Laparoscopic Appendectomy Turned Hepatotomy Revealing Rare Streptococcus Species: A Case Report
A B S T R A C T
While appendicitis is a common surgical emergency, progression to hepatic abscess due to rare microbial species is an unusual complication. We present the case of a 55 year-old male with past medical history of hypothyroidism presenting with one week of fever, cough, rigors, dyspnea, and generalized abdominal pain. He was diagnosed with viral gastroenteritis at urgent care but presented to the emergency room a week later where subsequent CT scan revealed appendiceal inflammation and hepatic abscess. He underwent laparoscopic appendectomy and hepatotomy, revealing perforated appendicitis, appendiceal abscess, localized peritonitis, and a hepatic abscess. Microbiology identified viridans streptococcus, citrobacter koseri, streptococcus intermedius, and streptococcus gordonii. He was treated with broad-spectrum antibiotics and additional percutaneous drainage. He was discharge on a 30-day course of oral antibiotics. This case highlights an unusual complication of appendicitis leading to hepatic abscess with rare bacterial isolates. Surgical intervention and targeted antimicrobial therapy were key in managing this patient.
Keywords
Appendiceal perforation, hepatic abscess, microbiology, streptococcus, surgery
Introduction
Acute appendicitis is a common surgical emergency requiring prompt diagnosis and intervention to prevent complications such as perforation, peritonitis, and abscess formation [1]. Delays in treatment can significantly increase the risk of complications, leading to higher morbidity and hospital stays [2]. Literature has shown that the risk of appendiceal perforation increases by about 9% for each day of delay in surgical intervention [3], underscoring the need for timely surgical intervention. The American College of Surgeons and other surgical societies advocate for prompt surgical management of acute appendicitis to minimize morbidity [4].
Appendicitis has a global incidence rate of approximately 100 per 100,000 person-years in North America, with variations by region [5]. The incidence is highest in newly industrialized countries in Asia and the Middle East, with rates as high as 206 per 100,000 person-years in South Korea [6]. The peak incidence occurs in the 15-19 year age group, with the condition more common in males than females [7].
Hepatic abscesses, although rare, can occur as a complication of appendicitis, particularly when there is a perforation and subsequent spread of infection [8]. Pyogenic liver abscesses are most commonly caused by spread of bacterial infections from the gastrointestinal tract, including the appendix [8]. The presence of hepatic abscesses in the context of appendicitis is associated with increased morbidity, often requiring a combination of surgical drainage and targeted antibiotic therapy for effective management [9].
With this case, we aim to highlight the adverse effects of delayed surgical intervention for appendicitis including the development of sepsis and multiple hepatic abscesses. This case also highlights the need for comprehensive microbiological evaluation in liver abscesses and the importance of tailored antibiotic therapy. Early surgical intervention of appendicitis is crucial in preventing adverse effects.
Case Presentation
We present the case of a 55-year-old man with past medical history of hypothyroidism and no past surgical history who presented to a regional emergency department with a one-week history of progressive fever (104 F), cough, rigors, dyspnea, constipation, and right upper and lower quadrant abdominal pain. Initially, he was evaluated at an urgent care, where he was diagnosed with viral gastroenteritis and managed symptomatically. Upon arrival to the emergency department, vital signs were notable for tachycardia, fever, and mild hypotension. Physical examination revealed vague tenderness diffusely throughout the abdominal with guarding and rebound tenderness in the right lower quadrant. Labs showed leukocytosis measuring 15,000 and stable hemoglobin and platelet levels. Contrast-enhanced CT scan of the abdomen and pelvis showed large, multiloculated cysts throughout the right hepatic lobe concerning for abscess with thickening of the appendix and a small adjacent appendiceal abscess measuring 2.5 × 1.1 cm.
Given these findings, the patient was taken for urgent laparoscopic appendectomy and hepatotomy for drainage of the hepatic abscess. Surgical exploration revealed the appendix densely adherent to the retroperitoneum with an abscess posterior. The liver was inflammatory on the lateral aspect of the right lobe and adherent to the peritoneum. Upon bluntly peeling the liver off the peritoneum, copious white, thick purulent fluid came in to view and was drained. More superiorly, there was another abscess cavity drained. About 800 cc of purulent fluid was evacuated for culture. A Jackson-Pratt drain was placed in the right hepatic lobe.
Microbiology revealed rare viridans streptococcus and Citrobacter koseri for the liver abscess. Blood culture grew streptococcus intermedius and streptococcus gordonii. The patient was admitted and initiated on vancomycin, piperacillin-tazobactam, and fluconazole given the size of the hepatic abscess and suspected appendiceal source. Despite initial surgical intervention, interventional radiology placed an additional accordion drain deeper into the hepatic abscess, which subsequently drained an additional 500 cc of mucopurulent discharge over two days. As drain output decreased, he was discharged with a 30-day course of oral Augmentin and Levofloxacin. The patient’s clinical condition improved significantly with this regimen.
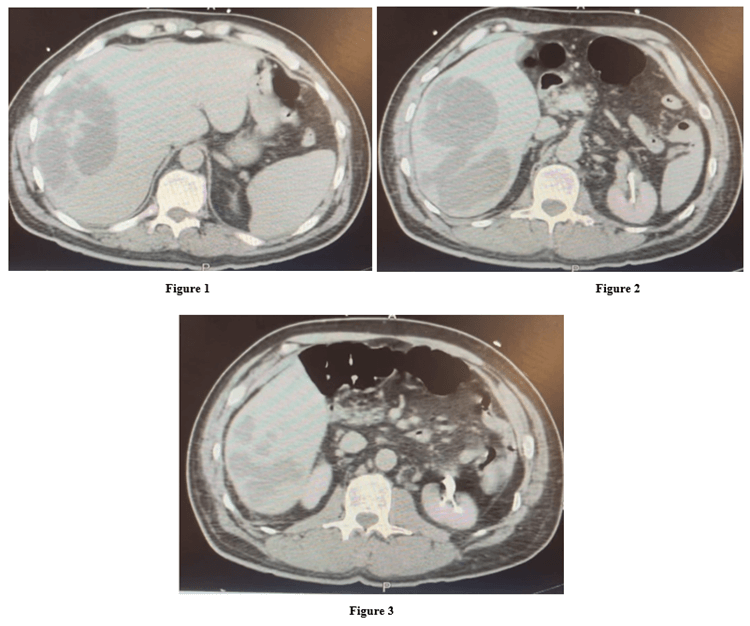
Figure 1-3: Proximal to distal CT scan of the hepatic abscesses.
Figure 4: Timeline of events for the presentation and management of this case.
Discussion
Hepatic abscesses secondary to appendicitis are rare and often result from hematogenous, direct, or lymphatic spread of infection [2]. In this case, the hepatic abscess was likely seeded from an adjacent perforated appendiceal abscess. The patient was treated with vancomycin and Zosyn, which is supported by the American Association for the Study of Liver Diseases for managing complex intra-abdominal infections, including liver abscesses, especially with suspected multi-drug resistant organisms [10].
The microbiological findings in this case are notable for the presence of rare pathogens, including Viridans Streptococcus and Citrobacter Koseri. The most common bacteria found in liver abscesses are Klebsiella Penumoniae, Escherichia Coli, and other enterobacteria [11]. Though uncommon, these pathogens but should be considered in differential diagnoses, especially in the context of polymicrobial infections following gastrointestinal perforations [12].
This case underscores the importance of early surgical management of appendicitis to avoid morbidity. It is also important to consider appendicitis as a source of hepatic abscesses, especially in atypical presentations. The identification of rare pathogens further emphasizes the need for comprehensive microbiological analysis to guide appropriate antimicrobial therapy. The decision to use interventional radiology for additional drainage proved beneficial, significantly reducing the abscess volume and infection burden. A combination of surgical drainage and broad-spectrum antimicrobial therapy is essential for managing complex cases. A multidisciplinary approach utilizing surgery, medicine, and interventional radiology was key to the successful management of this case.
Data Availability
Please contact authors regarding data at email provided.
Declarations of Interest
None.
Author Contributions
Kyra Hunsberger: Project conception, writing, original and final draft, project administration. Burke De Lange, DO: project conception.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 02, Apr 2025Accepted: Thu 08, May 2025
Published: Thu 22, May 2025
Copyright
© 2023 Kyra Hunsberger. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2025.01.02
Author Info
Kyra Hunsberger Burke De Lange
Corresponding Author
Kyra HunsbergerThe University of Arizona, College of Medicine - Phoenix, Phoenix, Arizona, United States of America
Figures & Tables

References
1.
Westfall KM, Charles
AG (2019) Risk of Perforation in the Era of Nonemergent Management for Acute
Appendicitis. Am Surg 85 (11): 1209-1212. [Crossref]
2.
Saar S, Talving P,
Laos J, Podramagi T, Sokirjanski M et al. (2016) Delay Between Onset of
Symptoms and Surgery in Acute Appendicitis Increases Perioperative Morbidity: A
Prospective Study. World J Surg 40 (6): 1308-1314. [Crossref]
3.
Elniel M, Grainger J,
Nevins EJ, Misra N, Skaife P (2018) 72 h Is the Time Critical Point to Operate
in Acute Appendicitis. J Gastrointest Surg 22 (2): 310-315. [Crossref]
4.
Kovler ML, Pedroso FE,
Etchill EW, Vacek J, Bouchard ME et al. (2022) Prolonged In-hospital Time to
Appendectomy is Associated With Increased Complicated Appendicitis in Children.
Ann Surg 275 (6): 1200-1205. [Crossref]
5.
Appendicitis
Collaborator Group (2024) Trends and levels of the global, regional, and
national burden of appendicitis between 1990 and 2021: findings from the Global
Burden of Disease Study 2021. Lancet Gastroenterol Hepatol 9 (9):
825-858. [Crossref]
6.
Ferris M, Quan S,
Kaplan BS, Molodecky N, Ball CG et al. (2017) The Global Incidence of
Appendicitis: A Systematic Review of Population-based Studies. Ann Surg
266 (2): 237-241. [Crossref]
7.
Wickramasinghe DP,
Xavier C, Samarasekera DN (2021) The Worldwide Epidemiology of Acute
Appendicitis: An Analysis of the Global Health Data Exchange Dataset. World
J Surg 45 (7): 1999-2008. [Crossref]
8.
Liao KF, Lai SW, Lin
CL, Chien SH (2016) Appendectomy correlates with increased risk of pyogenic
liver abscess: A population-based cohort study in Taiwan. Medicine
(Baltimore) 95 (26): e4015. [Crossref]
9.
Weiss CR, Bailey CR,
Hohenwalter EJ, Pinchot JW, Ahmed O et al. (2020) ACR Appropriateness Criteria®
Radiologic Management of Infected Fluid Collections. J Am Coll Radiol 17
(5S): S265-S280. [Crossref]
10. Biggins SW, Angeli P, Garcia-Tsao G, Gines P, Ling SC et al. (2021)
Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial
Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American
Association for the Study of Liver Diseases. Hepatology 74 (2):
1014-1048. [Crossref]
11. Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC et al. (2018) A
Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious
Diseases: 2018 Update by the Infectious Diseases Society of America and the
American Society for Microbiology. Clin Infect Dis 67 (6): e1-e94. [Crossref]
12. Kitahara H, Park Y, Seharada K, Yoshimura M, Horiuchi A et al. (2024) Culture-based bacterial evaluation of the appendix lumen and antibiotic susceptibility of acute appendicitis in Japan: A single-center retrospective analysis. Medicine (Baltimore) 103 (29): e39037. [Crossref]
