Isolated Case of a Slot in the Anterior Leaflet of the Mitral Valve Revealed by Mitral Insufficiency
A B S T R A C T
Isolated mitral clefting is a rare congenital cause of mitral insufficiency. Surgical management is dominated by mitral plasty, which, despite a lack of robust studies, has produced satisfactory results.
Keywords
Isolated mitral cleft, mitral valve plasty, mitral valve, mitral insufficiency, congenital malformation
Introduction
Mitral cleft is a congenital malformation that is rare in itself and is a rare cause of mitral regurgitation (MI). First described in 1954 by Edwards et al.; it is called a true mitral cleft when it is not associated with inter-atrial communications (IAC) or interventricular communications (IVC) or does not occur in the context of an atrioventricular canal (AVC) [1].
We report the case of a 35-year-old woman admitted for treatment of severe MI due to isolated cleft of the anterior leaflet of the mitral valve.
Case Presentation
This is a 35-year-old patient who presented with NYHA stage II dyspnea, for whom a transthoracic ultrasound (TTE) was requested and revealed a severe MI associated with a mitral cleft. The patient was in good general condition, stable on the hemodynamic and respiratory levels. The physical examination was normal except for a systolic murmur heard at the mitral site of intensity 4/6.
|
·
Severe MI on mitral slot with thin and flexible leaflets: ERO = 73 mm²
VR = 132 ml Mitral ring = 30mm ·
Non-hypertrophied dilated LV with good systolic function: TDD= 65 mm/
TDDi=45.4 mm/m² EF=65% ·
LA dilated ELA= 40 cm² ·
Non-dilated RV with good longitudinal function Wave S=11 cm/s TAPSE=24
mm ·
Minimal TI with low probability of PHT: SPAP=28 mmHg ·
Fine and compliant IVC |
The TTE did not reveal other congenital malformations in particular (IAC, IVC, AVC, etc.). It is therefore an isolated mitral cleft located at the level of the anterior leaflet of the mitral valve (Figure 1). Based on the diagnosis of a severe mitral cleft MI with an undisturbed valve, the patient was admitted to the operating room for mitral plasty. Under general anaesthesia, creation of a vertical median sternotomy, installation of extracorporeal circulation (ECC) between an aortic cannula and two venous cannulas. Cardiac arrest was achieved using a cold blood cardioplegia solution administered anterogradely. The mitral valve was accessed through the LA via the sondergaard groove. Examination of the mitral valve revealed flexible, thin leaflets with a slit located on the A2 festoon (Figure 2).
Figure 1: A & B) TTE images in long axis parasternal section showing the mitral cleft and leak on colour doppler with dilation of the left atrium (LA).
Figure 2: Intraoperative image of the mitral cleft.
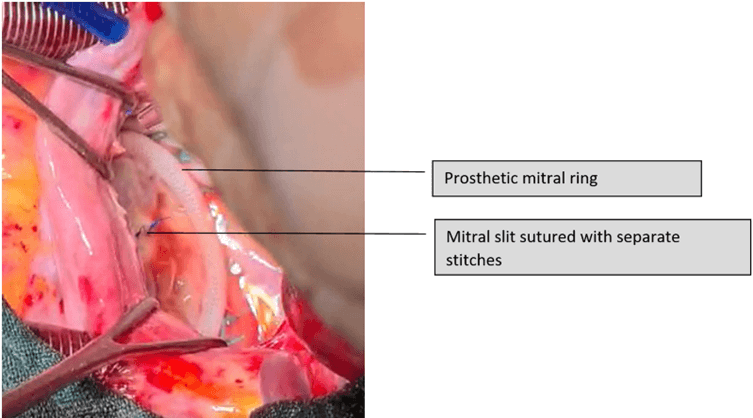
Once the lesion was well examined and other anomalies ruled out, a mitral plasty was performed, consisting of closing the slit with separate stitches with prolene 5/0 then placing a prosthetic ring to stabilize the mitral ring and strengthen the coaptation of the valve leaflets (Figure 3). ECC exit was simple under dobutamine 5 gamma/kg/min.
Figure 3: Intraoperative image after correction of the mitral cleft by plastic surgery.
The postoperative course was simple and an TTE check on postoperative day 60 showed minimal MI.
|
·
Non-leaking, non-stenosing mitral valve: minimal MI and average
gradient=5 mmHg ·
Non-dilated LV in moderate dysfunction EF=45% ·
Non-dilated RV with good longitudinal function ·
LA of limited size, free of thrombus ·
Doppler: normal filling pressures, minimal MI/TI/AI ·
Fine and compliant IVC |
Discussion
The mitral cleft (MC) is defined as an orifice or a “defect” which is due to a lack of fusion of the endocardial buds. It is preferentially located on the anterior leaflet of the mitral valve and more rarely on the posterior leaflet [2]. First described in 1954 by Edwards et al., MC has an incidence of 0.07% in ultrasound series [1, 3]. Subsequent descriptions have clearly separated isolated mitral clefts (IMC) which occur apart from other atrioventricular communications (IAC, IVC or AVC) and despite this distinction some authors still consider IMC to be a crude form of AVC [4]. Thus Sigfusson et al. suggested that MC occurring over a normal mitral valve should be classified separately from atrioventricular septal defects [5]. Finally, the nomenclature in congenital heart surgery characterized IMC as a cleft of the anterior mitral leaflet which is not associated with ostium primum IAC or any other form of atrioventricular communication [1].
Perier and Clausnizer et al. in their study revealed some anatomical specificities found in the IMC, contrary to what is observed in the AVC: the mitral annulus is in a normal position, the slot is oriented towards the LV outflow tract and the mitral and tricuspid valves are attached to the septum with a tricuspid valve located lower than the mitral valve [1].
IMC is recognized as a rare congenital cause of MI in adults. MI can be moderate to severe and TTE generally allows the diagnosis to be made, sometimes supplemented by transesophageal echocardiography (TOE). Management depends on the symptoms and severity of the MI. In 40% of cases it is surgical [6]. This surgical treatment is dominated by mitral plasty which usually consists of suturing separate stitches of the MC with placement of a mitral ring. Mitral annuloplasty is often performed if there is dilation of the mitral annulus. Furthermore, depending on the size of the MC, an autologous pericardium patch is used to close the gap and it is stabilized with artificial cords. Levinia E et al. opted for this technique [6]. Percutaneous treatment with Mitraclip under certain conditions can also be used for the closure of an IMC, this is what the study by Richard Cheng et al. reports [3].
The results of IMC surgery are rather rare, and those that are published come from small series or case reports [7]. The work of Rakesh M. Suri et al. report a 5-year morbidity and mortality rate of 67+-7% for mitral plasty versus 73+-9% after replacement, a difference which is not significant [8]. The reoperation rate is 3% with improved survival [8]. The case that we report actually benefited from a mitral plasty consisting of the closure of the IMC with separate points with 5/0 prolene and the installation of a prosthetic ring. The results at D60 are reassuring with minimal MI, regression of LV dilation but persistence of some moderate dysfunction.
Conclusion
IMC is a rare congenital anomaly causing MI whose surgical management is dominated by mitral plasty. The surgical results, although coming from small series, are rather reassuring. Larger studies and sufficient hindsight will certainly be required to confirm these results.
Author Contributions
Idrissa AM wrote the manuscript and all authors have read and approved the manuscript. Rhissassi J: managed the patient. Bouhdadi H, Wazren H, Briki J, Saadouni Y: co-author analysed the patient data and was a major contributor in writing the manuscript. Benlafqih C, Rhissassi J, Sayah R and Laaroussi M: supervised the manuscript.
Conflicts of Interest
None.
Funding
None.
Data Availability
Data sharing is not applicable to this article as no dataset were generated or analysed during the current study.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Article Info
Article Type
Case ReportPublication history
Received: Sat 30, Dec 2023Accepted: Mon 05, Feb 2024
Published: Fri 08, Mar 2024
Copyright
© 2023 Abdel Malick Idrissa. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2024.01.03
Author Info
Rhissassi J Abdel Malick Idrissa Bouhdadi H Wazaren H Briki J Saadouni Y El Idrissi A Benlafqih C Sayah R Laaroussi M
Corresponding Author
Abdel Malick IdrissaCardiovascular Surgery Department A, Ibn Sina University Hospital, Rabat, Morocco
Figures & Tables
|
·
Severe MI on mitral slot with thin and flexible leaflets: ERO = 73 mm²
VR = 132 ml Mitral ring = 30mm ·
Non-hypertrophied dilated LV with good systolic function: TDD= 65 mm/
TDDi=45.4 mm/m² EF=65% ·
LA dilated ELA= 40 cm² ·
Non-dilated RV with good longitudinal function Wave S=11 cm/s TAPSE=24
mm ·
Minimal TI with low probability of PHT: SPAP=28 mmHg ·
Fine and compliant IVC |
|
·
Non-leaking, non-stenosing mitral valve: minimal MI and average
gradient=5 mmHg ·
Non-dilated LV in moderate dysfunction EF=45% ·
Non-dilated RV with good longitudinal function ·
LA of limited size, free of thrombus ·
Doppler: normal filling pressures, minimal MI/TI/AI ·
Fine and compliant IVC |


References
1.
El
Hammiri A, Drighil A, Benhaourech S (2016) Spectrum of cardiac lesions
associated with isolated cleft mitral valve and thier impact on therapeutic
choices. Arq Bras Cardiol 106: 367-372. [Crossref]
2.
Minardi
G, Leonetti S, Bernardi L, Pulignano G, Guiseppe Pino P et al. (2010) An
isolated anterior mitral leaflet cleft: a case report. Cardiovascular
Uultrasound 8: 26. [Crossref]
3.
Cheng
R, Kar S, Siegel RJ, Nakamura M (2019) Cleft mitral leaflets and severe mitral
regurgitation: testing the limits of percutaneous mitral valve repair. Catheter
Cardiac Interv 93: 1161-1164. [Crossref]
4.
Abadir
S, Fouilloux V, Metras D, Ghez O, Kreitmann B et al. (2009) Isolated cleft of
the mitral valve: Distinctive features and surgical management. Ann Thorac Surg
88: 839-843. [Crossref]
5.
Kirali
K, Mansuroglu D, Ozen Y, Bozbuga NU, Tuncer A et al. (2003) Mitral cleft and
interartial septum defects: 15 years Results. Asian Cardiovasc Thorac Ann
11: 135-138. [Crossref]
6.
Zamfir
LE, Diena M, Cerin G, Hakimpour M, Benea CD et al. (2011) Mitral Insufficiency
due to an isolated anterior-leaflet cleft. Correction with an autologous
pericardial patch supported by artificial chrodae. Tex Heart Inst J 38:
243-245. [Crossref]
7. Hargiss BJ, Dearani JA, Stephens EH, Taggart NW (2022) Management of isolated, congenital anterior mitral valve cleft. World J Pediatr Congenit Heart Surg 13: 60-64. [Crossref]
8. Suri RM, Hartzell Schaff HV, Dearani JA, Sundt TM, Daly RC et al. Survival adventage and improved durability of mitral repair for leaflet prolapse subsets in the current era. Ann Thorac Surg 82: 819-827. [Crossref]
