Intestinal Ameboma Involving the Jejunum: First Case Reported in Medical Literature
A B S T R A C T
We present the case of a 58-years-old caucasian male who was hospitalized in our hospital with an early diagnosis of a jejunal tumor. However, all the instrumental and laboratory testing conducted were inconclusive and a preoperative diagnosis was not established. Patient was scheduled for surgery and en-bloc resection of the jejunal mass was performed. Microscopic analysis of the specimen reported the presence of intense mixed lympho-granulocytic inflammatory infiltrate of the mucosa associated with entamoeba parasites and a diagnosis of intestinal ameboma was ruled out. Ameboma is a rare complication of chronic amoebic colitis. usually found in the cecum and ascending colon. To our knowledge, this is the first case of an intestinal ameboma involving the jejunum to be reported in medical literature.
Keywords
Emergency surgery, laparoscopy, ameboma, intestinal amoebiasis
Introduction
We present the case of a 58-years-old caucasian male who was admitted in our surgical department for abdominal pain, anorexia, bloody diarrhea and fever. During hospitalization, the patient underwent a CT scan of the abdomen which demonstrated a tumor-like abdominal mass of 9.4 cm in diameter involving the jejunum. However, all the instrumental and laboratory testing conducted were inconclusive and a preoperative diagnosis was not established. According to the radiological aspect suspicious for an intestinal tumor, we decided to schedule the patient for surgery and en-bloc resection of the jejunal mass was performed. Microscopic analysis of the specimen reported the presence of intense mixed lympho granulocytic inflammatory infiltrate of the mucosa associated with Entamoeba histolytica parasites and a diagnosis of jejunal ameboma was ruled out. Ameboma is a rare complication of intestinal amebiasis and it occurs as a mass of granulation tissue usually found in the cecum and ascending colon which is clinically and radiologically indistinguishable from a colonic tumor. To our knowledge, this is the first case of an intestinal ameboma involving the jejunum to be reported in medical literature so far.
Case Report
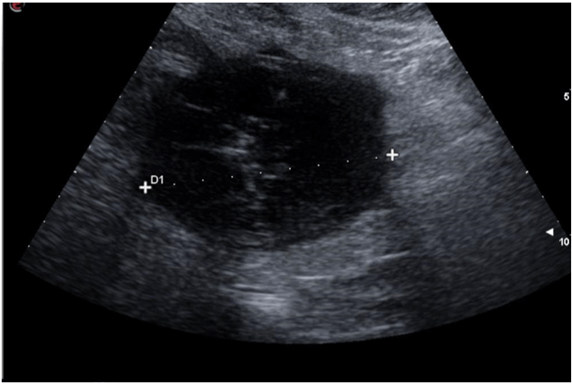
Our case report involves a 58-years-old caucasian obese male affected by hypertension, who was admitted to our emergency department (E.D.) for anorexia, abdominal pain, bloody diarrhea and fever. Home treatment with empiric antibiotics (amoxicillin/clavulanic acid) was reported to be without benefit. Our patient lives in Italy and in his medical history denies travels in exotic and foreign countries. On clinical examination, the abdomen was soft with a mild tenderness in the left quadrant. Complete blood count revealed leukocytosis (WBC 9.36 × 10 g/L) with neutrophilia (neutrophil 6,27 × 10 g/L) and increased level of C-reactive protein (CRP 167 g/L); eosinophils count and haemoglobin level were in range. Abdominal ultrasound (Figure 1) showed an hypoechogenic mass of 88 mm × 90 mm in diameter which was described as an abdominal abscess. Contrast CT scan of the abdomen (Figure 2) revealed an encapsulated oval mass of 9.4 cm in diameter with an inhomogeneous content and gross calcification, highly suggestive for a neoplastic mass.
Figure 1: Abdominal ultrasounds imagine showing an hypoechogenic mass of 88 × 90 mm in diameter.
Figure 2: Contrast CT scan imagine showing an encapsulated mesenteric mass with 9.4 cm in diameter with gross calcification.
Patient was admitted to our general surgery department for further investigations. During hospitalization, chromogranin A and LDH levels were tested in suspicion of a neuroendocrine tumor (NET) and an intestinal lymphoma respectively, both tests were negative. Stool tests for parasites and infectious diarrhea were also negative. A needle aspiration biopsy of the mass was performed, and the cytological examination showed an inflammatory nonspecific infiltrate.
Despite the absence of a preoperative histological diagnosis, we decided to schedule the patient for an explorative laparoscopy in consideration of the highly suspicious radiological aspect of intestinal tumor. In the absence of clear levels of cleavage between the jejunal mass and the visceral peritoneum, surgery was converted with a laparotomic approach. En-bloc resection of the jejunal mass was performed (Figures 3a and 3b) and the intestinal tract was reconstructed with a side-to-side intestinal anastomosis. Microscopic analysis of the specimen reported the presence of intense mixed lympho granulocytic inflammatory infiltrate of the mucosa associated with Entamoeba histolytica parasites and a diagnosis of intestinal ameboma was ruled out. Patient was treated with i.v. injections of metronidazole 500 mg three times a day for 7 days. The postoperative course was without complications and the patient was discharged after 10 days of hospitalization.
Figure 3 (A & B): Imagines from operating theatre showing the diameter of the mass.
Discussion
According to our case report, the patient sought medical attention for unspecific symptoms like abdominal pain, fever and diarrhea. These clinical manifestations can be either attributable to an infectious disease or a gastrointestinal tumor. An early diagnosis of a tumor-like abdominal mass was initially supported by radiological findings, as the abdominal CT scan showed an encapsulated roundish mass with gross calcification of 9.4 cm in diameter involving the jejunum. The presence of calcifications within the tumor mass was suggestive of gastrointestinal stromal tumor (GIST). The diagnosis of neuroendocrine tumor (NET) was also taken under consideration due to the fact that the abdominal mass originated from the small intestine and the clinical presentation resembled a carcinoid syndrome with abdominal pain and diarrhea [2]. A diagnosis of intestinal lymphoma was also postulated, although the LDH test was in range [3]. An U.S. guided needle aspiration biopsy was performed in order to acquire a cytological preoperative diagnosis. However, the cytological examination showed inflammatory nonspecific infiltrate which was inconclusive for a clear diagnosis. Therefore, we decided to schedule the patient for surgical exploration. Histologic examination of the entire specimen reported the presence of intense mixed lympho-granulocytic inflammatory infiltrate of the mucosa associated with Entamoeba histolytica parasites and a diagnosis of jejunal ameboma was ruled out.
Entamoeba histolytica is commonly an asymptomatic disease and only 4-10% of the people affected develop symptoms. The gastrointestinal tract is often involved with subacute onset and common clinical manifestations are diarrhea and abdominal pain. Entamoeba histolytica infection of the intestines is referred to as amebiasis or amebic colitis. Occasionally, amoebic colitis can be fulminant, with acute abdominal pain, fever, leukocytosis, bloody diarrhea and peritonitis. Rarely, the infection can be chronic and can mimic an inflammatory bowel disease (IBD) with persistent diarrhea, weight loss, anorexia, lethargy, low-grade fever and abdominal pain. A rare complication of chronic intestinal amebiasis is ameboma. This complication appears as a mass of granulation tissue usually found in the cecum and ascending colon and it’s clinically and radiologically indistinguishable from colonic tumor [4, 5]. Identification of Entamoeba histolytica in stool samples allows a prompt diagnosis, however, in our case report, patient stool examination was negative. Entamoeba histolytica may be undetectable in stool and an endoscopic mucosal biopsy of colonic ameboma is required to rule out the diagnosis [6-8]. In our case, endoscopic biopsy was not feasible due to the anatomic location of the mass.
Ameboma of the small bowel has to be considered a rare manifestation of intestinal amoebiasis and a high level of suspicion is required to establish a prompt diagnosis [9]. To our knowledge, this is the first case of jejunal ameboma to be reported in medical literature so far.
Competing Interests
None.
Author Contributions
Nisi Antonella, Marini Michele, Fulco Emanuele, Pelfini Elisa, Vescovi Lorenzo, Piazzini Antonio, Metelli Flavio, Sonzogni Aurelio and Armellini Elia were involved in the clinical management of the patients and drafted the manuscript. Vescovi Lorenzo, Costanzo Antonio and Nisi Antonella were involved in the surgical management of the patients. All authors read and approved the final manuscript.
Acknowledgements
Special mansion goes to dr Francesco Locati, General Manager of Bolognini Hospital, and to dr Pietro Imbrogno, Medical Director of Bolognini Hospital, for their support and assistance in redacting the current article.
Article Info
Article Type
Case ReportPublication history
Received: Fri 09, Jun 2023Accepted: Mon 10, Jul 2023
Published: Mon 31, Jul 2023
Copyright
© 2023 Nisi Antonella. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2023.03.01
Author Info
Nisi Antonella Michele Marini Fulco E. Pelfini E. Vescovi L. Costanzo A. Caprioli M. Flavio M. Elia Armellini Sonzogni A. PatellI G. Piazzini Albani A.
Corresponding Author
Nisi AntonellaGeneral Surgery Postgraduate School, University of Milano, Italy
Figures & Tables


References
1. Von Mehren M,
Joensuu H (2018) Gastrointestinal Stromal Tumors. J Clin Oncol 36:
136-143. [Crossref]
2. Pinchot SN, Holen
K, Sippel RS, Chen H (2008) Carcinoid tumors. Oncologist 13: 1255-1269.
[Crossref]
3. Wong MT, Eu KW
(2006) Primary colorectal lymphomas. Colorectal Dis 8: 586-591. [Crossref]
4. Nagata N, Shimbo T,
Akiyama J, Nakashima R, Nishimura S et al. Risk factors for intestinal invasive
amebiasis in Japan, 2003-2009. Emerg Infect Dis 18: 717-724. [Crossref]
5. Li J, Cui Z, Li X,
Zhang L (2021) Review of zoonotic amebiasis: Epidemiology, clinical signs,
diagnosis, treatment, prevention and control. Res Vet Sci 136: 174-181.
[Crossref]
6. González Ruiz A,
Haque R, Aguirre A, Castañón G, Hall A et al. (1994) Value of microscopy in the
diagnosis of dysentery associated with invasive Entamoeba histolytica. J
Clin Pathol 47: 236-239. [Crossref]
7. Tanyuksel M, Petri
Jr. WA (2003) Laboratory diagnosis of amebiasis. Clin Microbiol Rev 16:
713-729. [Crossref]
8. Salles JM, Salles MJ, Moraes LA, Silva MC (2007) Invasive amebiasis: an update on diagnosis and management. Expert Rev Anti Infect Ther 5: 893-901. [Crossref]
9. Ahmed M (2010) Amoebic-induced ileal stricturing: a case report. Ann R Coll Surg Engl 92: W15-W16. [Crossref]
