Iliopsoas Abscess as the First Clinical Manifestation of Crohn’s Disease - A Rare Case Report and Literature Review
A B S T R A C T
Objective: Iliopsoas abscess is a rare complication of fistulizing Crohn’s disease, which is difficult to diagnose and manage. We report this case to alert clinicians to the diagnosis and management of this unusual association.
Case presentation: A 31-year-old male who presented with right groin pain, and hip pain due to an iliopsoas abscess. He was found to have iliopsoas fistula and underlying Crohn’s disease. The right iliopsoas abscess was managed with CT guided percutaneous drainage and pigtail catheter placement and intravenous antibiotics. The patient was started on mesalamine and prednisone. A month later, the patient became symptomatic again and a duodenocolic fistula was found. A laparoscopic extended right hemicolectomy with both fistulas takes-down, end ileostomy and mucus fistula were performed. Pathology revealed chronic active Crohn’s ileocolitis. His ileostomy was reversed three months later. The patient recovered uneventfully and was doing well after six-month follow-up.
Conclusions: Iliopsoas abscess can be a rare presentation of Crohn’s disease. Evaluation with CT imaging, and initial management with drainage and antibiotics are recommended. Surgical intervention should be considered early for impending arthritis.
Keywords
Iliopsoas abscess, crohn’s disease, percutaneous drainage, fistula, surgical management
Introduction
Crohn’s Disease (CD) is characterized by chronic inflammation of gastrointestinal tract (GIT). It can involve any part of the GIT from mouth to anus, but in the majority of cases it mainly affects the terminal ileum and/or the colon. A usual presentation is abdominal pain, diarrhea, with or without bleeding, weight loss and/or perianal disease. It is very rare for a patient presented with iliopsoas abscess (IPA) as a first presentation of underlying CD. In some cases, the identification of a fistula and its correlation with the clinical symptoms may be very difficult. There are only a few reports in the literature of psoas abscess and fistulae in patients with CD. We reported a 31 years old male patient with right iliopsoas abscess as the first symptoms of undiagnosed CD.
Case Description
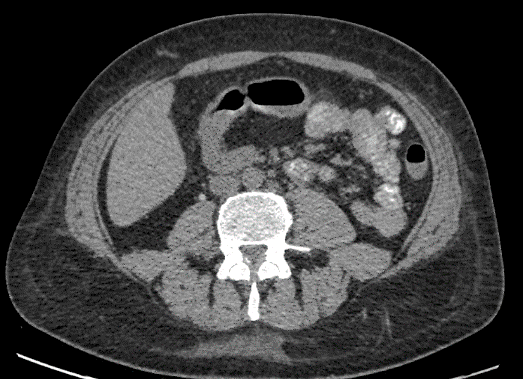
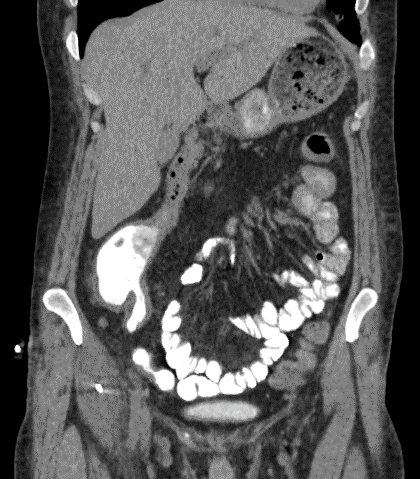
A 31-year-old male presented to Emergency Room with two weeks history of right groin pain and hip pain, as well as intermittent diarrhea for 16 years. He had a temperature of 101°F, tachycardia HR 106bpm. Physical examination revealed right lower abdomen tenderness and the right psoas sign was positive. Laboratory findings showed leukocytosis (WBC 12,400) and anemia (Hemoglobin 8.6 gram). Stool tests for parasites, bacteria, viruses and blood culture were negative. CT scan revealed a right iliopsoas abscess adjacent to the appendix and right colon. CT guided percutaneous drainage and pigtail catheter was placed. He was suspected to have fistulizing Crohn’s disease, was started on Mesalamine, Prednisone and antibiotics. He was discharged home two weeks later on maintenance medication and intravenous antibiotics. Surgical resection was recommended but patient refused. He came back 4 weeks later with worsening hip pain and decreased pigtail drainage. CT revealed iliopsoas fistula involving right iliopsoas into the cecum and duodenocolic fistula involving the second part of the duodenum into hepatic flexure, and extensive myositis, fasciitis, bursitis of right sacroiliac joints.
Figure 1: (A) Right iliopsoas abscess, (B) iliopsoas fistula after pigtail catheter placement, (C) axial view of colo-duodenal fistula, (D) Coronal view of Colo-duodenal fistula.
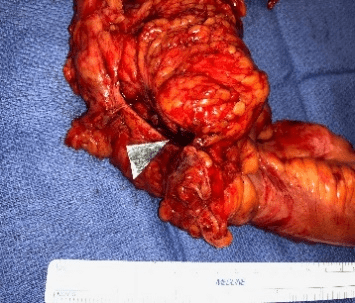
To prevent the development of septic arthritis of the hip joint, a laparoscopic extended right hemicolectomy with iliopsoas fistula and colo-duodenal fistula takedown was performed. An inflammatory mass fixed to the retroperitoneum was taken down associated with the involved bowel, and an abscess opening into the right psoas muscle was recognized and debrided after the ileocecal resection. A duodenocolic fistula fistulizing to the anterior second portion of duodenum was revealed after distal transection of transverse colon. A horizontal wedge duodenectomy was performed using Echelon 60 blue load after confirming adequate remaining lumen of duodenum. An end ileostomy and transverse colon mucus fistula were created.
Figure 2: Gross specimen of right colon with iliopsoas fistula and Duodenocolic fistula (arrow).
The pathology of resected specimen showed chronic active Crohn’s ileocolitis with ulceration, pseudopylop, fistula tracts and abscess formation, and negative for dysplasia. Patient recovered uneventfully and was discharged home on POD5. His transverse mucus fistula and end ileostomy were reversed three months later laparoscopically. He had recovered well when evaluated on his six-month follow-up.
Discussion
Iliopsoas abscess (IPA) is a rare pathology in adults, particularly as complication of the Crohn’s disease (CD). Since Van Patter et al [1] reported the first case of psoas abscess complicating CD in 1954, less than 100 cases have been documented in Western Countries. The primary IPA is caused by hematogenous or lymphatic spread of infection from remote locations. Whereas, secondary IPA develops due to direct spread of infection of psoas muscle from adjacent structures including vertebral bodies and discs, the hip joint, gastrointestinal tract, the genitourinary tract and vascular structures. Inflammatory bowel disease (IBD), especially CD, is the most common cause of secondary IPA, which was also found in cases of infected aortic aneurysm, appendicitis, colorectal cancer and following abdominal surgery [2-6]. The primary IPA predominates in undeveloped countries and in children, while the secondary IPA predominates in developed countries and in adults [7].
The diagnosis of IPA is made by evaluation of the history, careful physical examination, laboratory assessment and imaging studies. Classical triads of iliopsoas abscess include back pain, limp and fever, was described by Mynter in 1881 as a classic manifestation acute psoasitis. However, this may not always be present. Presence of psoas sign on examination may be a clinical clue of iliopsoas abscess. Leukocytosis, elevated erythrocyte segmentation rate and elevated C-reactive protein are significant laboratory features seen in majority of patients [5, 8]. CT is the imaging of choice to evaluate a suspected iliopsoas abscess. Other positive findings include a focal hypodensity, infiltration of surrounding fat, and gas or an air fluid level within the muscle when it fails to reveal an obvious abscess on CT scan [9].
Treatment of an iliopsoas abscess and fistula in CD consists of drainage of abscess (percutaneous or surgical drainage if failed percutaneously), medical management of CD, optimizing nutrition status and surgical resection of fistula and diseased bowel when not responding to medical therapy. A combination therapy with anti-TNF agent and an immunomodulatory agent is recommended for patients with fistulizing Crohn’s disease. In general, aggressive surgery should be avoided. Fistulizing disease not responding to medical therapy is an indication for surgery. Surgery for enteroenteric fistula can be taken as a radical approach with extensive resection of both segments involved in the fistula or a more conservative approach with resection of one segment and sparing of the victim segment provided that the latter is free of Crohn’s disease [10]. Surgical treatment aside, optimization of nutrition in patients with CD should not be overlooked. Poor perioperative nutritional status predisposes to increased risk of postoperative complication. Enteral nutrition (EN) (such as oral supplements, tube feedings are recommended in patients who have undernutrition and fail to meet nutritional requirements by standard diet alone. TPN in inflammatory bowel disease can prevent antigenic stimuli for intestinal mucosa, allow bowel rest as well as supply adequate calories and essential nutrients [11]. As found in the meta-analysis by Brennan et al, postoperative complication was seen in 25% of Crohn’s disease patients who did not receive preoperative TPN whereas it occurred only in 15 % of CD patients who received TPN [12].
Although still an uncommon association, iliopsoas abscess has been reported as a complication of Crohn’s disease. In our case, IPA was the first manifestation of underlying CD. A long duration of chronic inflammatory and fistulizing disease without treatment attributes to iliopsoas abscess formation, as in our case that the patient had intermittent diarrhea for many years. Following CT guided drainage of abscess and antibiotics, patient still had a worsening condition in follow up; this can be considered as another clue to presence of an underlying condition. Presence of fistula, as mentioned above, in repeat imaging, was a strong evidence in favor of Crohn’s disease. The patient’s symptoms resolved only after right hemicolectomy with fistula takedown. Thus, treatment of underlying condition should be also be addressed rather than only an isolated treatment of iliopsoas abscess. In CD with IPA, involved bowel segment should be resected followed by primary anastomosis. Time interval of surgical treatment varies in the literature. Surgery is recommended after resolution of the abscess and optimizing of nutrition status.
Conclusion
Iliopsoas abscess can be a complication of Crohn’s disease, appendicitis, diverticulitis or metastatic colon cancer. CT abdomen/pelvis with Oral and IV contrast is the most efficient and accurate imaging study in diagnosing and identify fistulization. Drainage of the abscess and use appropriate antibiotics is now accepted as a preoperative temporizing procedure to improve patient nutritional status, control sepsis or active inflammation and raise the odds of safe healing after a single operation of resection of the fistula and diseased colon. Time interval of surgical treatment varies in the literature. Persist symptoms and impending septic arthritis prompt early surgical intervention.
Authors’ Contributions
Kai Huang contribute to the concept design, and revised the manuscript; Nikita Sijapati, contribute to draft the manuscript; Abdul Waheed contribute to data acquisition, analysis, Cristiano Alpendre, and Misra Suhasis revised it critically for important intellectual content and give final approval of the version to be submitted. All the authors reviewed and contributed the final version.
Funding
None.
Disclosure
No conflict of interest.
This research was supported (in whole or part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.)
Article Info
Article Type
Case Report & Literature ReviewPublication history
Received: Sat 30, Nov 2019Accepted: Tue 17, Dec 2019
Published: Sat 28, Dec 2019
Copyright
© 2023 Cristiano Alpendre. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2019.01.04
Author Info
Abdul Waheed Cristiano Alpendre Kai Huang Nikita Sijapati Subhasis Misra
Corresponding Author
Cristiano AlpendreGeneral surgery, Brandon Regional Hospital, HCA West Florida Division/USF Consortium
Figures & Tables



References
- Mallick I, Thoufeeq M, Rajendran T (2004) Iliopsoas abscesses. Postgrad Med J 80: 459-462. [Crossref]
- Ogihara M, Masaki T, Watanabe T, Hatano K, Matsuda K et al. (2000) Psoas abscess complicating Crohn's disease: report of a case. Surg Today 30: 759-763. [Crossref]
- Hsu RB, Lin FY (2007) Psoas abscess in patients with an infected aortic aneurysm. J Vasc Surg 46: 230-235. [Crossref]
- Buttaro M, González Della Valle A, Piccaluga F (2002) Psoas abscess associated with infected total hip arthroplasty. J Arthroplasty 17: 230-234. [Crossref]
- Lin MF, Lau YJ, Hu BS, Shi ZY, Lin YH (1999) Pyogenic psoas abscess: analysis of 27 cases. J Microbiol Immunol Infect 32: 261-268. [Crossref]
- Lee YT, Lee CM, Su SC, Liu CP, Wang TE (1999) Psoas abscess: a 10-year review. J Microbiol Immunol Infect 32: 40-46. [Crossref]
- Ricci MA, Rose FB, Meyer KK (1986) Pyogenic psoas abscess: worldwide variations in etiology. World J Surg 10: 834-843. [Crossref]
- Chang CM, Ko WC, Lee HC, Chen YM, Chuang YC (2001) Klebsiella pneumoniae psoas abscess: predominance in diabetic patients and grave prognosis in gas-forming cases. J Microbiol Immunol Infect 34: 201-206. [Crossref]
- Zissin R, Gayer G, Kots E, Werner M, Shapiro-Feinberg M et al. (2001) Iliopsoas abscess: a report of 24 patients diagnosed by CT. Abdom Imaging 26: 533-539. [Crossref]
- Saint-Marc O, Frileux P, Sales JP, Faucheron JL, Balladur P et al. (1994) Entero-enteral fistulas in Crohn disease: radical or conservative surgical treatment of the "victim" segment? Gastroenterol Clin Biol 18: 873-879. [Crossref]
- Triantafillidis JK, Papalois AE (2014) The role of total parenteral nutrition in inflammatory bowel disease: current aspects. Scand J Gastroenterol 49: 3-14. [Crossref]
- Brennan GT, Ha I, Hogan C, Nguyen E, Jamal MM et al. (2018) Does preoperative enteral or parenteral nutrition reduce postoperative complications in Crohn's disease patients: a meta-analysis. Eur J Gastroenterol Hepatol 30: 997-1002. [Crossref]
