Intraperitoneal Rupture of a Giant Hydatid Cyst of Liver- Can Emergency Placement of Intraperitoneal Drain Improve Patient Optimisation!
A B S T R A C T
Hydatid cyst remains a global health problem. Intraperitoneal hydatid cyst rupture is a life-threatening complication because it causes serious hemodynamic instability and allergic reactions. No clearly defined guidelines exist for dealing with ruptured cysts or intraperitoneal spillage, though emergency exploration remains the standard approach.
We present here a case of a 35 -year- old woman who developed spontaneous rupture of a Giant hepatic hydatid cyst. However, patient could not be taken up for emergency surgery in view of very poor chest condition. She was managed by placement of an intra peritoneal drain and lavage with hypertonic saline. Subsequently, patient underwent two surgeries for definitive treatment of the giant hydatid cyst. At one year of follow- up, patient has no evidence of any recurrent disease. Intraperitoneal drain placement and lavage with hypertonic saline may be considered an option to contain peritoneal implantations while patient is being optimised for exploration.
Keywords
Giant hydatid cyst, spontaneous rupture, residual cavity, intraperitoneal drain
Introduction
Hydatid cyst or Cystic Echinococcosis is a systemic Zoonosis caused by the larval stage of Echinococcal tapeworm. Liver (50-70%) and Lungs (20-30%) are the predominant organs involved, though it can involve any organ of the body [1, 2]. Intrabiliary rupture (5%-25%), allergic reactions (1%-25%) and Intraperitoneal rupture (0.9%-16%) are the three most common complication. Risk factors for rupture include young age, cyst diameter (>10 cm), and superficial localization [3]. Intracystic pressure increases with increasing cyst dimension. When intracystic pressure increases to more than 50 cmH2O, spontaneous or traumatic rupture risk also increases. Clinical signs and symptoms of intraperitoneal cyst ruptures vary widely among patients. While 16.7%-25% of patients with hydatid cyst rupture develop minor allergic reactions, such as urticaria and macular eruption, 1%-12.5% of patients develop more severe allergic reactions such as peripheral edema, syncope, and anaphylaxis. The life-threatening anaphylactic shock incidence rate is approximately 1.4% [3].
Most patients who have intraperitoneal rupture present to the emergency with symptoms of severe abdominal pain, hypotension, tachycardia, and allergic reactions. US is the most common radiologic tool for diagnosis. If patients are hemodynamically stable, contrast-enhanced CT may be used. The sensitivity of US and CT is 85% and 100%, respectively [3].
After confirming the diagnosis of intraperitoneal rupture, medical treatment should be initiated with fluid resuscitation for stabilizing hemodynamic status and treating anaphylactic reactions with corticosteroids, antihistaminic, and vasopressor drugs. Emergency surgery remains the treatment of choice in Intra peritoneal rupture of Hydatid cyst [2-5]. Here we share our experience of a case of giant hydatid cyst of liver with spontaneous rupture and challenges faced in its management.
Case Report
A 35-year- old lady was admitted with complaints of pain and swelling in the right upper abdomen since 2 years. On examination she had a smooth, non-tender 10x10 cm lump in the right upper abdomen, which was dull on percussion. There was markedly decreased air entry in the lower zone of right lung, on work up, Ultrasound (USG) abdomen revealed a unilocular cyst with hydatid sand suggestive of liver hydatid cyst. However, her hydatid serology was negative. Patient was planned for exploration under high risk in view of poor pulmonary functions. Patient denied consent and was discharged on request on Tab Albendazole 400 mg x BD for one month and advised follow up.
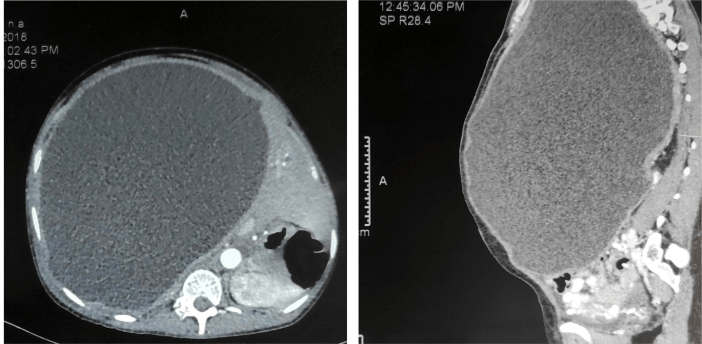
The patient presented 3 years later with same complaints and a poor general condition (BMI 16). Examination revealed a huge cystic lump occupying the entire abdomen. There was minimal air entry in her right lung. Investigations revealed suboptimal PFT and a positive hydatid serology, Contrast Enhanced CT Scan (CECT) abdomen showed a well-defined hypodense lesion, 20x23x32cm in size in right lobe of liver with internal echo and wall thickness of 3mm. There was no evidence of daughter cyst. An impression of Hepatic hydatid cyst with mass effect was made (Figure 1).
Figure 1: A) Axial view & B) Sagittal view-showing the giant hydatid cyst with mass effect.
She developed spontaneous rupture of the cyst on day 6 of admission and developed pain abdomen, vomiting, urticaria and hypotension. She was stabilised by intravenous fluids and antiallergic medication. Due to poor chest condition (poor PFT and active respiratory tract infection), her emergency laparotomy was deferred. Instead a USG guided Intra peritoneal drain was placed, which drained 3000 ml of turbid hydatid fluid stat, followed by 400-500ml/ day. While waiting for laparotomy, patient received daily peritoneal lavage with 200 ml of hypertonic saline (3%) for next one week. Subsequently, Exploratory laparotomy was done through a midline incision. Though cyst had much shrunk in size, no obvious site of cyst rupture was seen. There was no evidence of any peritoneal implantation. Cystectomy was done and a large residual cavity which was extending till mid thorax was closed over a drain. She received further washes with hypertonic saline through the drain for 1 week and subsequently discharged in stable condition.
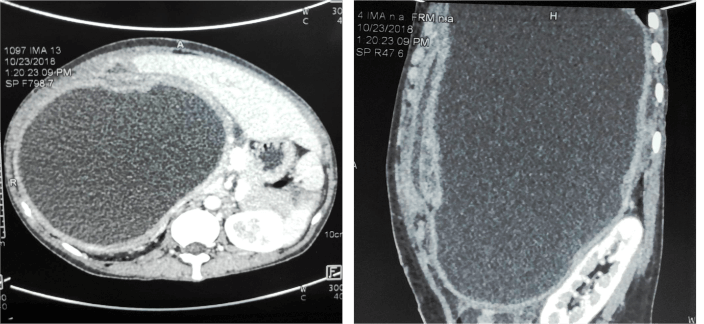
One month later she presented again with complaints of high-grade fever for 15 days and pus discharge from the drain site, and a rapidly increasing swelling of the abdomen. Examination of the abdomen revealed a tense, tender cystic lump occupying the whole abdomen again. Diagnosis of a recurrent cyst with secondary infection was made. CECT abdomen showed by a well-defined peripherally enhancing, hypodense fluid collection 23x17x15cm replacing right lobe of liver. There was an 8mm breach in the wall of lesion inferiorly, leading to fluid collection in right anterior abdominal wall (Figure 2).
Figure 2: A) Axial view & B) Sagittal view- Showing giant hydatid cyst with fluid collection in anterior abdominal wall.
This time exploration was done through a right thoraco-abdominal incision and complete Pericystectomy, with cholecystectomy, was done. No cysto Biliary Communication was found. Patient had an uneventful postoperative recovery. She continued on tab albendazole for next 6 months. A follow up CECT abdomen after one year reveals partially visualised right lobe of liver with left lobe hypertrophy and no recurrence of liver or peritoneal hydatid cyst.
Discussion
The aims of emergent surgical treatment of intraperitoneal rupture of hydatid cyst include prevention or minimization of anaphylactic reactions in the early term and prevention of the development of long-term secondary peritoneal hydatidosis. There is no consensus in the literature about surgical treatment options for intraperitoneal cyst rupture [3]. The operative procedures, either radical or conservative, are performed based on the patient’s condition, and the surgeon’s experience.
Though, Surgery is considered standard approach in ruptured hydatid cyst. To minimize morbidity and mortality, patients should be hemodynamically stabilized before surgery [3]. Also, surgery may not be feasible due to various constraints like lack of availability of OT, logistics and other resources, especially as prevailing in low and middle-income countries frequently. This makes performing Intraperitoneal drainage with scolicidal lavage, a bridging procedure, until patient is optimised, and resources are available for performing surgery. It also helps to reduce the risk of secondary hydatidosis by reducing the seeding of hydatid scolices and also, the load of the daughter cysts.
Hypertonic saline (3%-10%-15%-30%), is the most commonly used scolicidal agent for wash of peritoneal cavity though use of other agents such as silver nitrate (0.5%), cetrimide, chlorhexidine, cetrimide plus chlorhexidine (1.5%/0.15%), hydrogen peroxide (1.5%-3%), povidone iodine (10%-50%), or ethyl alcohol (70%-95%) is also described. Each solution has a different time frame for possible scolicidal effects [3]. Derici et al. reported that hypertonic saline is not appropriate because it may damage the peritoneal surfaces and may cause hypernatremia. However, we did not encounter any significant dyselectrolytemia or any other complications with the use of this solution. Additionally, profuse peritoneal lavage with hypertonic saline is recommended mandatory for preventing intra-abdominal recurrence of hydatid disease.
Management of Giant Residual cavities is another area of debate. Literature mentions various options like Marsupialisation, External drainage, Capitonnage, Introflexion, and Omentopexy [6]. Though External Drainage is considered a management option for giant residual cavity, it is reported to have with higher morbidity due to higher incidence of complications like secondary infection etc, as was seen in our case too [7, 8].
Conclusion
Intra peritoneal drain placement can be considered as a ‘bridging procedure’ before taking a case of Ruptured Hydatid Cyst for Surgery. Management of Giant Residual Cavity is a challenge. External drainage should be avoided, and also more prospective comparative studies are needed to establish an evidence-based protocol for its management.
Acknowledgements
The authors thank their colleagues for the work behind this case report.
Conflicts of Interest
None.
Funding
None.
Consent
Informed consent taken from the patient.
Article Info
Article Type
Case ReportPublication history
Received: Fri 28, Feb 2020Accepted: Mon 16, Mar 2020
Published: Fri 20, Mar 2020
Copyright
© 2023 Praveenkumar M. Patil. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.02.02
Author Info
Nishtha and Navneet Kaur Praveenkumar M. Patil
Corresponding Author
Praveenkumar M. PatilDepartment of Surgery, University College of Medical Sciences and GTB Hospital, New Delhi, India
Figures & Tables
References
- Turgut AT, Altın L, Topçu S, Kılıçoğlu B, Altınok T et al. (2007) Unusual imaging characteristics of complicated hydatid disease. Eur j Radiol 63: 84-93. [Crossref]
- Ozturk G, Aydinli B, Yildirgan MI, Basoglu M, Atamanalp SS et al. (2007) Posttraumatic free intraperitoneal rupture of liver cystic echinococcosis: a case series and review of literature. Am J Surg 194: 313-316. [Crossref]
- Akbulut S, Ozdemir F (2019) Intraperitoneal rupture of the hydatid cyst: Four case reports and literature review. World J Hepatol 11: 318-329. [Crossref]
- Arikanoglu Z, Taskesen F, Aliosmanoğlu İ, Gul M, Cetincakmak MG et al. (2012) Spontaneous intraperitoneal rupture of a hepatic hydatid cyst. Int surg 97: 245-248. [Crossref]
- Mouaqit O, Hibatallah A, Oussaden A, Maazaz K, Taleb KA (2013) Acute intraperitoneal rupture of hydatid cysts: a surgical experience with 14 cases. World J Emerg Surg 8: 28. [Crossref]
- Salemis NS (2008) Giant hydatid liver cyst. Management of residual cavity. Ann hepatol. 7: 174-176. [Crossref]
- Bahar MM, Nooghabi AJ, Hamid A, Amouzeshi A, Jangjoo A (2014) Study of treatment results and early complications of tube drainage versus capitonnage after the unroofing and aspiration of hydatid cysts. Asian J surg 37: 195-199. [Crossref]
- Ozacmak ID, Ekiz F, Ozmen V, Isik A (2000) Management of residual cavity after partial cystectomy for hepatic hydatidosis: comparison of omentoplasty with external drainage. Eur J Surg 166: 696-699. [Crossref]
