Journals
Insect bite-like reaction showing features of panniculitis in a patient with chronic lymphocytic leukemia
A B S T R A C T
The association of insect bite-like reactions with hematological malignancies, especially chronic lymphocytic leukemia (CLL) is well established. Rarely, these eruptions may involve the subcutis, leading to eosinophilic panniculitis. Here, we present a case of CLL accompanied by an insect bite-like reaction with features of panniculitis. Insect bite-like lesions, eosinophilic panniculitis and and Wells’ syndrome should be considered in the same spectrum in patients with hematologic disorders.
Introduction
Skin lesions occur in up to 25% of patients with CLL. These disorders develop as a result of cutaneous infiltration of leukemic cells (leukemia cutis) or as secondary or nonspesific lesions. Secondary lesions include pyoderma gangrenosum, Sweet’s syndrome, purpura, vasculitis, paraneoplastic pemphigus, exfoliative dermatitits, pruritus and insect bite-like reactions [1, 2]. Insect bite-like reactions are characterized by pruritic frequently tender papules, plaques, nodules and in some cases vesicles/bullae in exposed and nonexposed areas of the body with no relationship to seasonal changes [1, 3]. Here, we present a case of insect bite-like reaction with panniculitis-like features in association with CLL.
Case Report
62-year-old female patient who was diagnosed with CLL 13 years ago was admitted to the dermatology department with severely pruritic lesions. The lesions had appeared three months ago. On physical examination, numerous indurated, erythematous, nodular lesions with a central punctum, measuring 2-3 cm were noted on the hands, forearms and lower legs (Figure 1). The patient had received six courses of chemotherapy regimen consisting of rituximab, fludarabine and cyclophosphamide three years ago and she was administered chlorambucil intermittantly. Consequently, remission was achieved.
Figure 1: Erythematous, nodular lesion with a central punctum located to the left hand.
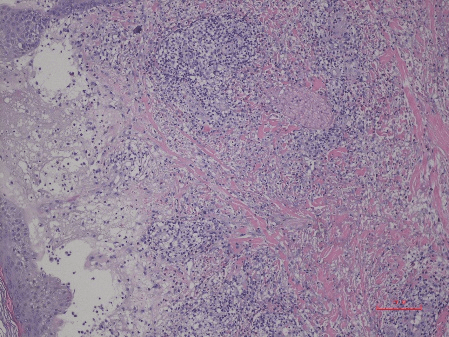
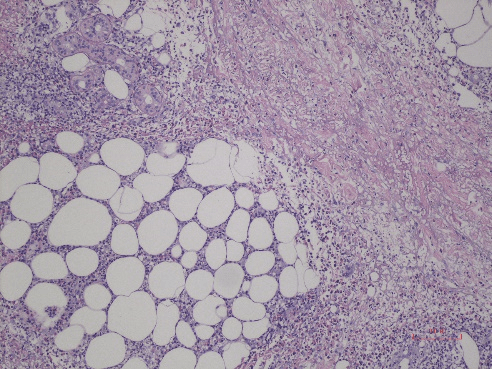
Laboratory examination was as follows: ESR: 84 mm/h, leukocyte: 25.430/mm3 (differential count could not be measured in complete blood count), hb: 9.4 gm/dL, htc: 29.5%. LDH levels, liver and renal function tests were normal. The biopsy revealed spongiosis, microvesicles filled with eosinophils in the epidermis as well as subepidermal splitting (Figure 2a). Perivascular and interstitial lymphocyte and histiocyte infiltration accompanied by eosinophils was present in the dermis. Additionally, dense eosinophilic infiltration located to the septal, paraseptal and lobular regions was noted in the subcutis suggestive of eosinophilic panniculitis (Figure 2b). Immunohistochemical analysis was not performed and direct immunofluorescence test was negative. A diagnosis of insect bite-like reaction was made based on clinical and histopathologic findings. The patient was administered topical corticorticosteroids and systemic antihistamines, but the lesions persisted despite the symptomatic therapy. The lesions were controlled partially by this treatment over the following 12 months, during which new lesions occurred sporadically.
Figure 2a: Spongiosis, microvesicles filled with eosinophils in the epidermis and subepidermal splitting. In the upper dermis there is a perivascular and interstitial lymphocyte and histiocyte infiltration accompanied by eosinophils (HE, 40x).
Figure 2b: Dense eosinophilic infiltration located to the septal, paraseptal and lobular regions (HE, 100x).
Discussions
Weed described an exaggerated hypersensitivity reaction to mosquito bites in eight patients with CLL in 1965 [4]. Consequently, it was observed that this reaction occurred most frequently without any connection to arthropod bites. Although the clinical and histopathological picture is consistent with insect bites, there is no history of insect bites in most of the patients. Besides, the clinical course, distribution of lesions, response to treatment or preventive measures do not indicate an exagerrated reaction to true insect bites. Therefore, new terms were proposed to describe this phenomenon: “insect bite-like reaction” or “eosinophilic eruption of hematoproliferative disease” by Barzilai et al. and “eosinophilic dematosis of myeloproliferative disease” by Byrd et al. [1, 5].
Byrd et al. proposed following criteria for defining the disorder: (1) pruritic papules, nodules and/or vesiculobullous eruption refractory to standard treatment; (2) histopathology revealing eosinophil-rich superficial and deep dermal lymphohistiocytic infiltrate; (3) exclusion of other causes of tissue eosinophilia and (4) diagnosis of hematologic malignancy (5). Our case fulfilled these criteria.
Histopathological examination shows superficial and deep perivascular infiltrate of lymphocytes accompanied by eosinophils. A heavy eosinofilic infiltrate may produce vesicobullous lesions that are seen clinically. Eosinophils may be present in the epidermis causing spongiosis or they may also infiltrate the subcutis leading to panniculitis as in our case [3]. Rodriguez-Lojo et al. reported a case of CLL with eosinophilic panniculitis in a patient with (CLL), in which the morphology of cutaneous eruption changed later to insect bite-like lesions. Flame figures were also noted in this case [6]. It is speculted that, Wells’ syndrome which has been described in patients with malignant hematologic disorders is a variant of insect bite-like reactions [1]. Of the various hematologic malignancies, eosinophilic dermatosis has been most frequently described in association with CLL [3]. Other less frequent associations are mantle zone lymphoma, acute lymphoblastic leukemia, large cell lymphoma, marginal zone lymphoma, as well as myeloproliferative diseases [1, 7, 8]. The differential diagnosis of insect bite-like reactions includes leukemia cutis, scabies, prurigo, drug eruption, insect bite reaction, papular urticaria, urticarial stage of bullous pemphigoid, dermatitis herpetiformis, eosinophilic folliculitis, Wells’ syndrome and leukemic infilrates [3, 5].
The eruption usually occurs concurrent with or months to years after CLL diagnosis, but sometimes insect bite-like reactions disease can precede the diagnosis of CLL [1, 3, 6]. The relationship between the disorder and the prognosis is controversial. According to Barzilai, the eruption was unrelated to disease course and laboratory findings; however, three patients had progression of their disease showing Richter transformation and malinant clone expression in their series [1]. Additionally, Bairey et al. noted that the eruption was not related to disease activity or the course of hematological disease, but relatively high proportion of their patients had poor prognostic feaures such as elevation of β2-microglobulin levels, deletion of 17p or 11q. and CD38 positivity [8].
The pathogenesis of insect bite-like reactions is not fully elucidated. An altered immunologic response due to underlying malignancy, chemotherapy or immunosupression have been suggested [3]. It is possible that that a population of T-helper 2 (Th2) lymphocytes, reactive to malignant B-cells, induces tissue eosinophilia, mainly through production of interleukin IL-4 and IL-5, among other cytokines. Eosinophils appear to be the main effector cells [1, 9]. Recently, FISH analysis revealed neoplastic CLL-cells within the eo¬sinophilic skin infiltrate in a patient [10].
Treatment of insect bite-like reactions is generally difficult. Topical corticosteroids and systemic antihistamines are usually not effective. Other treatment options are phototherapy, systemic corticosteroids, dapsone, intravenous immunoglobulin and even reinitiation of chemotherapy [1, 2, 7, 8]. Systemic corticosteroids (prednisolone ≥ 40 mg) are usually the most effective treatment, but the lesions may flare after the dose is tapered [7, 8]. Our patient was also resistant to topical antipruritics and systemic antihistamines.
In conclusion, insect bite-like reactions should be included in the differential diagnosis of pruritic papulovesicular or nodular lesions in the setting of hematological malignancies. These reactions may rarely have panniculitis-like features. Insect bite-like lesions, eosinophilic panniculitis and and Wells’ syndrome should be considered in the same spectrum in patients with hematologic disorders. Although the relation between the dermatosis and the prognosis of CLL is not clear, patients should be monitored carefully since the condition may herald a more severe CLL course.
Article Info
Article Type
Case ReportPublication history
Received: Tue 01, Jan 2019Accepted: Wed 16, Jan 2019
Published: Thu 28, Mar 2019
Copyright
© 2023 Ralfi Singer. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2019.01.101
Author Info
K?bra K?z?ltac Naciye Demirel Rahime Tanr?tan?r Ralfi Singer Tlin Yksel
Corresponding Author
Ralfi SingerOkmeydanı Training and Research Hospital, Department of Dermatology, Istanbul, Turkey
Figures & Tables

References
1. Barzilai A, Shapiro D, Goldberg I, Yacob-Hirsch Y, Diaz-Cascajo C, et al. (1990) Insect bite-like reaction in patients with hematologic malignant neoplasms. Arch Dermatol 1999 135: 1503-1507. [Crossref]
2. Robak E, Robak T (2007) Skin lesions in chronic lymphocytic leukemia. Leuk lymphoma 48: 855-865. [Crossref]
3. Farber MJ, Forgia SL, Sahu J, Lee JB (2012) Eosinophilic dermatosis of hematologic malignancy. J Cutan Pathol 39: 690-695. [Crossref]
4. Weed RI (1965) Exaggerated delayed hypersensitivity to mosquito bites in chronic lymphocytic leukemia. Blood 26: 257-268. [Crossref]
5. Byrd JA, Scherschun L, Chaffins ML, Fivenson,DP (2001) Eosinophilic dermatosis of myeloproliferative disease: characterization of a unique eruption in patients with hematologic disorders. Arch Dermatol 137: 1378-1380. [Crossref]
6. R Rodríguez-Lojo, M Almagro, F Piñeyro, L Pérez-Varela, B Fernández-Jorge, et al. (2010) Eosinophilic panniculitis and insect bite-like eruption in a patient with chronic lymphocytic leukaemia: a spectrum of the same entity. Dermatol Res Pract 2010: 263827. [Crossref]
7. Dodiuk-Gad RP, Dann EJ, Bergman R (2004) Insect bite like reaction associated with mantle cell lymphoma: a report of two cases and review of the literature. Int J Dermatol 45: 754-758. [Crossref]
8. Bairey O, Goldschmidt N, Ruchlemer R, Tadmor T, Rahimi-Levene N, et al. (2012) Insect-bite-like reaction in patients with chronic lymphocytic leukemia: a study from the Israeli Chronic Lymphocytic Leukemia Study Group. Eur J Haematol 89: 491-496. [Crossref]
9. Chassine AF, Dadban A, Charfi S, Chaby G, Royer B, et al. (2010) Eosinophilic dermatosis associated with haematological disorders: a clinical,histopathological and immunohistochemical study of six observations. Ann Dermatol Venerol 137: 181-188. [Crossref]
10. Mitteldorf C, Tronnier M, Merz H, Haenssle HA, Bertsch HP, et al. (2012) Insect bite-like reactions in a patient with B-cell chronic lymphocytic leukaemia: fluorescence in situ hybridization analysis revealed neoplastic B cells within the skin infiltrate. Br J Dermatol 167: 944-946. [Crossref]
