Malignant Transformation of Post-Nephrectomy Enterocutaneous Fistula: A Review of Literature
A B S T R A C T
Background: Enterocutaneous fistula is an aberrant epithelialized communication between the bowel and the skin occurring mostly as a complication of abdominal surgery. Enterocutaneous fistula may present as chronically discharging sinus and like any other chronic non healing wound, malignant transformation has rarely been reported in such gastrointestinal fistula. Herein we report an additional case of malignant transformation of enterocutaneous fistula leading to duodenal mass.
Case Presentation: A 50-year diabetic gentleman presented with a persistent draining sinus from his surgical site of right nephrectomy for 6 months with friable growth over the sinus opening which sheds off spontaneously to reappear again after a period. Investigations showed duodenal growth communicating to the right renal fossa and further to the skin surface in the lumbar region. Exploratory laparotomy was performed where a circumferential mass was noted in the second part of duodenum with perforation in the posterior wall. The perforation was seen to communicate with skin via fistulous tract. Postoperative biopsy of duodenal mass confirmed it to be well differentiated squamous cell carcinoma with transmural infiltration.
Conclusion: When perirenal or retroperitoneal inflammation takes place, second part of the duodenum becomes involved and the absence of a protective peritoneal barrier between the two, along with the relative immobility of the duodenum, accounts for the internal drainage and fistula formation which occurs. Persistent enterocutaneous fistula after nephrectomy causes long standing pus discharge and malnourishment affecting the overall health of these patients. Chronic inflammation is known to be a risk factor for development of squamous cell carcinoma. Two previous cases of malignant transformation of post nephrectomy colocutaneous fistula have been reported. However, this case is unique as no prior reporting of malignant transformation of duodeno-cutaneous fistula was found in literature.
Keywords
Case report, enterocutaneous fistula, post nephrectomy, gastrointestinal malignancy, duodeno-cutaneous fistula, malignant transformation
Background
Fistula is defined as an epithelium lined connection between two epithelialized organs. Enterocutaneous fistula is a similar abnormal tract connecting the intestine to skin. While most (75-85%) occur after abdominal surgery, 15-25% fistulas develop spontaneously [1]. Such patients are usually malnourished, cachexic presenting in sepsis with poor prognosis. Management includes skin care, nutrition, infection control and anatomical correction with surgery [1]. Ongoing chronic inflammation in enterocutaneous fistula predisposes it for malignant transformation, though rarely seen. Two cases of malignant GI fistula have been reported in literature till now. Herein we report a case of enterocutaneous fistula after nephrectomy complicating into squamous cell carcinoma.
Case Report
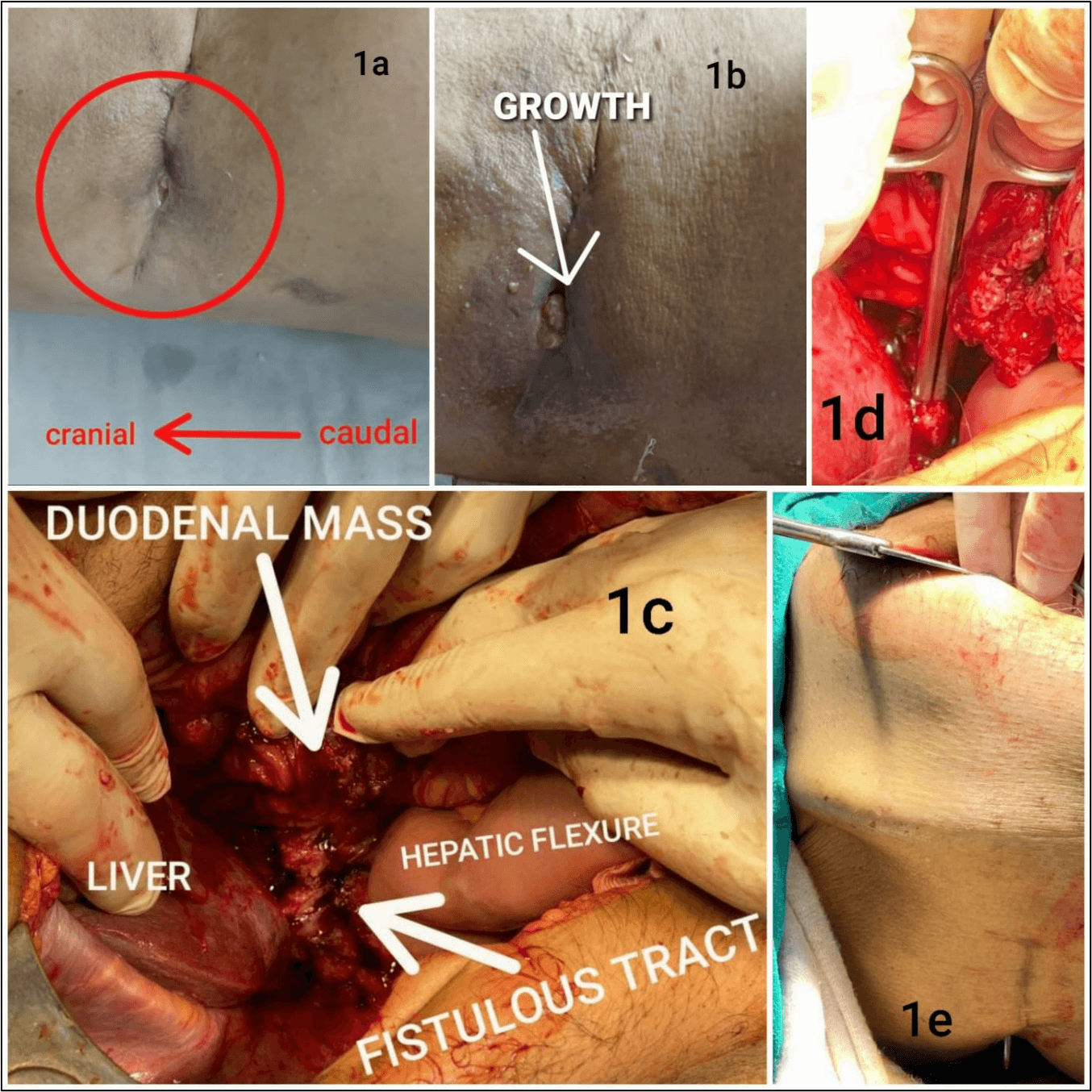
A diabetic gentleman in his 50s, controlled on regular medications was a case of status post nephrectomy complicated with enterocutaneous fistula. He had undergone right nephrectomy with iatrogenic colonic injury 4 years back for non-functioning kidney with pyonephrosis. In the immediate post op period enterocutaneous fistula developed at drain site with feculent output. He was conservatively managed for one month and discharged after spontaneous closure of fistula. Now he reported persistent discharging sinus from his surgical scar site in the right flank for the past 6 months. It was associated with friable growth over the sinus opening which sheds off spontaneously to reappear again after a period. Figures 1a & 1b show sinus with friable growth over it.
Figure 1: a) Sinus opening over right flank scar. b) Growth over the enterocutaneous fistula. c) Intraoperative picture showing duodenal mass with enterocutaneous fistula. d) Probe inserted into enteral opening of fistulous tract. e) Probe exiting from skin over scar site.
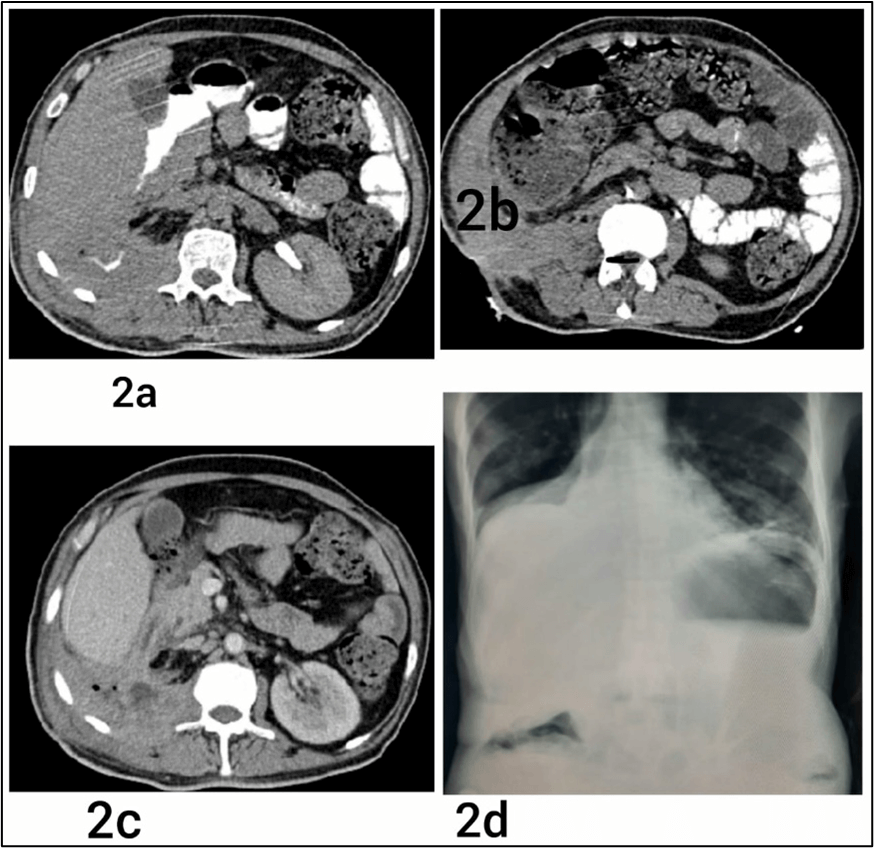
Blood investigations revealed a raised total leukocyte count and severe anemia. Ultrasound of the abdomen revealed a collection of ~2.2cm × 1.7 cm in right renal fossa communicating with sinus in the right flank region with a width of 9.1 mm. The patient was managed conservatively with intravenous antibiotics and regular dressing of the wound. The patient developed new onset infrequent episodes of malena and progressive loss of appetite. Subsequent contrast enhanced computed tomography scan revealed a heterogeneously enhancing collection in right renal fossa communicating with skin surface in lumbar region and D2 which showed heterogeneously enhancing, irregular, circumferential mural thickening of ~11mm in maximum thickness as seen in (Figure 2). The patient further underwent upper gastrointestinal endoscopy which showed large circumferential ulceroproliferative growth occluding the lumen in D2. Biopsy taken from growth showed atypical squamous cell nests with a possibility of squamous cell carcinoma.
Figure 2: a) CECT showing enterocutaneous fistula. b) CECT showing spillage of oral contrast onto skin via fistulous opening. c) Enterocutaneous fistula as visible on CT. d) Abdominal X-Ray showing enterocutaneous fistula.
The patient was being optimized for elective resection when he developed signs of acute intestinal obstruction for which emergency exploratory laparotomy was performed. Intraoperatively, liver, omentum and small intestines were seen to be adhered together in the right hypochondrium. A circumferential mass was noted in the second part of duodenum with perforation in the posterior wall. The perforation was seen to communicate with skin via fistulous tract as seen in (Figures 1c-1e).
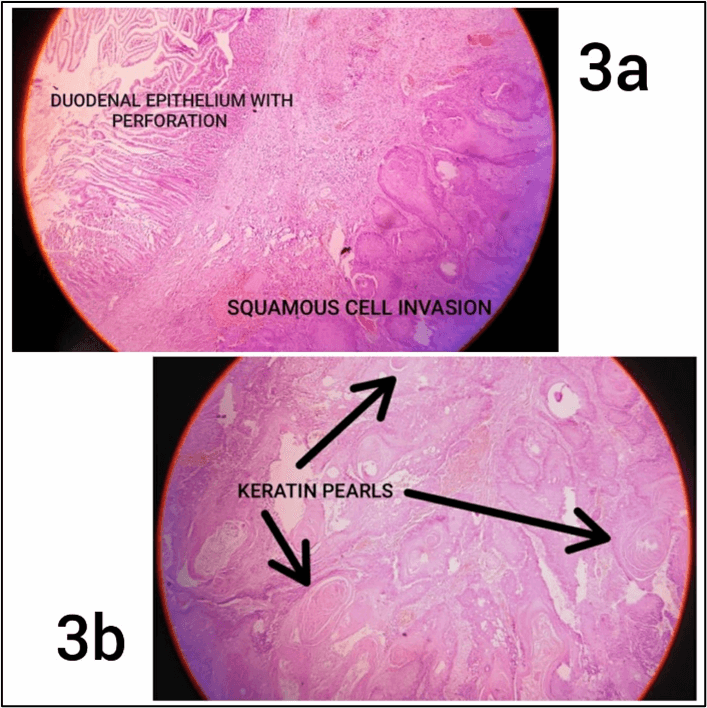
In view of the general condition of the patient, damage control measures were taken with pyloric exclusion with drainage and feeding jejunostomy. Postoperatively, the patient was managed in intensive care with mechanical ventilation and inotropic support. However, the patient expired on the fourth postoperative day due to ongoing sepsis with septic shock and subsequent multiple organ dysfunction. Postoperative biopsy report of duodenal mass confirmed it to be well differentiated squamous cell carcinoma with transmural infiltration as shown in (Figure 3).
Figure 3: a) Histopathological image of duodenal perforation with transmural infiltration of squamous cell. b) Duodenal mass biopsy showing squamous differentiation with keratin pearl.
Discussion
The anterior pararenal space of the retroperitoneum contains the duodenum, pancreas, and the ascending and descending colon. There is free communication within this space, and towards the mesenteries along the vessels [4]. Retroperitoneal infection is usually caused by secondary complications such as inflammation, damage, or perforation of adjacent organs in the retroperitoneal space. Pathogenic bacteria invade the retroperitoneal space through retroperitoneal and interstitial organs, peripheral tissue, and the blood. Initially manifested by the presence of lower back pain, this disease spreads easily and is often misdiagnosed. Because of the loose space and poor blood flow in the retroperitoneal tissues, an infection often spreads easily in the space to form abscesses early on. Retroperitoneal infections are persistent and difficult to treat which further spread to surrounding structures, resulting in retroperitoneal fistulae [5].
The second portion of the duodenum lies in the retroperitoneum with its posterior aspect close to the medial portion of the kidney and renal pelvis. When perirenal or retroperitoneal inflammation takes place, this portion of the duodenum becomes involved and the absence of a protective peritoneal barrier between the two, along with the relative immobility of the duodenum, accounts for the internal drainage and fistula formation which occurs [6].
Surgery is the most common cause of entero-cutaneous fistula. While most enterocutaneous fistulas heal spontaneously, persistent entero-cutaneous fistula may be due to foreign body, radiation, infection, inflammation, epithelization, neoplasm and distal obstruction [3]. Squamous cell carcinoma is known to develop in long standing ulcers, scars, wounds, sinuses, and fistulas. The time between the inciting inflammatory event and the development of cancer is typically 25-40 years but can occur as early as 1-7 years in the immunocompromised population, with a latency period that is inversely proportional to the patient's age at the time of injury [7]. Referring to our case since the injury occurred later in life but the patient had compromised immunity due to diabetes, thereby leading to an early inception of cancer.
Tissue injury during inflammation results in cellular proliferation and regeneration which would normally subside once the offending agent is removed or once the tissue is satisfactorily repaired. If there is failure in eliminating the inciting agent, proliferation continues in a microenvironment rich in cytokines, growth factors, and accumulating breakdown products of cellular function in a prolonged attempt to repair, often resulting in an accumulation of genetic errors and further inappropriate proliferation. Such an inflammatory response is well documented in the development of gastrointestinal (GI) cancer, be it gastric cancer in H. pylori infection or colorectal cancer in inflammatory bowel disease [7].
Cancer development can be prevented in this setting by early removal of chronic wounds or ulcerations and skin grafting to the area. Successful elimination of chronic inflammation in other organ systems could have a preventive effect, though far more complicated than treating visible external wounds. In all similar cases of malignant transformation of enterocutaneous fistula reported till now showed persistent GI fistula after nephrectomy. These have been summarized in (Table 1). Long standing pus discharge and malnourishment affected the overall health of these patients. Both were managed with supportive care initially followed by surgical resection of fistulous tract and adhered structures.
Table
1:
|
AUTHOR |
Yueh-Tsung Lee et al. [8] |
Monisha G et al. [9] |
|
|
PUBLICATION YEAR |
2005 |
2020 |
|
|
AGE AT PRESENTATION |
60 years |
29 years |
|
|
GENDER |
Female |
Male |
|
|
PRESENTATION |
Generalized weakness, anorexia with fever
and chills for 2 weeks. She got two fistulous openings with intermittent
fecal discharge on her left flank scar. |
Long standing intermittent pus and
feculent discharge from fistulous tract opening over left flank at the drain
site scar. |
|
|
PREVIOUS SURGERY AND ITS INDICATION |
Left nephrectomy for left renal stones at
30 years age |
Left nephrectomy for unknown reasons at
10 years age |
|
|
SITE OF FISTULA AND INTRAOPERATIVE
FINDING |
Colo-cutaneous fistula at splenic flexure
with lower pole of the spleen adhered and irregular soft tissue beside the
region. Partial wall of the jejunum, 10 cm distal to Treitz’s ligament was
also adhered. |
Colo-cutaneous fistula |
|
|
OPERATIVE PROCEDURE |
En bloc resection with splenectomy,
segmental resection of colon with primary anastomosis and wedge resection of
jejunum were performed. |
Excision of fistulous tract, with primary
closure of descending colon site of fistula. |
|
|
OUTCOME |
Postoperative course was grossly smooth
and was being followed up at the outpatient department. |
Postoperative period was uneventful.
Colonoscopy done 2 weeks later was normal. Patient remained asymptomatic and
was in regular follow-up till 6 months post surgery. Then he died due to
sepsis. |
|
|
HISTOPATHOLOGICAL ANALYSIS |
The pathologist reported moderately
differentiated squamous cell carcinoma with the tumor cells arising from the
fistulas accompanied by spleen and colon invasion. |
Histopathology revealed a moderately differentiated
squamous cell carcinoma. |
This case is unique as the microscopic photographs revealed the origination of tumor cells from the epithelium of the fistulous tract. It is our speculation that the duodenal fistula occurred as a result of chronic inflammation which further underwent malignant transformation.
Conclusion
Enterocutaneous fistula is a common entity encountered in surgery. However, development of malignancy within such a fistula is rarely reported. All persistent GI fistula should be accurately evaluated and treated aggressively to eliminate chronic inflammation and prevent malignant transformation.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Written informed consent was obtained from the patient's relative for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of Data and Materials
Not applicable.
Competing Interests
None.
Funding
None.
Author Contributions
All authors listed have significantly contributed to the investigation, development and writing of this article.
Acknowledgements
Not applicable.
Additional Information
An additional file shows CARE checklist in more detail (Additional File 1) is included in the manuscript file. This case report has been reported in line with the CARE 2020 Guideline [10].
Abbreviations
CECT: Contrast Enhanced Computed Tomography
CT: Computed Tomography
cm: Centimeter
D2: Second Part of Duodenum
GI: Gastrointestinal
H. pylori: Helicobacter pylori
mm: Millimeter
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Fri 15, Mar 2024Accepted: Tue 16, Apr 2024
Published: Tue 21, May 2024
Copyright
© 2023 Srishti Bhowmik. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2024.02.01
Author Info
Srishti Bhowmik Anurag Mishra Chandra Bhushan Singh Sarmista Roy Vibha Singh
Corresponding Author
Srishti BhowmikPostgraduate Resident, Department of Surgery, Maulana Azad Medical College, New Delhi, India
Figures & Tables
Table
1:
|
AUTHOR |
Yueh-Tsung Lee et al. [8] |
Monisha G et al. [9] |
|
|
PUBLICATION YEAR |
2005 |
2020 |
|
|
AGE AT PRESENTATION |
60 years |
29 years |
|
|
GENDER |
Female |
Male |
|
|
PRESENTATION |
Generalized weakness, anorexia with fever
and chills for 2 weeks. She got two fistulous openings with intermittent
fecal discharge on her left flank scar. |
Long standing intermittent pus and
feculent discharge from fistulous tract opening over left flank at the drain
site scar. |
|
|
PREVIOUS SURGERY AND ITS INDICATION |
Left nephrectomy for left renal stones at
30 years age |
Left nephrectomy for unknown reasons at
10 years age |
|
|
SITE OF FISTULA AND INTRAOPERATIVE
FINDING |
Colo-cutaneous fistula at splenic flexure
with lower pole of the spleen adhered and irregular soft tissue beside the
region. Partial wall of the jejunum, 10 cm distal to Treitz’s ligament was
also adhered. |
Colo-cutaneous fistula |
|
|
OPERATIVE PROCEDURE |
En bloc resection with splenectomy,
segmental resection of colon with primary anastomosis and wedge resection of
jejunum were performed. |
Excision of fistulous tract, with primary
closure of descending colon site of fistula. |
|
|
OUTCOME |
Postoperative course was grossly smooth
and was being followed up at the outpatient department. |
Postoperative period was uneventful.
Colonoscopy done 2 weeks later was normal. Patient remained asymptomatic and
was in regular follow-up till 6 months post surgery. Then he died due to
sepsis. |
|
|
HISTOPATHOLOGICAL ANALYSIS |
The pathologist reported moderately
differentiated squamous cell carcinoma with the tumor cells arising from the
fistulas accompanied by spleen and colon invasion. |
Histopathology revealed a moderately differentiated
squamous cell carcinoma. |
References
1. Berry SM, Fischer
JE (1996) Classification and pathophysiology of enterocutaneous fistulas. Surg
Clin North Am 76: 1009-1018. [Crossref]
2. Rodney K, Maxted
WC, Pahira JJ (1983) Pyeloduodenal fistula. Urology. 22: 536-539. [Crossref]
3. Jackson L, Evers BM
(2006) Chronic inflammation and pathogenesis of GI and pancreatic cancers. Cancer
Treat Res 130: 39-65. [Crossref]
4. Lin W, Watts K,
Aboumohamed A (2018) Renoalimentary fistula: Case report of a renoduodenal
fistula and systematic literature review. Urol Case Rep 18: 41-43. [Crossref]
5. Coffin A, Boulay
Coletta I, Sebbag Sfez D, Zins M (2015) Radioanatomy of the retroperitoneal
space. Diagn Interv Imaging 96: 171-186. [Crossref]
6. Li Z, Tang Y, Wang
P, Ren J (2021) Diagnosis and Treatment of Retroperitoneal Infection. Surg
Infect (Larchmt) 22: 477-484. [Crossref]
7. Gribovskaja Rupp I,
Melton GB (2016) Enterocutaneous Fistula: Proven Strategies and Updates. Clin
Colon Rectal Surg 29: 130-137. [Crossref]
8. Lee YT, Hsu SD, Kuo
CL, Chou DA, Lin MS, et al. (2005) Squamous cell carcinoma arising from long
standing colocutaneous fistula: a case report. World J Gastroenterol 11:
5251-5253. [Crossref]
9. Monisha G, Manikanta KS (2020) A Rare Case of Squamous Cell CA Arising from Drain Site Enterocutaneous Fistula- A Case Report. Clin Surg 5: 2731.
10. Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan (2020) The SCARE 2020 Guideline: Updating Consensus Surgical Case Report (SCARE) Guidelines. Int J Surg 84: 226-230. [Crossref]
