: 271-275. [Crossref]
- Ruddle CJ (2004) Nonsurgical retreatment. J Endod 30: 827-845. [Crossref]
- Buchanan L (2016) Removing separated files with the Terauchi File Retrieval Kit. Roots 1 2016: 20-23.
- Madarati A, Watts DC, Qualtrough AJE (2008) A survey on the experience of UK endodontists and general dental practitioners in the management of intra-canal fractured endodontic files. Int Endod J 41: 816-816.
- Shiyakov KK, Vasileva RI (2014) Effectiveness in the curve of eight types of endosonic tips for broken instruments removal. J IMAB - Annu Proceeding 20: 595-600.
- Gomes BP, Ferraz CC, Vianna ME, Berber VB, Teixeira FB, et al. (2001) In vitro antimicrobial activity of several concentrations of sodium hypochlorite and chlorhexidine gluconate in the elimination of Enterococcus faecalis. Int Endod J 34: 424-428. [Crossref]
- Radcliffe CE, Potouridou L, Qureshi R, Habahbeh N, Qualtrough A, et al. (2004) Antimicrobial activity of varying concentrations of sodium hypochlorite on the endodontic microorganisms Actinomyces israelii, A. naeslundii, Candida albicans and Enterococcus faecalis. Int Endod J 37: 438-446. [Crossref]
- Zehnder M (2006) Root canal irrigants. J Endod 32: 389-398. [Crossref]
- Mammani IMA, Mohammod JMN, Saleh ZE (2010) Efficacy of endox endodontic system in eradication of enterococcus faecalis from infected pulp in Duhok, Kurdistan, Iraq. Rawal Med J 35: 48-50.
- Nygaard-Ostby BN (1957) Chelation in root canal therapy: ethylenediamine tetra-acetic acid for cleansing and widening of root canals. Odontol Tidskr 65: 3-11.
- Garberoglio R, Becce C (1994) Smear layer removal by root canal irrigants. A comparative scanning electron microscopic study. Oral Surg Oral Med Oral Pathol 78: 359-367. [Crossref]
- Peters OA, Boessler C, Zehnder M (2005) Effect of liquid and paste-type lubricants on torque values during simulated rotary root canal instrumentation. Int Endod J 38: 223-229. [Crossref]
- Baumgartner JC, Mader CL (1987) A scanning electron microscopic evaluation of four root canal irrigation regimens. J Endod 13: 147-157. [Crossref]
- Yamada RS, Armas A, Goldman M, Lin PS (1983) A scanning electron microscopic comparison of a high volume final flush with several irrigating solutions: Part 3. J Endod 9: 137-142. [Crossref]
- Goldman M, Goldman LB, Cavaleri R, Bogis J, Lin PS (1982) The efficacy of several endodontic irrigating solutions: a scanning electron microscopic study: Part 2. J Endod 8: 487-492. [Crossref]
- Hargreaves MK, Berman L (2016) Cohen’s Pathways of the Pulp. 11th ed. Elsevier.
- Yared GM, Dagher FB, Machtou P (1997) Influence of the removal of coronal gutta-percha on the seal of root canal obturations. J Endod 23: 146-148. [Crossref]
- Pisano DM, DiFiore PM, McClanahan SB, Lautenschlager EP, Duncan JL (1998) Intraorifice sealing of gutta-percha obturated root canals to prevent coronal microleakage. J Endod 24: 659-662. [Crossref]
- Weine F (1982) Endodontic therapy. 3rd ed. Mosby 288-386.
- Cunningham CJ, Senia ES (1992) A three-dimensional study of canal curvatures in the mesial roots of mandibular molars. J Endod 18: 294-300. [Crossref]
- Luiten DJ, Morgan LA, Baumgartner JC, Marshall JG (1995) A comparison of four instrumentation techniques on apical canal transportation. J Endod 21: 26-32. [Crossref]
- Hankins PJ, ElDeeb ME (1996) An evaluation of the canal master, balanced-force, and step-back techniques. J Endod 22: 123-130. [Crossref]
- Pettiette M, Conner D, M T (2002) Procedural errors with the use of nickel-titanium rotary instruments in undergraduate endodontics. J Endod .
- Günday M, Sazak H, Garip Y (2005) A comparative study of three different root canal curvature measurement techniques and measuring the canal access angle in curved canals. J Endod 31: 796-798. [Crossref]
- Pruett JP, Clement DJ, Carnes DL Jr (1997) Cyclic fatigue testing of nickel-titanium endodontic instruments. J Endod 23: 77-85. [Crossref]
- Schafer E, Diez C, Hoppe W, Tepel J (2002) Roentgenographic Investigation of Frequency and Degree of Canal Curvatures in Human Permanent Teeth. J Endod 28: 211-216. [Crossref]
- Sonntag D, Stachniss-Carp S, Stachniss V (2005) Determination of root canal curvatures before and after canal preparation (part 1): a literature review. Aust Endod J 31: 89-93. [Crossref]
- Lin C, Xu L, Chen Y, Liang Y, Chen X, et al. (2015) A statistical model for predicting the retrieval rate of separated instruments and clinical decision-making. J Dent Sci 10: 423-430. [Crossref]
- Hargreaves MK, Berman L (2016) Cohen’s Pathways of the Pulp. 11th ed. Elsevier 2016: 224-233.
- Sattapan B, Nervo G, Palamara J, Messer H (2000) Defects in Rotary Nickel-Titanium Files After Clinical Use. J Endod 26: 161-165. [Crossref]
- Setzer FC, Böhme CP (2013) Influence of Combined Cyclic Fatigue and Torsional Stress on the Fracture Point of Nickel-Titanium Rotary Instruments. J Endod 39: 133-137. [Crossref]
- Ullmann C, Peters OA (2005) Effect of Cyclic Fatigue on Static Fracture Loads in ProTaper Nickel-Titanium Rotary Instruments. J Endod 31: 183-186. [Crossref]
- Ferreira F, Adeodato C, Barbosa I, Aboud L, Scelza P, et al. (2017) Movement kinematics and cyclic fatigue of NiTi rotary instruments: a systematic review. Int Endod J 50: 143-152. [Crossref]
- Duke F, Shen Y, Zhou H, Ruse ND, Wang Z, et al. (2015) Cyclic Fatigue of ProFile Vortex and Vortex Blue Nickel-Titanium Files in Single and Double Curvatures. J Endod 41: 1686-1890. [Crossref]
- Parashos P, Gordon I, Messer HH (2004) Factors Influencing Defects of Rotary Nickel-Titanium Endodontic Instruments After Clinical Use. J Endod 30: 722-725. [Crossref]
- Kramkowski TR, Bahcall J (2009) An In Vitro Comparison of Torsional Stress and Cyclic Fatigue Resistance of ProFile GT and ProFile GT Series X Rotary Nickel-Titanium Files. J Endod 35: 404-407. [Crossref]
- Alapati SB, Brantley WA, Svec TA, Powers JM, Nusstein JM, et al. (2005) SEM observations of nickel-titanium rotary endodontic instruments that fractured during clinical Use. J Endod 31: 40-43. [Crossref]
- Al-Fouzan KS (2003) Incidence of rotary ProFile instrument fracture and the potential for bypassing in vivo. Int Endod J 36: 864-867. [Crossref]
- Ramirez-Salomon M, Soler-Bientz R, de la Garza-González R, Palacios-Garza CM (1997) Incidence of Lightspeed separation and the potential for bypassing. J Endod 23: 586-587. [Crossref]
- Schäfer E, Schulz-Bongert U, Tulus G (2004) Comparison of Hand Stainless Steel and Nickel Titanium Rotary Instrumentation: A Clinical Study. J Endod 30: 432-435. [Crossref]
- Spili P, Parashos P, Messer HH (2005) The impact of instrument fracture on outcome of endodontic treatment. J Endod 31: 845-850. [Crossref]
- Tordai B, Schreindorfer K, Lempel E, Krajczár K (2018) Factors affecting ultrasonic removal of separated endodontic instruments: A retrospective clinical study. Quintessence Int 49: 257-266. [Crossref]
- Madarati AA, Hunter MJ, Dummer PMH (2013) Management of Intracanal Separated Instruments. J Endod 39: 569-581. [Crossref]
- Cujé J, Bargholz C, Hülsmann M (2010) The outcome of retained instrument removal in a specialist practice. Int Endod J 43: 545-554. [Crossref]
- Ward JR, Parashos P, Messer HH (2003) Evaluation of an Ultrasonic Technique to Remove Fractured Rotary Nickel-Titanium Endodontic Instruments from Root Canals: Clinical Cases. J Endod 29: 764-767. [Crossref]
- Alomairy KH (2009) Evaluating Two Techniques on Removal of Fractured Rotary Nickel-Titanium Endodontic Instruments from Root Canals: An In Vitro Study. J Endod 35: 559-562. [Crossref]
- Nagai O, Tani N, Kayaba Y, Kodama S, Osada T (1986) Ultrasonic removal of broken instruments in root canals. Int Endod J 19: 298-304. [Crossref]
- Terauchi Y, O’Leary L, Kikuchi I, Asanagi M, Yoshioka T, et al. (2007) Evaluation of the Efficiency of a New File Removal System in Comparison With Two Conventional Systems. J Endod 33: 585-588. [Crossref]
- Young G, Parashos P, Messer HH (2007) The principles of techniques for cleaning root canals. Aust Dent J 52: S52–S63. [Crossref]
- Ruddle CJ, Machtou P, West JD (2014) Endodontic canal preparation: innovations in glide path management and shaping canals. Dent Today 33: 118-123. [Crossref]
- Cassim I, van der Vyver PJ (2013) The importance of glide path preparation in endodontics: a consideration of instruments and literature. SADJ 68: 324-327. [Crossref]
- Berutti E, Cantatore G, Castellucci A, Chiandussi G, Pera F, et al. (2009) Use of nickel-titanium rotary PathFile to create the glide path: comparison with manual preflaring in simulated root canals. J Endod 35: 408-412. [Crossref]
- Capar ID, Kaval ME, Ertas H, Sen BH (2015) Comparison of the Cyclic Fatigue Resistance of 5 Different Rotary Pathfinding Instruments Made of Conventional Nickel-Titanium Wire, M-wire, and Controlled Memory Wire. J Endod 41: 535-538. [Crossref]
- Bürklein S, Benten S, Schäfer E (2013) Shaping ability of different single-file systems in severely curved root canals of extracted teeth. Int Endod J 46: 590-597. [Crossref]
- Kim HC, Kwak SW, Cheung GS P, Ko DH, Chung SM, et al. (2012) Cyclic Fatigue and Torsional Resistance of Two New Nickel-Titanium Instruments Used in Reciprocation Motion: Reciproc Versus WaveOne. J Endod 38: 541-544. [Crossref]
- De-Deus G, Moreira EJL, Lopes HP, Elias CN (2010) Extended cyclic fatigue life of F2 ProTaper instruments used in reciprocating movement. Int Endod J 43: 1063-1068. [Crossref]
- Webber J (2015) Shaping canals with confidence: WaveOne Gold single-file recipocating system. Roots 1: 34-40.
- Özyürek T (2016) Cyclic Fatigue Resistance of Reciproc, WaveOne, and WaveOne Gold Nickel-Titanium Instruments. J Endod 42: 1536-1539. [Crossref]
- Ninan E, Berzins DW (2013) Torsion and Bending Properties of Shape Memory and Superelastic Nickel-Titanium Rotary Instruments. J Endod 39: 101-104. [Crossref]
- Elsaka SE, Elnaghy AM, Badr AE (2017) Torsional and bending resistance of WaveOne Gold, Reciproc and Twisted File Adaptive instruments. Int Endod J 50: 1077-1183. [Crossref]
- NikincDental. SmartTrack [Internet]. [cited 2018 Aug 8].
- VDW. RECIPROC blue – A great file. Even better. [Internet]. [cited 2018 Aug 9].
- Stewart GG (1998) A scanning electron microscopic study of the cleansing effectiveness of three irrigating modalities on the tubular structure of dentin. J Endod 24: 485-486. [Crossref]
- Tatsuta CT, Morgan LA, Baumgartner JC, Adey JD (1999) Effect of calcium hydroxide and four irrigation regimens on instrumented and uninstrumented canal wall topography. J Endod 25: 93-98. [Crossref]
- Lim TS, Wee TY, Choi MY, Koh WC, Sae-Lim V (2003) Light and scanning electron microscopic evaluation of Glyde File Prep in smear layer removal. Int Endod J 36: 336-343. [Crossref]
- Bystrom A, Sundqvist G (1985) The antibacterial action of sodium hypochlorite and EDTA in 60 cases of endodontic therapy. Int Endod J 18: 35-40. [Crossref]
- Hargreaves MK, Berman L (2016) Cohen’s Pathways of th ePulp. 11th ed. Elsevier 2016: 302-304.
- Cailleteau JG, Mullaney TP (1997) Prevalence of teaching apical patency and various instrumentation and obturation techniques in united states dental schools. J Endod 23: 394-396. [Crossref]
- Mattigatti S, RR M, Chopade R, Grag V (2012) Unusual canal morphology in all mandibular incisors in a single patient. Int J Dent Case Reports 2: 72-76.
- Peng L, Ye L, Tan H, Zhou X (2007) Outcome of Root Canal Obturation by Warm Gutta-Percha versus Cold Lateral Condensation: A Meta-analysis. J Endod 33: 106-109. [Crossref]
- Chu CH, Lo EC, Cheung GS (2005) Outcome of root canal treatment using Thermafil and cold lateral condensation filling techniques. Int Endod J 38: 179-185. [Crossref]
- Aqrabawi JA (2006) Outcome of endodontic treatment of teeth filled using lateral condensation versus vertical compaction (Schilder’s technique). J Contemp Dent Pract 7: 17-24. [Crossref]
- Aminsobhani M, Ghorbanzadeh A, Bolhari B, Shokouhinejad N, Ghabraei S, et al. (2010) Coronal microleakage in root canals obturated with lateral compaction, warm vertical compaction and guttaflow system. Iran Endod J 5: 83-87. [Crossref]
- Olczak K, Pawlicka H (2012) Evaluation of the sealing ability of two root canal obturation techniques by using a glucose leakage test. J Stomatol 65: 863-877.
- Varun K, Harpreet S, Rajinder B, Samrity P (2013) Qualitative and quantitative comparative evaluation of sealing ability of guttaflow, thermoplasticized gutta percha and lateral compaction for root canal obturation: a cohort, controlled, ex-vivo study. Oral Health Dent Manag 12: 155-161. [Crossref]
- Hargreaves MK, Berman L (2016) Obturation of the cleaned and shaped root canal system. Cohen’s Pathways of the Pulp. 11th ed 2016: 292-293.
- 96.Sirona D. AH Plus ® [Internet]. [cited 2018 Aug 15].
- Gogos C, Economides N, Stavrianos C, Kolokouris I, Kokorikos I (2004) Adhesion of a New Methacrylate Resin-Based Sealer to Human Dentin. J Endod 30: 238-240. [Crossref]
- Saleh IM, Ruyter IE, Haapasalo M, Ørstavik D (2004) Survival of Enterococcus faecalis in infected dentinal tubules after root canal filling with different root canal sealers in vitro. Int Endod J 7: 193-198. [Crossref]
- Aboobaker S, Nair BG, Gopal R, Jituri S, Veetil FR (2015) Effect of intra-orifice barriers on the fracture resistance of endodontically treated teeth - an ex-vivo study. J Clin Diagn Res 9: 17-20. [Crossref]
- Salim B, Hassan N (2015) Effect of different intra-orifice barriers in endodontically treated teeth obturated with gutta-percha. IAJD.
- Van Ende A, De Munck J, Van Landuyt K, Van Meerbeek B (2016) Effect of Bulk-filling on the Bonding Efficacy in Occlusal Class I Cavities. J Adhes Dent 18: 119-124. [Crossref]
- Kumagai RY, Zeidan LC, Rodrigues JA, Reis AF, Roulet JF (2015) Bond Strength of a Flowable Bulk-fill Resin Composite in Class II MOD Cavities. J Adhes Dent 17: 427-432. [Crossref]
- Sirona D. SDR® Posterior Bulk Fill Flowable Base Study and case compilation.
- Rosatto CMP, Bicalho AA, Veríssimo C, Bragança GF, Rodrigues MP, et al. (2015) Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J Dent 43: 1519-1528.
- Ilie N, Hickel R (2011) Investigations on a methacrylate-based flowable composite based on the SDRTM technology. Dent Mater 27: 348-355. [Crossref]
- van Dijken JWV, Pallesen U (2016) Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J Dent 51: 29-35. [Crossref]
- Scotti N, Alovisi M, Berutti E, Comba A, Gambino A, et al. (2014) Microleakage at enamel and dentin margins with a bulk fills flowable resin. Eur J Dent 8: 1. [Crossref]
- Sorensen JA, Martinoff JT (1984) Intracoronal reinforcement and coronal coverage: A study of endodontically treated teeth. J Prosthet Dent 51: 780-784. [Crossref]
- Aquilino SA, Caplan DJ (2002) Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 87: 256-263. [Crossref]
- Nagasiri R, Chitmongkolsuk S (2005) Long-term survival of endodontically treated molars without crown coverage: A retrospective cohort study. J Prosthet Dent 93: 164-170. [Crossref]
- Hargreaves MK, Berman L (2016) Restoration of the endodontically Treated tooth. Cohen’s Pathways of the Pulp. 11th ed 2016: 8821-8822.
