Laparoscopic Hepatectomy with Selective Hepatic Artery Clamping for A Hyperintense Hepatic Adenoma on Hepatospecific Gadolinium-Enhanced Magnetic Resonance Imaging: The Great Pretender
A B S T R A C T
Introduction: Focal nodular hyperplasia and hepatocellular adenoma are benign hepatic tumors and differential diagnosis is important as hepatic adenomas may complicate with hemorrhage and malignant transformation. Magnetic resonance imaging with gadolinium-enhanced contrast agents is the best non-invasive diagnostic tool for benign hepatic tumors. Nevertheless, atypical radiological findings can make differential diagnosis a challenge.
Presentation of case: We report a young female patient with large hepatic benign tumor with intralesional hemorrhage that disclosed hyper-intensity on hepatobiliary phase on a gadolinium-enhanced magnetic resonance imaging study, suggestive of focal nodular hyperplasia. As this type of tumor usually do not complicate with bleeding, surgical resection was proposed and a laparoscopic right posterior hepatic sectionectomy with selective hepatic artery clamping was performed. Pathology disclosed an inflammatory hepatic adenoma.
Discussion: Hepatic adenomas may present as hyper-intense tumors on hepatobiliary phase of gadolinium-enhanced magnetic resonance imaging. Surgical resection still has a role on the treatment of benign hepatic tumors. Laparoscopic liver resections must be considered, even when a major hepatectomy is planned, as this approach has proved safe and effective. Selective hepatic artery clamping during minimally invasive liver surgery may be an option to reduce intraoperative bleeding, remnant liver ischemia and postoperative hepatic failure.
Conclusion: We reported a young female patient with a benign hepatic tumor complicated with hemorrhage suggestive of a focal nodular hyperplasia on gadolinium-enhanced magnetic resonance imaging study. A laparoscopic hepatectomy was performed and final pathology disclosed an inflammatory hepatocellular adenoma.
Keywords
Adenoma, liver cell, magnetic resonance imaging, gadolinium, hepatectomy
Introduction
Magnetic resonance imaging (MRI) using hepatobiliary (HPB) gadolinium (Gd) based contrast agents is a powerful tool on one of the biggest diagnostic challenges in hepatology: the non-invasive differentiation between focal nodular hyperplasia (FNH) and hepatocellular adenoma (HCA), benign hepatic lesions that usually occur in middle-aged woman that are typically asymptomatic and discovered incidentally on routine abdominal image studies [1]. While FNH has no malignant deterioration potential and is rarely associated with complications, HCA is associated with rupture, hemorrhage and malignant transformation [2]. Therefore, the differentiation of an FNH from a HCA is very important, as FNHs most of the times are conducted conservatively and HCAs many times require surgical treatment [3]. Several studies and extensive experience on MRI using Gd based contrast agents demonstrate that HCAs are almost invariably hypointense on delayed HPB phase while FNHs are typically hyper or isointense lesions [4]. In this study, we report a female patient with a large right liver tumor that complicated with hemorrhage. An MRI with HPB Gd based contrast agent (gadoxetic acid - Primovist®; Bayer-Schering, Berlin, Germany) was performed and the tumor presented hyperintensity at late HPB phase of the study and was suspected as an FNH. The patient was submitted to a laparoscopic right posterior sectionectomy with selective hepatic artery clamping as previously described by Surjan et al. Despite of the characteristic findings on the MRI, final pathology disclosed an inflammatory hepatic adenoma [5].
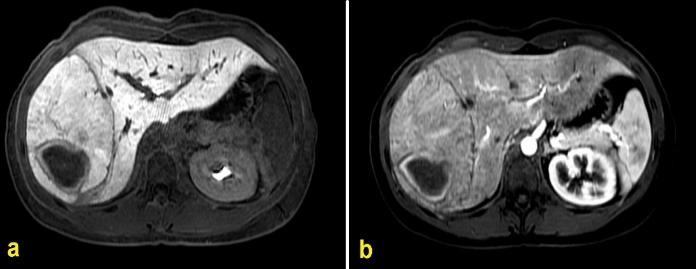
Figure 1: MRI study axial images disclosing a large right hepatic tumor with signs of intralesional bleeding.a) MRI with Primovist® contrast agent, late HPB phase disclosing an hyperintense right hepatic tumor; b) MRI right hepatic tumor with enhenacement at the arterial phase. (MRI: magnetic resonance imaging; HPB: hepatobiliary).
Figure 2: MRI study axial plane image of late HPB phase disclosing a 2,2 cm hypointense left hepatic sector tumour suggestive of a HCA (yellow arrow) and a large hyper-intense right liver tumour with signs of intralesional hemorrhage suggestive of a FNH, with possible differential diagnoses of inflammatory or beta-catenin-mutated HCA. (MRI: magnetic resonance imaging; HPB: hepatobiliary; HCA: hepatocellular adenoma; FNH: focal nodular hyperplasia).
Presentation of Case
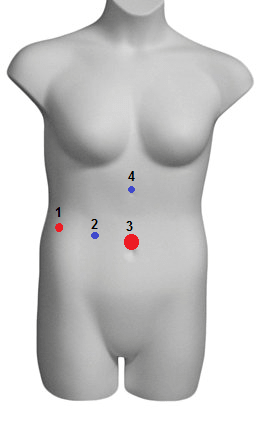
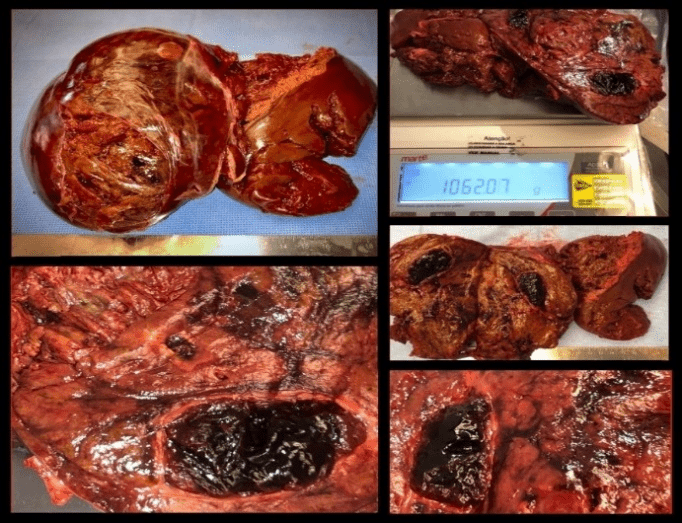
An asymptomatic 26-year-old female patient with previous history of oral contraceptives use was submitted to a routine abdominal sonography during gynecological evaluation that disclosed a large hepatic right liver tumor. During further evaluation of the lesion, an MRI with Gd based contrast agent Primovist® disclosed a 14,0 x 13,6 x 8,5 cm hepatic tumor on the right lateral sector. The tumor presented signs of intratumoral hemorrhage and an 80-cc hematoma, with intense enhancement during the arterial and HPB phases of the study, suggestive of an FNH (Figure 1). The MRI also disclosed several other hepatic tumors with arterial enhancement but that were hypointense in the HPB phase, the largest on the left lateral hepatic sector (Figure 2). As FNHs do rarely present with any complications and are not associated with hemorrhage, despite the radiological aspect suggestive of this type of benign hepatic lesion and taking under consideration the antecedent of oral contraceptive use and the possibility of an inflammatory HCA with intralesional bleeding, a laparoscopic hepatectomy was proposed. The patient was submitted to a totally laparoscopic anatomical right posterior hepatic sectionectomy with 4 laparoscopic trocars (Figure 3). Instead of performing an intermittent Pringle maneuver or a right hemi-Pringle to minimize intraoperative bleeding during parenchymal transection, our option was to perform continuous selective right hepatic artery clamping, as we previously described [5, 6]. This surgical technique can be easily performed with a laparoscopic bulldog clamp without the need of a dedicated trocar or repeated intermittent clamping and, while partially preserving portal flow, prevents remaining liver ischemia (Figure 4) [7, 8]. Operative time was 240 minutes. Surgical specimen was retracted through a suprapubic incision. Final pathology disclosed a 13, 2 cm inflammatory hepatic adenoma with intralesional hemorrhage and free surgical margins (Figure 5). Postoperative period was uneventful. The patient was discharged on the third postoperative day.
Figure 3: Trocar displacement for a totally laparoscopic right posterior sectionectomy with selective hepatic artery clamping. Trocars: 1) 5 mm surgeon left hand; 2) 5 mm camera port; 3) 12 mm surgeon right hand – vascular stapler; 4) 5 mm assistant port.
Figure 4: Intraoperative images of a totally laparoscopic right hepatic posterior sectionectomy. a) selective clamping of the right hepatic artery; b) ischemic delineation of the right liver after hepatic artery clamping; c) determination of the line of hepatic transection for a right posterior sectorectomy; d) final aspect of a right laparoscopic posterior sectionectomy. Transection was performed with harmonic scalpel, bipolar forceps and endoscopic vascular stapler. Hemostatic tissue applied to the raw surface area and a 19 Fr Blake drain positioned.
Figure 5: Surgical specimen.
Discussion
HCAs are benign hepatic tumors that mostly develop in young females usually taking contraceptive medications [9]. The differential diagnosis of this tumor from other benign primary liver tumors such as FNH and hemangioma is extremely important, as HCAs may complicate with tumor hemorrhage and malignant transformation [9]. However, the precise diagnosis of this tumor is not always straight forward, as many times it is difficult to differentiate this tumor specially from FNHs.
The development of HPB contrast agents for MRI has improved the accuracy on the non-invasive diagnosis of benign hepatic tumors [10]. HCAs most commonly appear as intensely enhanced lesions on the arterial phase of an MRI and hypo-intense in HPB phases of the study, different from FNHs that are usually iso or hyper-intense in late HPB phase of a Gd-enhanced MRI [2]. Nevertheless, although uncommon, HCAs may appear as iso- or hyperintense in comparison to adjacent normal liver on HPB phase images, specially the inflammatory type of HCA [11].
We reported the case of an asymptomatic young female patient with previous use of contraceptive medications that presented with a large hepatic tumor with sings of hemorrhage on image studies. Although being suggestive of an FNH on the HPB phase of a Primovist® enhanced MRI, our option was to perform a laparoscopic hepatectomy to resect the tumor. The rationale for this treatment was that FNHs are not associated with bleeding and that some HCAs may appear as iso- or hyperintense tumors on Gd-enhanced MRI [12]. In the era of minimally invasive hepatic resection, laparoscopic hepatectomy is a safe and effective procedure to treat selected benign hepatic lesions, even when major hepatectomies are required [13]. Minimizing intraoperative bleeding and remaining liver ischemia are paramount to achieve adequate operative results, low morbidity and intended dismal mortality [13]. The use of the selective hepatic artery clamping emerges in this context as an effective operative technique to enhance surgery results [6].
Therefore, it must be kept in mind that there is still a place for surgeryon the treatment of benign hepatic lesions. Recent advances on the knowledge of different pathological and molecular characteristics of both FNHs and HCAs have emerged to demonstrate that even some types of FNHs must be considered to surgical resection [14]. Although Gd-enhanced MRI are the best non-invasive diagnostic method for benign hepatic tumors, non-usual characteristics of these tumors must always be suspected.
Conclusion
We report a totally laparoscopic right posterior hepatic sectionectomy with selective hepatic artery clamping for the treatment of a large hepatocellular adenoma that presented with intralesional hemorrhage and atypical characteristics on a gadolinium- enhanced magnetic resonance imaging study.
Conflicts of Interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Approval
This article does not contain any personal information that can lead to the identification of the patient.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author’s Contribution
RCTS designed and wrote the paper. AZAB performed data collection and figures editing. RB provided critical review. SPS performed data collection and wrote the paper. MFAB provided critical review and designed the paper. All authors approved the final version of this manuscript.
Highlights
• MRI with Gd-based contrast agents is the best non-invasive diagnostic tool for benign hepatic tumors.
• HAs may present atypical findings on late HPB phase of MRI using gadoxetic acid.
• Laparoscopic hepatectomy is a safe and effective procedure for the treatment of benign hepatic tumors.
• Selective hepatic artery clamping may reduce remnant liver ischemia.
Article Info
Article Type
Case ReportPublication history
Received: Thu 07, Nov 2019Accepted: Mon 25, Nov 2019
Published: Fri 06, Dec 2019
Copyright
© 2023 Rodrigo Cañada Trofo Surjan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.02.07
Author Info
Rodrigo Cañada Trofo Surjan Andrea Zaidan de Almeida Barros Roberto Blasbalg Sergio do Prado Silveira Mauricio Fernando de Almeida Barros
Corresponding Author
Rodrigo Cañada Trofo SurjanHospital Nove de Julho, Surgery Department, Rua Peixoto Gomide, 545 - Cerqueira César, São Paulo, Brazil
Figures & Tables


References
- Lizardi-Cervera J, Cuéllar-Gamboa L, Motola-Kuba D (2006) Focal nodular hyperplasia and hepatic adenoma: a review. Ann Hepatol 5: 206-211. [Crossref]
- Mohajer K, Frydrychowicz A, Robbins JB, Loeffler AG, Reed TD et al. (2012) Characterization of hepatic adenoma and focal nodular hyperplasia with gadoxetic acid. J Magn Reson Imaging 36: 686-696. [Crossref]
- Maillette de Buy Wenniger L, Terpstra V, Beuers U (2010) Focal nodular hyperplasia and hepatic adenoma: epidemiology and pathology. Dig Surg 27: 24-31. [Crossref]
- Grazioli L, Morana G, Kirchin MA, Schneider G (2005) Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology 236: 166-177. [Crossref]
- Surjan RC, Makdissi FF, Basseres T, Leite D, Charles LF (2016) First totally laparoscopic ALPPS procedure with selective hepatic artery clamping: Case report of a new technique. Medicine (Baltimore) 95: e4236. [Crossref]
- Surjan RC, Makdissi FF, Basseres T, Machado MA (2018) Advanced hepatocellular carcinoma with portal tumor thrombosis in cirrhotic patient: laparoscopic right hepatectomy with vascular reconstruction. J Vis Surg 4: 223.
- Jakimowicz J, Stultiëns G, Smulders F (1998) Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc 12: 129-132. [Crossref]
- Yokoyama Y, Alterman DM, Sarmadi AH, Baveja R, Zhang JX (2002) Hepatic vascular response to elevated intraperitoneal pressure in the rat. J Surg Res 105: 86-94. [Crossref]
- European Association for the Study of the Liver (EASL) (2016) EASL Clinical Practice Guidelines on the management of benign liver tumours. J Hepatol 65: 386-398. [Crossref]
- Ronot M, Bahrami S, Calderaro J, Valla DC, Bedossa P et al. (2011) Hepatocellular adenomas: accuracy of magnetic resonance imaging and liver biopsy in subtype classification. Hepatology 53: 1182-1191. [Crossref]
- Glockner JF, Lee CU, Mounajjed T (2018) Inflammatory hepatic adenomas: Characterization with hepatobiliary MRI contrast agents. Magn Reson Imaging 47: 103-110. [Crossref]
- Dharmana H, Saravana-Bawan S, Girgis S, Low G (2017) Hepatocellular adenoma: imaging review of the various molecular subtypes. Clin Radiol 72: 276-285. [Crossref]
- Abu Hilal M, Di Fabio F, Teng MJ, Godfrey DA, Primrose JN et al. (2011) Surgical management of benign and indeterminate hepatic lesions in the era of laparoscopic liver surgery. Dig Surg 28: 232-236. [Crossref]
- Balabaud C, Al-Rabih WR, Chen PJ, Evason K, Ferrell L et al. (2013) Focal Nodular Hyperplasia and Hepatocellular Adenoma around the World Viewed through the Scope of the Immunopathological Classification. Int J Hepatol 268625. [Crossref]
