Journals
Knowledge of UK Dental Undergraduates and Dentists in Treating Dentine Hypersensitivity
A B S T R A C T
Aim: The purpose of the present questionnaire-based study was to evaluate the knowledge and understanding of UK based dental undergraduates and qualified dentists in treating Dentine Hypersensitivity (DH).
Methods: 120 questionnaires were handed out to 4th and 5th year dental students and Staff at the Dental Hospital in London UK as part of a collaborative study with the Faculdade de Odontologia de Bauru, University of Sao Paulo, Brazil. The questionnaire consisted of 22 questions, which included both open and closed questions.
Results: 91 questionnaires (75.8% response rate) were returned; of the 91 respondents (38M; 52F, 1 missing value) 53 were dentists (61%) and 34 were dental students (39%) (4 missing values). 37.5% of students indicated that 10% of patients suffered from DH whereas 18.9% of dentists indicated that 25% of patients suffered from DH. Both dentists (22.6%) and 27.5% of students indicated that DH lasted >12 weeks. 18.9% of dentists considered that DH was a serious problem for patients although 32.5% of students were not sure. Dentists (66%) and students (62.5%) indicated that DH had a major impact on the quality of life (QOL) with 51.1% (dentists) and 56.3% (students) indicating that it was moderate in nature.
Conclusion: The results of the present pilot study would suggest that in terms of knowledge and understanding of DH (e.g., hydrodynamic theory) both dentists (90.5%) and students (76.9%) were comparable although in the assessment and subsequent management of DH the results indicated that dentists were more confident than the students.
Keywords
Dentine hypersensitivity, knowledge, questionnaire
Introduction
Dentine Hypersensitivity (DH) is a recognized clinical condition that may have a profound impact on the Quality of life (QoL) of those who suffered from the problem [1-4]. Although there have been numerous questionnaire studies reporting on the prevalence of DH in patient populations which may be as high as 57%, data, however from the dentist’s perspective of the prevalence of DH is in the region of 10-25% [5-13]. Furthermore, previous studies or reviews have indicated that dentists may be uncertain about the aetiology, diagnosis, and effective management of Dentine Hypersensitivity (DH) [10, 11, 14-16]. This lack of awareness or understanding regarding DH may therefore have an impact on how confident the dentist is in managing the condition and whether DH will be successfully treated to the patient’s satisfaction.
Aim
The aim of the study was to evaluate the knowledge and understanding of UK based dental undergraduates and qualified dentists in treating Dentine Hypersensitivity (DH).
Materials & Method
120 questionnaires were handed out to 4th and 5th year dental students and Staff at The Royal London Dental Hospital, UK as part of a collaborative study with the Faculdade de Odontologia de Bauru, University of Sao Paulo, Brazil. The study was submitted to the local Queen Mary University of London Ethics committee (QMREC) and the research did not present any ethical concerns due to its low risk and therefore did not require the scrutiny of the full Research Ethics Committee.
The questionnaire consisted of 22 questions, which included both open and closed questions. The questionnaires were distributed from April 2011 to Feb 2012 by JH to both the dental students and Staff members of the Dental hospital. Data were entered using the Microsoft Excel, and the results analysed using SPSS 22.0 for Windows (IBM, Portsmouth UK) in presented in the form of frequency distribution tables and figures.
Results
91 questionnaires (75.8% response rate) were returned; of the 91 respondents (38M; 52F, 1 missing value) 53 were dentists (61%) and 34 were dental students (39%) (4 missing values). When asked if they had examined a patient with DH in the last two-four weeks/month (Q. 2), 62.7% (n=32) of dentists and 37.3% (n=15) of the students indicated that they did examine a patient with DH. In response to Q3 on the estimated percentage of patients attending the Dental hospital reported that they had DH, 37.5% (n=15) of the students estimated that 10% of patients suffered from DH, whereas 18.9% (n=10) of dentists estimated that 25% of patients suffered from DH.
When asked whether the patient or the dentist/student initiated the conversation prior to a clinical examination and subsequent diagnosis of DH (Q.4-5), 73.1% (n=38) of dentists and 87.5% (n=35) of students indicated that the patient initiated the conversation. Whereas only 24.4% (n=11) of dentists and 9.8% (n=4) of students indicated that the clinician initiated the conversation about DH with the patient.
In response to Q.6 both dentists (73.1%; n=38) and students (74.4%; n=29) reported that they had observed the signs associated with DH. When asked whether they considered DH to be a serious clinical problem (Q.7) 18.9% (n=10) of dentists considered that DH was a serious problem in their patients although 32.5% (n=13) of students were unsure. Both dentists (22.6% n=12) and 27.5% (n=11) of students estimated that DH lasted >12 weeks (Q.8)
When asked whether DH had a major impact on the QoL of their patients 66% (n=35) of dentists and 62.5% (n=25) of students indicated that DH had a major impact on the quality of life (QOL) with 51.1% (n=35) of dentists and 56.3% (n=28) of students indicating that this impact was mild to moderate in nature (Q.9-10). Both dentists (36.5%; n=19) and students (32.5%; n=13) indicated that they were often asked about the condition by their patients (Q.11).
Responses to Q. 12 regarding the aetiology of DH highlighted some differences between the dentist and student responses. The main suggestions by the dentists and students were as follows: 1) Exposed dentine (46.3%; n=25), 2) Gingival recession (33.4%; n=18), 3) Abrasion (27.8%; n=15), 4) Erosion (22.2%; n=11) and 5) Periodontal disease (20.4%; n=11) for dentists and 1) Exposed dentine (73.2%; n=30), 2) Gingival recession 43.9%; n=18), 3) Abrasion (19.5%; n=8), 4) Fluid movement (19.5%; n=8) and 5) Loss of enamel (19.5%; n=8) for the students (Table 1).
Table 1: Selected responses from Q.12 regarding an understanding of the aetiology of DH.
|
Q.12 The Aetiology of Dentine Hypersensitivity (Selected variables) |
Staff (n) |
Students (n) |
|
Exposed Dentine |
25 |
30 |
|
Gingival Recession |
18 |
18 |
|
Abrasion |
15 |
8 |
|
Fluid Movement |
9 |
8 |
|
Loss of Enamel |
4 |
8 |
|
Wrong (incorrect) brushing |
4 |
5 |
|
Periodontal Disease |
11 |
5 |
|
Enamel Fracture |
4 |
5 |
|
Erosion |
11 |
4 |
|
Attrition |
5 |
3 |
|
Bleaching Techniques |
2 |
3 |
|
Periodontal Treatment (post-operative sensitivity) |
5 |
2 |
|
Leaking Restoration |
3 |
2 |
|
Caries |
6 |
2 |
When asked to respond to the question on the steps taken to clinically diagnose a patient with dentine hypersensitivity (Q.13) the four most common diagnostic tools recommended by both dentists and students were 1) Clinical Sensitivity to Cold (59.3%; n= 32)(73.2%; n=30 ), 2) Clinical Examination (55.6%; n=30)(53.7%; n=22), 3) Dentine Hypersensitivity History (42.6%; n=23)(51.2%; n=21) and 4) Vitality Test (18.5%; n=10)(19.5%; n=8). The fifth most frequent response by dentists was ‘eliminate the cause of DH’ (16.7%; n=9), whereas for students the fifth most frequent response was ‘aggravating factor’ (17.5%: n=7) (Table 2).
Table 2: Selected responses from Q.13 on what steps would you take to clinically diagnose a patient with DH.
|
Q.13 What steps would you take to clinically diagnose a patient with dentine hypersensitivity (Selected variables) |
Staff (n) |
Students (n) |
|
Clinical Sensitivity to Cold, |
32 |
30 |
|
Clinical Examination, |
30 |
22 |
|
Dentine Hypersensitivity History |
23 |
21 |
|
Vitality Test |
10 |
8 |
|
Aggravating factor |
5 |
7 |
|
Eliminate the cause of Dentine Hypersensitivity |
9 |
3 |
|
Assess Recession |
8 |
6 |
|
Take a radiograph |
7 |
5 |
|
Clinical Testing Not Specified |
7 |
4 |
|
Apply Bonding Agent |
1 |
5 |
|
Provision of a desensitising toothpaste |
1 |
5 |
|
Med History |
2 |
2 |
|
Diet History |
2 |
3 |
When asked, what other dental conditions would you take into consideration when making a diagnosis of DH (Q.14) both dentists and students provided similar responses (Table 3). The main responses for both dentists and students were as follows: 1) Cracked Tooth Syndrome (72.2%; n=39)(73.2%; n=30), 2) Fractured Restoration (75.9%; n=41)(70.7%; n=29), 3) Chipped Tooth (72.2%; n=39)(65.9%; n=27), 4) Dental Caries (74.1%; n=40)(92.7%; n=38), 5) Bleaching Sensitivity (83.3%; n=45) (61%; n=25), 6) Periodontal Disease (61.1%; n=33)(73.2%; n=30), 7) Post-Operative Sensitivity (72.2%; n=39)(70.7%; n=29), 8) Marginal Leakage (70.4%; n=38)(78%; n=32) and 9) Pulpitis (66.7%; n=36)(73.2%; n=30) (Table 3).
Table 3: Selected responses from Q.14 on what other dental conditions would you take into consideration when making a diagnosis of DH.
|
Q.14 what other dental conditions would you take into consideration when making a diagnosis of DH? (Selected variables) |
Staff (n) |
Students (n) |
|
Cracked Tooth Syndrome |
39 |
30 |
|
Fractured restoration |
41 |
29 |
|
Chipped teeth |
39 |
27 |
|
Dental Caries |
40 |
38 |
|
Periodontal Disease |
33 |
30 |
|
Post-operative sensitivity |
39 |
29 |
|
Marginal Leakage |
38 |
32 |
|
Pulpitis |
36 |
30 |
|
Palatogingival groove |
16 |
8 |
|
Bleaching Sensitivity |
45 |
25 |
|
None |
11 |
6 |
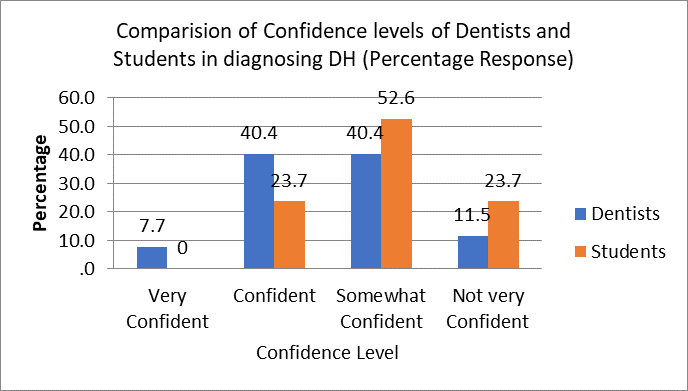
The responses to Q15 on how confident the participants were in correctly diagnosing dentine hypersensitivity rather than other dental conditions that result in pain indicated that dentists claimed to be more confident than the students on differential diagnosing DH from other dental conditions. For example, 7.7% (n=4) indicated that they were very confident in diagnosis DH, with 40.4% (n=21) indicating that they were confident with 40.4% (n=21) indicating that they were somewhat confident respectively. Whereas students, indicated that they were either confident (23.7%; n=9) or somewhat confident (40.8%; n=20). There were relatively more students indicating that they were not very confident (23.7%; n=9) compared to dentists 11.5% (n=6) (Figure 1).
Figure 1: Comparison of confidence levels of Dentists and Students in diagnosing DH.
When asked about the currently accepted theory of DH (Q.16) occurs? 90.5% (n=38) of dentists and 76.9% (n=20) of students indicated that the hydrodynamic theory was the currently held theory. Other responses by the students (23.1%; n=6) indicated that other theories (including nerve desensitization) were considered compared to the dentists’ other responses (9.5%; n=4).
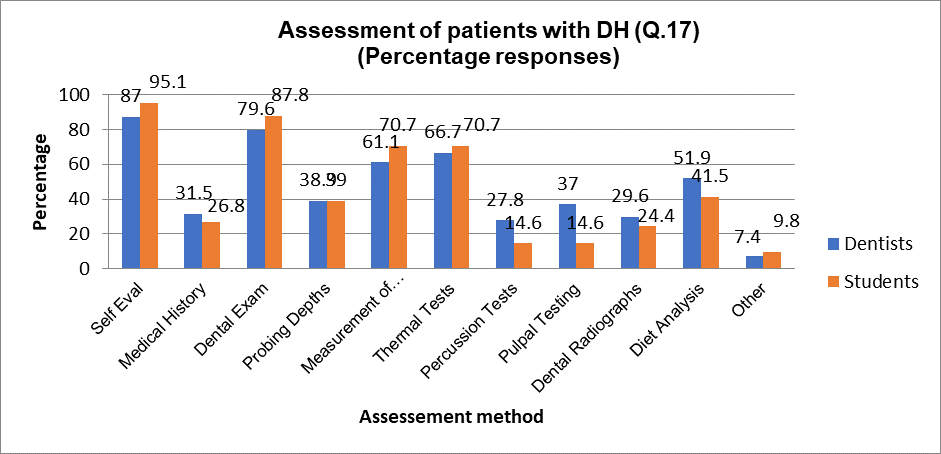
The responses from dentists and students to how they assessed/evaluated patients complaining of dentine hypersensitivity in the surgery environment (Q.17) are shown in (Figure 2). The five main assessment methods based on the dentist and student responses were as follows: 1) Self Evaluation (87%; n=47)(95.1%; n=39), 2) Dental Exam (76.6%; n=43)(87.8%; n=36), 3) Measurement of recession (61.1%; n=33)(70.7%; n=29), 4) Thermal tests (66.7%; n=36)(70.7%; n=29) and 5) Diet analysis (51.9%; n=28)(41.5% (n=17) (Figure 2).
Figure 2: Dentists and Students responses to Q17 on how to assess/evaluate patients complaining of DH in the surgery environment.
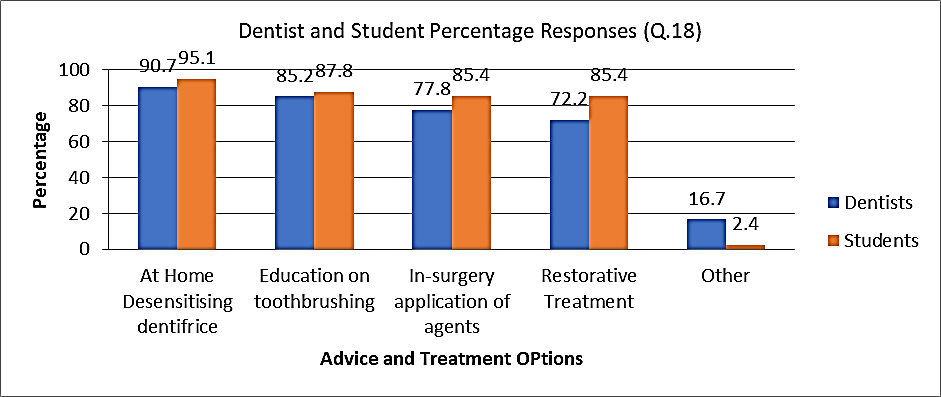
The advice recommended by both dentists and students to patients experiencing DH (Q.18) was in reasonable agreement as follows; 1) At Home desensitizing dentifrice (90.7%; n=49)(95.1%; n=39), 2) Education on toothbrushing (85.2%; n=46)(87.8%; n=36), 3) In-surgery application of a desensitizing agent (77.8%; n=42)(85.4%; n=35) 4) restorative treatment (72.7%; n=39)(85.4%; n=35) and 5) Other options (not specified 16.7%; n=9)(2.4%; n=1) (Figure 3).
Figure 3: Advice and treatment options recommended by Dentists and students to patients with DH (Q.18).
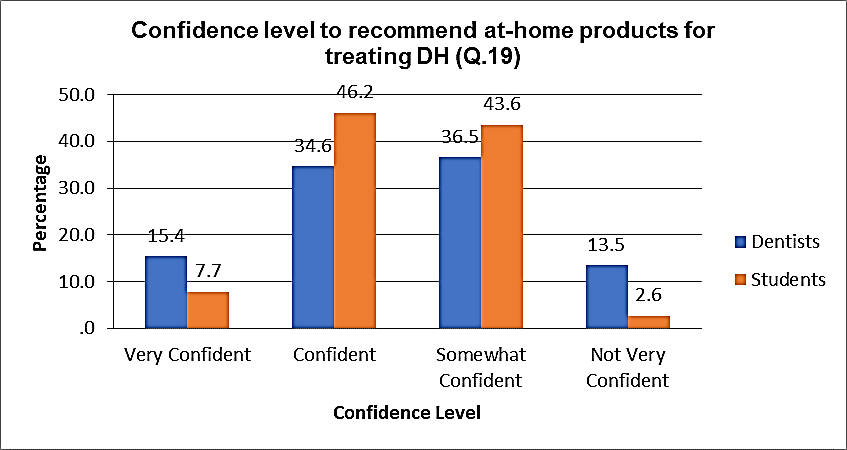
When asked to indicate how confident they were when recommending appropriate at-home materials to patients experiencing dentine hypersensitivity (Q.19) both dentists and students responded in the following manner. Dentists indicated that they either very confident (15.4%; n=8), confident (34.6%; n=18), somewhat confident (36.5%; n=19) or not very confident (13.5%; n=7) whereas the students indicated that they were either very confident (7.3%; n=3), confident (46.2%; n=18), somewhat confident (43.6%; n=17), or not very confident (2.6%; n=1) (Figure 4).
Figure 4: Dentist and student responses to how confident they were in recommending at-home desensitizing products.
When responding to whether patients had non-dental problems (such as stress etc.) in their daily life which may contribute to DH (Q.20) both dentists and students responded in a similar manner. For example, 48.1% (n=25) of dentists and 48.7% (n=19) of students indicated that in their opinion there was a non-dental problem associated with DH. 23.1% (n=12) of dentists and 23.1% (n=9) of students did not consider non-dental problems to be associated with DH. 28.8% of dentists (n=15) and 28.2% (n=11) of students indicated that they did not know.
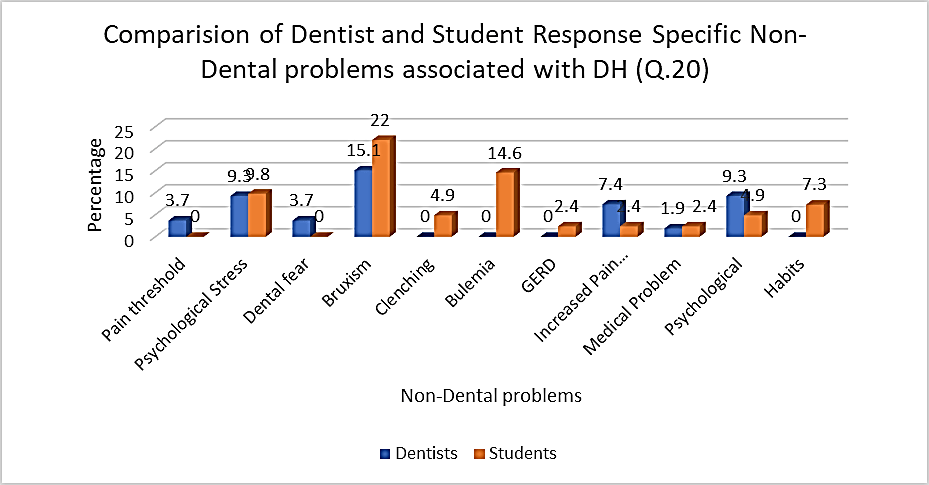
When asked to elaborate on whether there were any specific non dental problems associated with DH (Q.20) the four main responses for both dentists and students were as follows: 1) Bruxism (15.1 %; n=8)(22%; n=9), 2) psychological stress (9.3%; n=5)(9.4%; n=4), 3) other psychological issues (9.3%; n=5) (4.9%; n=2) and 4) increased pain perception (7.4%; n=4)(2.4%; n=1). Other responses which differed between the two groups were 1) Pain threshold (Dentists; 3.7%; n=2) and 2) Bulimia and GERD (Students; 17%; n=7) (Figure 5).
Figure 5: Comparison of Dentist and Student responses detailing specific non-dental problems associated with DH.
Q21. asked if their patients frequently complied with the professional advice provided for the treatment and management of DH. From the responses, the majority of dentists and students indicated that in their opinion their patients complied with the advice given to them (55.8%; n=29)(59%; n=23), 25% (n=13) of dentists and 10.3% (n=4) of students indicated that their patients were non-compliant with 19.2% (n=10) of dentists and 30.8% (n=12) of students indicated they did not know if their patients were compliant with the professional advice provided.
When asked if there was a need for additional information to prevent further occurrences of DH in the form of a leaflet etc., (Q.22) 34.6% (n=18) of dentists and 46.2% (n=18) of students indicated that there was a need for a patient leaflet. 65.4% (n=34) of dentists and 53.8% (n=21) of students indicated that there was no need for any further information regarding the prevention of DH. There were 36 responses from dentists and 35 from students (total 71 responses), of those respondents who recommended additional information for providing patient leaflets, the main responses from the dentists and students were 1) treatment options (14.8%; n=8)(20; n=8) and 2) knowledge about DH (15.1%; n=8)(14.6%; n=6). Other main options provided by the students were, 1) causes of DH (12.5%; n=5) and 2) reminders to patients (12.5%; n=5).
Discussion
The questionnaire used in the present study was based on a previous questionnaire study in the UK (DGG) originally translated from a questionnaire used in a study by Schuurs et al. [10-11]. The questionnaire has been subsequently validated in several studies both in the UK, Brazil, India, Kuwait and Greece [17-21]. (DH) is a recognized clinical condition that may have a profound impact on the Quality of life (QoL) of those who suffered from the problem [1-4]. Although there have been numerous questionnaire studies reporting on the prevalence of DH in patient populations which may be as high as 57%, data, however from the dentist’s perspective of the prevalence of DH is in the region of 10-25% [5-13]. Furthermore, previous studies or reviews have indicated that dentists may be uncertain about the aetiology, diagnosis and effective management of Dentine Hypersensitivity (DH) [10, 11, 14-16]. This lack of awareness or understanding regarding DH may therefore have an impact on how confident the dentist is in managing the condition and whether DH will be successfully treated to the patient’s satisfaction.
The current study together with a similar study by Pereira et al. in Brazil was unique in that it compared young dental students with their more experienced colleagues unlike the majority of other similar studies that evaluated the awareness and understanding of dentists with a wide range of clinical expertise [10, 11, 14-16, 18-23]. Interestingly in the present study the overall responses were comparable although in the assessment and subsequent management of DH the results indicated that dentists were more confident than the students. The results from the study should be viewed with some caution due to the relatively small sample size. The response rate was reasonable high compared to similar studies of this nature although this may be due to cooperation of both students and staff who were willing to take part. This is in contrast when collecting questionnaires from dental practitioners in general practice where other pressures may prevent them from participating in such studies [1, 10, 19].
When comparing the students and dentists’ responses to the various questions although there was a divergence of understanding and knowledge between the two groups nevertheless there were similarities in the respective responses. For example, 37.5% of students indicated that 10% of patients suffered from DH whereas 18.9% of dentists indicated that 25% of their patients suffered from DH. 18.9% of dentists indicating that DH was a serious problem for patients although 32.5% of students were not sure with both dentists (22.6%) and 27.5% of students indicating that DH lasted >12 weeks. There was also agreement between the dentists (66%) and students (62.5%) regarding the impact on the quality of life (QOL) with 51.1% (dentists) and 56.3% (students) indicating that this impact was moderate in nature [4]. The responses to questions relating to the aetiology, diagnosis and assessment of DH was reasonably consistent and in keeping with other published studies [17-20]. One of the problems that was highlighted in a previous study was the lack of understanding regarding the underlying mechanism of DH, however in the present study both 90.5% (n=38) of dentists and 76.9% (n=20) of students indicated that the hydrodynamic theory was the current accepted mechanism of action [14].
More recent studies have also confirmed this observation that clinicians are more aware of the underlying mechanisms initiating DH than previously reported [10, 19, 20]. The results of the present study also indicated that when asked how confident they were in the assessment and subsequent management of DH the dentist responses suggested that they were more confident than the students. Both dentists and students were relatively similar in their expressed confidence in recommending advice on DH and at-home desensitizing products. When asked whether there were any non-dental aspects (such as stress) that may impact on DH the responses where in general agreement although the responses on any specific factors were limited. Both dentists and students were split as to whether there was a need for any further information on DH in the form of leaflets.
Conclusion
The results of the present pilot study would suggest that in terms of knowledge and understanding of DH (e.g., hydrodynamic theory) both dentists (90.5%) and students (76.9%) were comparable although in the assessment and subsequent management of DH the results indicated that dentists were more confident than the students.
Acknowledgements
The Investigators would like to thank all the Staff and Students of The Royal London Dental Hospital, UK.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 06, May 2020Accepted: Thu 21, May 2020
Published: Thu 18, Jun 2020
Copyright
© 2023 D G Gillam. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.03.01
Author Info
Corresponding Author
D G GillamDepartment of Adult Oral Health, Barts and The London School of Medicine and Dentistry QMUL, London, UK
Figures & Tables
Table 1: Selected responses from Q.12 regarding an understanding of the aetiology of DH.
|
Q.12 The Aetiology of Dentine Hypersensitivity (Selected variables) |
Staff (n) |
Students (n) |
|
Exposed Dentine |
25 |
30 |
|
Gingival Recession |
18 |
18 |
|
Abrasion |
15 |
8 |
|
Fluid Movement |
9 |
8 |
|
Loss of Enamel |
4 |
8 |
|
Wrong (incorrect) brushing |
4 |
5 |
|
Periodontal Disease |
11 |
5 |
|
Enamel Fracture |
4 |
5 |
|
Erosion |
11 |
4 |
|
Attrition |
5 |
3 |
|
Bleaching Techniques |
2 |
3 |
|
Periodontal Treatment (post-operative sensitivity) |
5 |
2 |
|
Leaking Restoration |
3 |
2 |
|
Caries |
6 |
2 |
Table 2: Selected responses from Q.13 on what steps would you take to clinically diagnose a patient with DH.
|
Q.13 What steps would you take to clinically diagnose a patient with dentine hypersensitivity (Selected variables) |
Staff (n) |
Students (n) |
|
Clinical Sensitivity to Cold, |
32 |
30 |
|
Clinical Examination, |
30 |
22 |
|
Dentine Hypersensitivity History |
23 |
21 |
|
Vitality Test |
10 |
8 |
|
Aggravating factor |
5 |
7 |
|
Eliminate the cause of Dentine Hypersensitivity |
9 |
3 |
|
Assess Recession |
8 |
6 |
|
Take a radiograph |
7 |
5 |
|
Clinical Testing Not Specified |
7 |
4 |
|
Apply Bonding Agent |
1 |
5 |
|
Provision of a desensitising toothpaste |
1 |
5 |
|
Med History |
2 |
2 |
|
Diet History |
2 |
3 |
Table 3: Selected responses from Q.14 on what other dental conditions would you take into consideration when making a diagnosis of DH.
|
Q.14 what other dental conditions would you take into consideration when making a diagnosis of DH? (Selected variables) |
Staff (n) |
Students (n) |
|
Cracked Tooth Syndrome |
39 |
30 |
|
Fractured restoration |
41 |
29 |
|
Chipped teeth |
39 |
27 |
|
Dental Caries |
40 |
38 |
|
Periodontal Disease |
33 |
30 |
|
Post-operative sensitivity |
39 |
29 |
|
Marginal Leakage |
38 |
32 |
|
Pulpitis |
36 |
30 |
|
Palatogingival groove |
16 |
8 |
|
Bleaching Sensitivity |
45 |
25 |
|
None |
11 |
6 |
References
- Gillam DG, Seo H, Bulman JS, Newman HN (1999) Perceptions of dentine hypersensitivity in a general practice population. J Oral Rehabil 26: 710-714. [Crossref]
- Bekes K, John MT, Schaller HG, Hirsch C (2009) Oral health-related quality of life in patients seeking care for dentin hypersensitivity. J Oral Rehabil 36: 45-51. [Crossref]
- Gibson B, Boiko OV, Baker SR (2010) The everyday impact of dentine sensitivity: personal and functional aspects. Soc Sci Dent 1: 11-21.
- Gillam DG (2013) Current diagnosis of dentin hypersensitivity in the dental office: an overview. Clin Oral Investig 17: S21-S29. [Crossref]
- Irwin CR, McCusker P (1997) Prevalence of dentine hypersensitivity in a general dental population. J Ir Dent Assoc 43: 7-9. [Crossref]
- Rees JS (2000) The prevalence of dentine hypersensitivity in general dental practice in the UK. J Clin Periodontol 27: 860-865. [Crossref]
- Murray LE, Roberts AJ (1994) The prevalence of self-reported hypersensitive teeth. Arch Oral Biol 39: 129.
- Clayton DR, McCarthy D, Gillam DG (2002) A study of the prevalence and distribution of dentine sensitivity in a population of 17-58year-old serving personnel on an RAF base in the Midlands. J Oral Rehabil 29: 14-23. [Crossref]
- Cunha Cruz J, Wataha JC (2014) The Burden of Dentine Hypersensitivity. In: Robinson PG (ed). Dentine hypersensitivity: Developing a Person-centred Approach to Oral Health, Elsevier (A division of Reed Elsevier India Pvt. Ltd.) 34-44.
- Schuurs AH, Wesselink PR, Eijkman MA (1995) Dentists’ views on cervical hypersensitivity and their knowledge of its treatment. Endod Dent Traumatol 11: 240-244.
- Gillam DG, Bulman JS, Eijkman MA, Newman HN (2002) Dentists’ perceptions of dentine hypersensitivity and knowledge of its treatment. J Oral Rehabil 29: 219-225. [Crossref]
- Amarasena N, Spencer J, Ou Y, Brennan D (2010) Dentine Hypersensitivity - Australian dentists' Perspective Dentine Hypersensitivity. Aust Dent J 55: 181-187. [Crossref]
- Benoist FL, Ndiaye FG, Faye B, Bane K, Ngom PI et al. (2014) Knowledge of and management attitude regarding dentin hypersensitivity among dentists from a West African country. J Contemp Dent Pract 15: 86-91. [Crossref]
- Canadian Advisory Board on Dentin Hypersensitivity (2003) Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J Can Dent Assoc 69: 221-226. [Crossref]
- Orchardson R, Gillam DG (2006) Managing dentin hypersensitivity. J Am Dent Assoc 137: 990-998. [Crossref]
- Cunha Cruz J, Wataha JC, Zhou L, Manning W, Trantow M et al. (2010) Treating dentin hypersensitivity: Therapeutic choices made by dentists of the Northwest PRECEDENT network. J Am Dent Assoc 141: 1097-1105. [Crossref]
- Chana B, Kumar K, Gillam D (2012) Knowledge of UK Dental Professionals in Treating Dentine Hypersensitivity. IADR-SEA Annual Scientific Meeting November 3rd-4th (Poster Abstract).
- Pereira JC, Francisconi L, Calabria M, Hatton J, Honório H et al. (2013) Knowledge of Brazilian Dentists and Students in Treating Dentine Hypersensitivity. J Dent Res 92: 2193.
- Pereira R, Gillam DG, Bapatla S, Satyamurthy P (2018) Awareness of dentine hypersensitivity among general dental practitioners in Mumbai, India. J Odontol 2: 103.
- Gillam D, Dashti N, Chatzopoulou D (2019) A Survey of the Professional Opinions of Kuwaiti Dentists for the Treatment and Management of Dentine Hypersensitivity: A Questionnaire-based Study. Jacobs J Dentistry Res 5: 1-13.
- Exarchou C, Betsani I, Sakellari D, Chatzopoulou D, Gillam D (2019) Survey of Dentists in the Management of Dentine Hypersensitivity: A Questionnaire-based Study. Eur J Dent 13: 383-390. [Crossref]
- Izhar F, Nazir MA, Majeed A, Almas K (2019) A Study of Dentists about Their Knowledge and Practice of Dentine Hypersensitivity. Eur J Dent 13: 540-546. [Crossref]
- Kopycka Kedzierawski DT, Meyerowitz C, Litaker MS, Chonowski S, Heft MW et al. (2017) Management of Dentin Hypersensitivity by National Dental Practice-Based Research Network practitioners: Results from a questionnaire administered prior to initiation of a clinical study on this topic. BMC Oral Health 17: 41. [Crossref]
