Intraoperatively Diagnosed Double Cystic Duct During Laparoscopic Cholecystectomy: A Case Report of a Surgical Dilemma for the Operating Surgeons
A B S T R A C T
Introduction and Importance: A double cystic duct with a single gallbladder is one of the extremely uncommon variations of the cystic duct and only a few cases were reported in literature.
Case Presentation: A 33-year-old female, with an unremarkable medical history, presented to the emergency department with a 2-day history of right upper quadrant abdominal (RUQ) pain. The abdominal pain was gradually increasing in intensity radiating to the back and was associated with anorexia and multiple episodes of vomiting. Abdominal examination revealed RUQ pain and tenderness. Abdominal ultrasonography was performed, showing a markedly distended gallbladder with evidence of a few calculi one of which was impacted at the neck. laparoscopic cholecystectomy was done within 2 days of admission during which another luminal structure was identified that suggested a double cystic duct.
Clinical Discussion: Anomalies of the biliary tree are common with the classical anatomical picture presenting in only 33% of cholecystectomy cases. However, the presence of a double cystic duct is a rare variation, especially in the case of a single gallbladder. The identification of such anomaly can be achieved preoperatively using imaging modalities or it can be identified during the surgical procedure itself. such identification reduces the chances of postoperative comorbidities.
Conclusion: Pre-operative identification of biliary tract anomalies by different imaging modalities is limited. Hence the importance of cautiousness and achieving a proper critical view of safety intra-operatively to prevent possible complications intra- and post-operatively. Our case report emphasizes the diagnostic and surgical challenges of the double cystic duct.
Keywords
Double cystic duct, common bile duct, cholecystectomy, case report
Introduction
The biliary tree anatomical abnormalities are predictors of high susceptibility to ductal injuries and surgical complications. Of these anomalies, congenital defects of the extrahepatic biliary duct system are documented [1]. The development of a double cystic duct with a gallbladder is one of the extremely uncommon variations of the cystic duct [1, 2]. Statistically, only a few cases were reported in the literature [2]. The preoperative diagnosis of the abnormal anatomy of the cystic duct is challenging [2, 3].
Here we highlight a 33-year-old female patient, who performed laparoscopic cholecystectomy, and duplication of the cystic duct was detected intraoperatively.
Case Presentation
A 33-year-old female, with an unremarkable past medical history, presented to the emergency department with 2 days of history of right upper quadrant (RUQ) abdominal pain. The abdominal pain was gradually increasing in intensity radiating to the back and was associated with anorexia and multiple episodes of vomiting. Initially, the vomitus content was food then progressed to yellowish secretions.
There were no changes in bowel habits or urinary manifestations. No evidence of fever or jaundice was documented. Physical examination revealed an alert, conscious, and oriented patient. Upon the abdominal examination, there was RUQ pain and tenderness, epigastric tenderness, and negative Murphy’s sign. No rebound tenderness or abdominal distention was detected. Laboratory investigations of the patient are mentioned in (Table 1). A plain abdominal X-ray showed insignificant findings (Figure 1).
Figure 1: Chest and abdominal X-ray.
Table 1: Patient’s vital
signs and laboratory investigations on admission
|
Patient’s vital
signs |
Hematology |
Coagulation |
|
GCS 15/15 |
WBC 12.8 |
PT 13.70 |
|
BP 122 /80 mmHg |
Hb 139 |
PT-INR 1.060 |
|
HR 72 bpm |
Platelets 323 |
APTT-A 26.40 |
|
RR 19 |
Neutrophils 10.80 |
APTT-A
Ratio 0.82 |
|
SPO2 99 % on room air |
Lymphocytes 1.68 |
Amylase 98 |
|
Body
temperature 37 o C |
Monocytes 0.29 |
Albumin 45.5 |
|
Total
bilirubin 10.8 |
Eosinophils 0.01 |
ALT 19 |
|
Direct
bilirubin 2.11 |
Basophils 0.01 |
AST 21 |
|
Indirect
bilirubin 9 |
Creatinine 39 |
ALK-PHOS 50 |
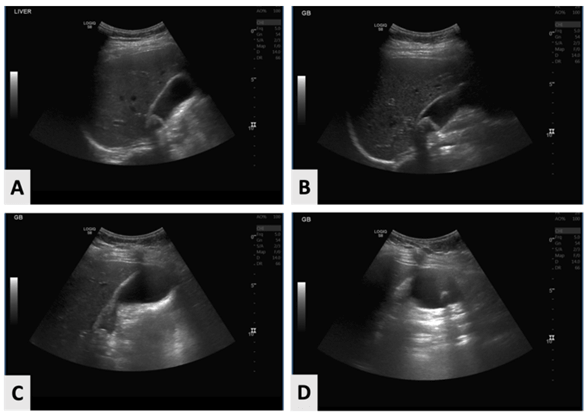
Figure 2: Abdominal ultrasonography. A-D) Showing inflamed gallbladder.
Abdominal ultrasonography was performed, showing a markedly distended gallbladder with evidence of a few calculi. One of the detected calculi was impacted at the neck, measuring 2.4 cm. Also, mild wall thickening and fatty liver were identified, and no pericystic fluid was noted (Figure 2). At this point, acute cholecystitis was diagnosed, and laparoscopic cholecystectomy was decided.
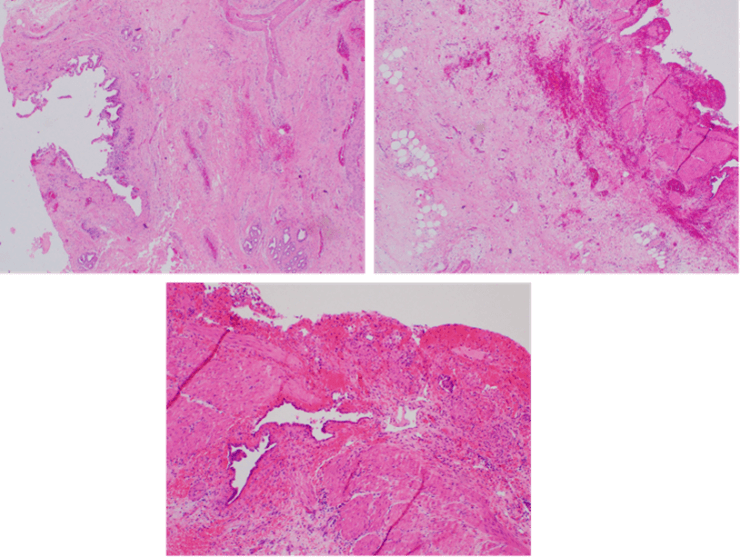
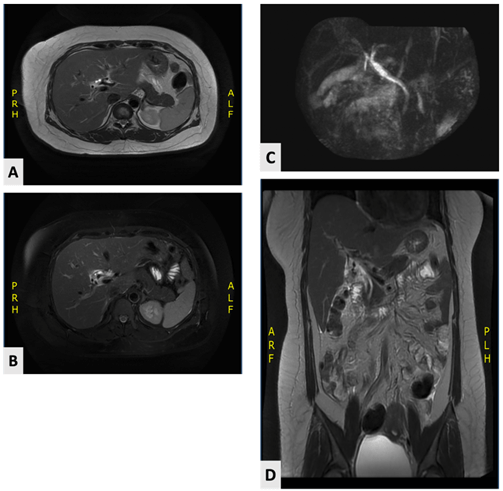
During the procedure, adhesions were noticed over the gallbladder bed, meticulous dissection was done using diathermy and blunt dissection as well, through which a critical view of safety was achieved. Surprisingly, three structures were identified to be connected to the gallbladder, one of which was a cystic artery that was adjacent to the right hepatic artery creating a challenge to separate it from the liver bed, the other luminal structure was seen arising between the rt hepatic duct and the gallbladder. Lastly, a third structure was arising between the GB and the CBD. The decision was to safely clip using hemilock over the two luminal structures connected to the biliary tree. Furthermore, an endoclip is placed over the cystic artery achieving hemostasis. Grossly, the resected inflamed gallbladder measured 10 × 4 cm with a wall thickness of 0.5 cm. The specimen was sent for a histopathology study that revealed acute on top of chronic cholecystitis with reactive atypia (Figure 3). MRCP arranged, revealed that the gallbladder was surgically removed with no definite abnormalities (Figure 4). The postoperative period was uneventful and discharged home on postoperative day 2 with normal labs.
Figure 3: Histopathology slides.
Figure 4: MRCP showed unremarkable study. A & B) Axial views. D) Coronal view.
Discussion
Anomalies of the biliary tree are common with the classical anatomical picture presenting in only 33% of cholecystectomy cases [4]. The first records of anatomical anomalies of the gallbladder date back to 1926 [5]. However, the presence of a double cystic duct is a rare variation especially in the case of a single gallbladder as it is associated with a double gallbladder 80% of the time [1, 4, 6]. Double cystic ducts can be classified into three different types according to the configuration of the ducts [1, 4-7]. The first type is the (Y) variant. In this type of configuration, both the primary and the accessory cystic ducts unite to form a common channel that drains into the common hepatic duct. The second type that the current patient had is the (H) variant in which the accessory cystic duct drains separately into either the left, right, or common hepatic duct (CHD) [1, 4-7]. The third type variant is the trabecular type, in which the accessory cystic duct enters the substance of the liver directly [1, 4-7].
Identifying anomalies in the biliary duct system plays an important role in avoiding postoperative complications. Imaging modalities such as magnetic resonance cholangiopancreatography (MRCP) and helical CT facilitate the detection of any anomalies preoperatively and intraoperative confirmation can be achieved by the use of cholangiography [3]. However, preoperative diagnosis of double cystic duct was only reported in only three cases found in the literature with the majority of cases being diagnosed intraoperatively [1, 4-7].
Our case was a double cystic duct originating from a single gallbladder drained by a separate opening to the right hepatic duct. The diagnosis was made intraoperatively. Reporting such cases highlights the importance of identifying anatomical variants such as double cystic duct in order to avoid postoperative morbidity such as bile leak.
Conclusion
Pre-operative identification of biliary tract anomalies by different imaging modalities is limited. Hence the importance of cautiousness for any variations intra-operatively to prevent possible complications intra- and post-operatively. Our case report emphasizes the diagnostic and surgical challenges of the double cystic duct.
Funding
None.
Ethical Approval
Not applicable.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Research Registration
Not applicable.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
Author Contributions
Ali Alenezi: Paper writing, editing, and literature review. Athary Saleem: Paper writing, editing, and manuscript drafting. Hamad Alajmi: Paper writing and editing. Dalal Al Husainan: Paper writing and editing. Odai Al Shadifat: Picture editing and assisting in surgery. Ahmed Bader: Performed surgery, supervision, and final approval.
Guarantor
Ali Alenezi, M.D., General Surgery Department, Al-Adan Hospital, Kuwait. E-mail: ali_a.alenezi@hotmail.com.
Article Info
Article Type
Case ReportPublication history
Received: Wed 06, Mar 2024Accepted: Tue 02, Apr 2024
Published: Tue 16, Apr 2024
Copyright
© 2023 Athary Saleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2024.01.04
Author Info
Ali Alenezi Athary Saleem Hamad Alajmi Dalal Al Husainan Odai Al Shadifat Ahmed Bader
Corresponding Author
Athary SaleemNeurosurgery Department, Jaber Al Ahmad Hospital, State of Kuwait
Figures & Tables
Table 1: Patient’s vital
signs and laboratory investigations on admission
|
Patient’s vital
signs |
Hematology |
Coagulation |
|
GCS 15/15 |
WBC 12.8 |
PT 13.70 |
|
BP 122 /80 mmHg |
Hb 139 |
PT-INR 1.060 |
|
HR 72 bpm |
Platelets 323 |
APTT-A 26.40 |
|
RR 19 |
Neutrophils 10.80 |
APTT-A
Ratio 0.82 |
|
SPO2 99 % on room air |
Lymphocytes 1.68 |
Amylase 98 |
|
Body
temperature 37 o C |
Monocytes 0.29 |
Albumin 45.5 |
|
Total
bilirubin 10.8 |
Eosinophils 0.01 |
ALT 19 |
|
Direct
bilirubin 2.11 |
Basophils 0.01 |
AST 21 |
|
Indirect
bilirubin 9 |
Creatinine 39 |
ALK-PHOS 50 |
References
1. Abdelsalam AM,
Elansary AMSE, Mohamed AMI (2021) A case report of double cystic duct during
laparoscopic cholecystectomy in patient with chronic calcular cholecystitis. Int J Surg Case Rep 78: 116-119. [Crossref]
2. Lim S, Kim CH, Paik
KY, Kim W (2020) Double cystic duct without being aware of the anatomic anomaly
during laparoscopic cholecystectomy: The first case of reverse Y type anomaly. Hepatobiliary Pancreat Dis Int 20: 201-202. [Crossref]
3. Fujii A, Hiraki M,
Egawa N, Kono H, Ide T et al. (2017). Double cystic duct preoperatively
diagnosed and successfully treated with laparoscopic cholecystectomy: a case
report. Int J Surg Case Rep 37: 102-105. [Crossref]
4. Huston TL, Dakin GF
(2008) Double cystic duct. Can J Surg
51: E9-E10. [Crossref]
5. Munie S, Nasser H,
Go PH, Rosso K, Woodward A (2019) Case report of a duplicated cystic duct: a
unique challenge for the laparoscopic surgeon. Int J Surg Case Rep 56:
78-81. [Crossref]
6. Salih AM, Kakamad FH, Mohammed SH, Salih RQ, Habibullah IJ et al. (2017) Double cystic duct, a review of literature with report of a new case. Int J Surg Case Rep 38: 146-148. [Crossref]
7. Nakasugi H, Kobayashi S, Sakamoto K, Inayoshi T, Matsumura M et al. (1995) A case of double cystic duct with cholecystolithiasis treated by laparoscopy. Journal of Hepato‐Biliary‐Pancreatic Surgery 2: 68-71.
