Journals
Imaging of Acute Appendicitis for Adult Patients
A B S T R A C T
Objectives: To describe the normal and pathological radiological appearance of the appendix in the adult patient using ultrasound (US), computed tomography (CT) and magnetic resonance imaging (MRI). Furthermore, to review the utility of the aforementioned imaging modalities in different clinical contexts.
Summary: The diagnosis of an inflamed appendix based on clinical evaluation, biological data and cross-sectional imaging. US is the first line technique to consider and is the modality of choice for children, young and thin patients and women of childbearing age. An inconclusive ultrasound examination should lead to the realization of a CT. The appearance of the normal and pathological appendix needs to be clarified, in view of the modern technological developments of US as well as on the basis of the new CT methods (multidetector CT, with or without dual energy, low-dose acquisition). CT examinations can be performed with or without intravenous injection of contrast medium, accompanied by oral or rectal opacification, with variable diagnostic performance depending on the thickness of the sections and the possible use of reconstructions. MRI remains the second most important examination for young patients and pregnant women. In view of such technical progress, the plain films of the abdomen no longer have a role in everyday practice.
Conclusion: A better knowledge of the US and cross-sectional appearance (CT-MRI) of the normal or inflamed appendix should allow the radiologist to contribute to an optimal management of this very frequent acute clinical situation. This approach reduces unnecessary radiation and negative appendectomies and optimizes the health care expenditures.
Keywords
Appendix,appendicitis,ultrasonography,computed tomography,MRI
Introduction
From the past until today, acute appendicitis in adult and pediatric patients remains the most common diagnosis in patients admitted for acute abdominal pain [1]. Appendectomy is the most common emergency abdominal surgery [2]. However, the proper diagnosis of this common condition is a permanent problem for any doctor. The rate of negative appendectomy used to be in the range of 20 to 28% before CT imaging and US became routinely used [2]. This negative appendectomy score was reduced by the use of imaging and was shown to be in the order of 7 to 10% when assessing the impact of imaging on this type of diagnostic pathway with a slightly lower score for US (8%) compared to that of CT (7%) [3-5]. Nowadays, the pre-operative diagnosis of acute appendicitis can no longer be based solely on clinical evaluation and biology. Thus, it has been shown that US is earlier and above all more reliable than biological tests in case of suspicion of acute appendicitis with reliability of 97% for US (based on the abnormal diameter of the appendix), and 66% based on an increase in the white blood cell count and / or CRP [6]. Additionally, US helps to identify alternative diagnoses leading to another medical or surgical management. These reasons support the important role of US and CT, which have reduced the rate of perforated appendicitis by up to 13%, and ameliorated the number of severe forms of appendicitis, despite the existence of publications questioning the role of sectional imaging [7-10]. The number of diagnostic errors is also steadily decreasing, especially in-patient populations whose clinical evaluation is more difficult, especially the pregnant woman and the elderly patient [11-13]. In addition, it is important to reduce unnecessary abdominal surgery, because any abdominal operation is associated with a high risk of adhesions and occlusion, with severe and repeated consequences for the patient and with decreased fertility for women [14]. The sensitivity, specificity and reliability values of clinical evaluation, US and CT are summarized in (Table 1). The purpose of this review is to analyze and illustrate the state of current knowledge regarding the role of imaging to highlight evidence of appendicitis and to recognize the severity of the condition.
Table 1:
|
|
Clinic (%) |
US (%) |
CT (%) |
MRI |
|
sensitivity |
85,93 |
30,76,83,95,98 |
88,92,97,100 |
95-97% |
|
specificity |
74,81 |
75,90,94,100 |
85,91,95,100 |
95-97% |
|
accuracy |
77,85 |
69,94,97 |
88,90,98 |
Based on Duke (2016), Horton (2001), Kessler (2004), Morris (2002), Park (2014), Rao (1997), Rioux (1992), and Storman (1999).
Current available modalities
I Plain films of the abdomen
In 1989, in clinically doubtful cases of appendicitis, the abdominal plain films were considering to bring decision-making elements: the highlighting of an appendicolith, which can be seen in 14% of patients and the median translation of the cecum with increase of the thickness of the para-colic gutter of more than 10 mm [15]. It is currently agreed that plain radiographs are so low in sensitivity that there are ineffective in this context [2, 16, 17].
II Ultrasound (US)
Key points
US technique offers performance that depends on the severity of appendicitis. In uncomplicated form, the US sensitivity is 75-90%, the specificity 86-100% and the positive predictive value 89-93% with an overall reliability of 89-93% [2]. In complicated cases, sensitivity drops to 28% largely because of the surrounding gases that mask the inflamed appendix and because of the abdominal defense [18]. The main limitation of US is related to cases where the appendix has not been seen [2]. The non-visualization of part or all of the appendix prevents the exclusion of the condition [19]. The US performance in pregnant women is optimal - except in late pregnancy - with a sensitivity of 100%, a specificity of 96% and a reliability of 98% [20].
Exam technique
US examination for suspicion of appendicitis should always begin with an overall evaluation of the abdomen using low frequency probes to exclude abnormal liver, gallbladder, pelvis, kidneys, aortic size and the portomesenteric vessels patency [21]. Abscesses or fluid effusions are detected during this abdominal sweep. Bladder repletion is not necessary to allow optimal examination of appendix (Figure 1) [22]. Some authors have shown improved visualization of the appendix using saling colonic enema: this option is however not applicable and commonly used in clinical routine [23].
The search for the appendix and the analysis of the ileocecal junction are then carried out with linear probes, of higher frequency, using the method of the gentle compression developed by Puylaert [18, 22]. This consists of a soft and progressive compression of the abdominal wall in the direction of the painful site, beginning the maneuver opposite the iliac bifurcation, to the point of maximum pain [22, 24]. More recently, an additional posterior compression maneuver has been reported, increasing the visibility score of the appendix [25]. The US diagnosis of appendicitis is improved if the patient is asked to pinpoint the painful location [26]. Conversely, drug sedation decreases the performance of US [27].
Figure 1: US findings of an acute appendicitis depicted with low and high frequency probes : (A) With the low frequency probe, there is a infiltration of the peridigestive fat (asterisk), and a thickening of a digestive segment (arrowheads) closed to the right iliac vessels (B) With the high frequency probe, this digestive structure corresponds to the inflamed appendix (arrow), distinct from the ileum (arrowheads) located in front of it.
Figure 2: Drawing of the ileo-caecal and the appendiceal junction.
Ultrasound features of the normal appendix
The point is to identify the ileocecal valve, with its pseudo-tumoral aspect, and to prevent confusion of the ileum with the appendix (Figure 2, 3) [28]. The appendix connects gently with the cecum. It appears as a digestive structure with a blind tip, with an external transverse diameter of less than 6 mm. Its length is variable, oscillating from 2 to 25 cm [29]. The normal appendiceal wall is less than 3 mm [29]. The locations of the appendix are variable, retrocecal, retro-longitudinal, pre-pelvic and pelvic [24, 26, 29]. The normal appendix is compressible, without peristaltic wave. The appendiceal lumen contains hyperechoic material (air or residues) [31]. The content becomes hypoechoic, even anechoic, when the appendix is full of liquid [18, 32, 33]. US examination is considered as normal when the entire appendix has been viewed [19]. The parietal flow of the normal intestine can be detected by Doppler US, using low velocity scales, identical to those used during venous system examinations. In the normal appendix, it is almost impossible to obtain a color Doppler signal [34-36].
Figure 3: (A) longitudinal view of the ileum (arrowheads) which is oriented toward the caecum; the caecum is seen in cross-section (asterisk). (B) Longituinal view of the appendix (arrowheads) which is in the continuity of the caecal wall (asterisk).
Figure 4: US centered on the right paracolic gutter showing typical appendicitis appearance: (A) Cross-sectional view of the inflamed and enlarged appendix: its transverse, diameter is 10 mm under compression; there is an infiltration of the periappendiceal fat (asterisk). (B) Longitudinal view of the inflamed appendix, which has a latero-caecal position.
Ultrasound appearance of acute appendicitis
The US diagnosis of appendicitis is based on the visualization of an intestinal structure with a blind tip having a maximum diameter of at least 6 mm under probe compression and in connection with the cecum (Figure 4) [18, 24, 37-39]. Some studies report that physicians rely on the thickness of the wall which must be 3 mm or more, a smaller thickness being accepted if the appendix is distended upstream of an appendicolith or when the fluid filling the appendiceal lumen cannot be hunted towards the cecum [40]. Appendicolith is sometimes seen as a hyperechoic structure in the appendiceal lumen. A parietal hyperemia is visible in color Doppler mode, which allows to specify inflammation of the appendix when its transverse diameter is at the limit of the norm (Figure 5) [35, 36, 41, 42]. The changes in the appendicular environment detected with US are the infiltration of the adjacent fat, a small amount of fluid, enlarged mesenteric lymph nodes and collections adjacent to the inflamed appendix. Localized perforation may be evoked when the hyperechoic layer of the appendicular wall (the submucosa) has focally disappeared or when a collection is seen in close contact with the inflamed appendix [24, 41, 43]. Usually this localized perforation is better assessed with CT (Figure 6). The absence of color Doppler flow in an inflamed appendix is a sign of necrosis [34-36].
Figure 5: Hyperhemia of the inflammatory appendix demonstrated with color Doppler mode.
Figure 6: US and CT scan in the same patient: the initial US was followed by a CT because of the severe pain suggestive of pneumoperitoneum or abscess not identified or excluded with US. (A) Acute appendicitis (arrowheads), well detected with US, where the periappendiceal fat infiltration is clearly seen. (B) On the CT, detection of periappendiceal gas (arrow) in relation to localized perforation of this inflamed appendix, not initially detected with US.
Some publications have supported improved diagnostic performance through the use of harmonic or other specific modalities from one manufacturer to another. In our personal experience, the quality and fineness of the image significantly improves the confidence of the operator. The harmonic, used with the low frequency probes, proved sometimes useful to better delimit the environment of the inflamed appendix and recognize signs of localized perforation.
How to proceed with an ambiguous US result?
Different attitudes are possible, based on the degree of clinical suspicion. If it is high, the discussion will focus on performing a CT scan in the process, or monitoring the patient. Some studies propose to release the patient and conduct clinical follow-up by seeing them within 24 hours if less than two of the following criteria are met: male sex, right iliac fossa pain migration, vomiting, leucocyte count > 12.0 x 109/ l [44].
III Tomodensitometry (CT)
Key points
A lot of publications have highlighted the predominant role of CT in the assessment of acute appendicitis. Some works have focused on the comparison between US and CT, demonstrating the superiority of CT, largely due to the independence of this technique from the operator's experience, relative to the type of patient and the presence of gaseous interfaces [45-49]. Two clinical situations are usually evoked: classic clinical presentation in a patient with acute and low abdominal pain and atypical clinical situations. In the first case, the CT results are as follows: a sensitivity of 97%, a specificity of 98% and a reliability of 98% [46]. In the second case (uncertain clinical situations), the results have a sensitivity of 92%, a specificity of 85% and an overall reliability of 90% [51].
Exam technique
Among the many articles on the subject, two attitudes are promoted: the focused examination of the right iliac fossa and the overall abdominal examination, from the liver dome to the pubis. The focused technique has the merit of reducing the field of exploration but it imposes manipulations and complementary acquisitions when the appendix has not been detected on the initial series [52, 53]. The global examination includes all the possible appendiceal localizations and leads to alternative diagnoses whose percentage can exceed more than 60% [50, 54]. The spiral CT is commonly made using reconstructed 3 mm thick sections, from the hepatic dome to the ischia. The other parameters used vary from one study to another: the mAs oscillate between 100, 200, 220, 240, 320 and kVp from 120 to 140 [50, 54]. A low dose CT approach (with 100 to 120 KvP and 25 to 30 mAs) has been demonstrated as accurate as the standard dose CT for the diagnosis of acute appendicitis [55, 56]. A recent metaanalysis has confirmed this scenario [57]. The utility of multiplanar reconstructions has been validated [58]. In our practice, we use it only exceptionally and mostly in complex cases.
Trends vary with regard to opacification, from the upper tract or colonic enema, and intravenous injection of contrast medium. In the UK and the USA, oral ingestion is used in more than 90% of cases, but much more rarely rectal opacification [50]. A total amount of 800 to 1000 ml of meglumine diatrizoate or meglumine ioxitalamate diluted from 2 to 5% has to be ingested at least 45 minutes before the CT examination [50, 52, 54]. Rectal opacification is performed with a quantity of 40 ml of meglumine diluted in one liter of water; if the cecum is not filled with contrast on the scout-view, it is recommended to complete the enema with 250 ml of saline water [53]. However, the recent trend is to dispense with this rectal opacification despite the fact that it allows a better delimitation of the appendix and inflammatory changes of neighborhood. The overall reliability of the CT technique is significantly improved by intravenous injection of contrast medium [2, 54]. 100 to 150 ml of contrast medium are injected intravenously at a concentration of 60% with an automatic injector at a rate of 2 to 4 ml / sec (more commonly at 3 ml / sec), the examination starting with a delay 70 seconds. In our institution, 120 ml are injected with a delay of 70 sec, with a flow rate of 2.5 ml / sec [54]. The reader performance has been demonstrated as the most reliable factor for the diagnostic correctness of CT in case of acute appendicitis, when oral or intravenous contrast (isolated or combined), radiation dose [59]. The patient sex has also an impact in this setting.
CT appearance of the normal appendix
The appendix has a normal appearance in CT when it is completely filled with opacifying material, air or both, and its wall is less than 2mm, whatever the maximum transverse diameter. A normal unfilled appendix can have a transverse diameter from 4.2 to 12.8 mm if the adjacent fatty tissue is not modified or if there is no nearby inflammation and the enhancement of the appendicular walls is similar to that of the normal intestine [53, 60-64].
Figure 7: Three CT illustrations of typical acute appendicitis: (A) Appendicitis in front of the psoas muscle (arrow): the appendix is slightly enlarged and its wall is hyper-attenuated. (B) Swollen appendix containing several appendicoltihes (arrowhead); the periappendiceal fat is infiltrated. (C) Thickened appendix containing an appendicolith at its center (arrowhead); the surrounding fat is finely infiltrated.
CT appearance of true appendicitis
Acute Appendicitis is diagnosed at two stages: the early form (frequent) and the advanced form (complicated, unusual) [8, 63]. We require two criteria in order to make the diagnosis of a simple and acute appendicitis: the visualization of a swollen appendix, with the diameter greater than 6mm, with or without an enhancement of the wall and accompanied by an infiltration of peri-appendicular fat or the identification of an appendicolith associated with an infiltration of the pericaecal fat (Figure 7) [60-65]. Secondary and non-specific anomalies of appendicitis are the presence of an appendicolith, the absence of contrast medium in the appendiceal lumen, extra-digestive gas, a fluid collection or lymph nodes, a localized thickening of the caecal walls [52-54, 60-62] (Figure 8). The thickening of the wall of the cecum can take on a very localized appearance, resulting in an arrow-like structure of the cecal contrast, opposite the entrance of the inflamed appendix ("cecal arrowhead sign") [62]. This sign, related to appendicitis, is associated with a high specificity 100% and a sensitivity of 30%.
Figure 8: Appendicitis not seen in US and clearly identified at CT. (A) US focused on the right iliac fossa: infiltration of pelvic fat and gazeous structures with a linear arrangement (arrows). (B) and (C) CT shows an enlarged and inflamed appendix (arrowhead), appendicolitis (arrow) and infiltration of periappendiceal fat.
Advanced or complicated appendicitis is more difficult to diagnose due to changes in the environment of the right iliac fossa [62]. The appendix becomes unrecognizable, but the CT allows to visualize a segment of residual appendix included in the peri-caecal inflammatory magma. Due to the delay in diagnosis, one or more peri-appendicular collections are visible; the surrounding fat is infiltrated and the adjacent organs are inflamed (small bowel, gynecological organs or sigmoid colon).
Figure 9: CT required for clinical suspicion of a small bowel obstruction in an elderly patient. On the CT, significant inflammatory swelling of the appendix (arrowheads) with infiltration of neighboring fat. There are some distented small loops in the left hemiabdomen due to an adynamic reflex ileus.
Sometimes, the clinical presentation of acute appendicitis may mimic the clinical and radiological picture of mechanical small bowel obstruction, more readily observed in the elderly patient (Figure 9) [13]. The purulent material occasionally points to the mesenteric venous network and causes pylephlebitis, complicated by hepatic abscesses (Figure 10) [65]. Extra-digestive air is also visible in contact with the inflammatory ileocecal junction, related to a localized and covered perforation (Figure 11). In more severe form, a diffuse pneumoperitoneum is detected: CT is the best imaging method for detection of this crucial and severe complication [66].
Figure 10: Complicated appendicitis with mesenteric vein thrombophleblitis. (A) Inflammatory involvement of the appendix (arrowhead): the appendix is hypervascularized and the adjacent fat is infiltrated. (B) Frontal view of the mesenteric venous network: expansive thrombosis of the ileocecal branch of the superior mesenteric vein (arrowheads) and infiltration of adjacent fat.
Figure 11: Perforated appendicitis not seen on US and detected with CT. (A) Ultrasonography of the right iliac fossa, showing a gazeous structure (arrowhead) fixed within the infiltrated pelvic fat. (B) and (C) The CT scan helps to conclude to a perforated acute appendicitis: the appendix is enlarged (arrow), there is ascitis and extra-digestive gas (arrowhead).
How to proceed with an ambiguous CT result?
The reliability of the CT for appendicitis assessment is high: sensitivity 90-100%, specificity 91-99% [68]. Equivocal CT is debated in the literature. The equivocal scan cases range from 5 to 13% and in these cases, the surgical conclusion of appendicitis was finally noted in 13 to 73% of cases [68]. In this series of 1344 patients admitted for suspicion of appendicitis, 22% had a CT read as positive, confirmed surgically in 88%, 13% equivocal and confirmed as appendicitis in 30% and 64% as CT negative and with proven appendicitis in 0.2% [69]. In this study, the threshold value of the appendicular diameter was 9 mm. This study recommends that an equivocal CTs helps to recognize an appendicitis with a probability of surgical confirmation in 30% when the appendicular diameter equals or exceeds 9 mm. In another publication on the equivocal CTs of appendicitis, it is noted that the following signs point to the diagnosis of appendicitis at CT: enhancement of the appendicular wall, absence of gas in the lumen of the appendix, co-existence of a neighboring inflammatory lesion, thickening of the walls of the appendix (3,54 mm ± 0,5) [1-4 ,66].
Figure 12: CT frontal reformation illustrating the fluid distension of the appendix related to a non-complicated appendiceal mucocele.
Figure 13: CT findings of an appendiceal mucinous cystadenoma with high grade dysplasia causing the appendiceal mucocele : the appendix is distended and its wall is partially calcified. The surrounding fatty tissue is infiltrated.
IV The mucocele of the appendix: a rare condition not to be ignored
The appendiceal mucocele is a cystic dilatation of the appendix, which is filled with mucus (Figure 12). When this distended appendage breaks, it causes the peritoneal pseudomyxoma. This mucocele can be detected outside or during acute abdominal pain, such as suspicion of acute appendicitis. It is therefore important for the radiologist to mention such a diagnosis, whether with US or CT (Figure 13) [70]. Mucocoele appears as a blind cystic mass in the right iliac fossa. On US, its intraluminal echostructure is heterogeneous, mainly hypoechoic, with posterior acoustic reinforcement; the appearance of the contents is depending on the presence of necrosis, cell debris and the mucus consistency. The content can be stratified as an onion bulb and includes septas. In less than 50% of cases there are fine parietal, arciform or punctiform, hyperechoic calcifications. On CT, the mucocele appears as a well-encapsulated thin-walled cystic mass, the presence of parietal calcification may suggest the diagnosis, but this sign is only found in less than 50% of cases (Figure 14).
Figure 14: CT findings of a low-grade appendiceal mucosal lesion infiltrating the appendiceal wall and inflammatory adhesions closed to the terminal ileum (arrows). Thin calcification is noted in the appendiceal fundus (arrowhead).
The consequences of irradiation
Many studies have highlighted the high value of CT in case of appendicitis. However, it is necessary to discuss about the consequences of the irradiation. Indeed, CT is responsible for 40 to 70% of irradiations in radiology, while it represents between 4 and 7% of the volume of acts performed in radiology [9, 71]. The dose delivered per examination is estimated to be between 8 to 20 mSv, with a current average of 10 mSv. Nevertheless, the practice of CT to rule out or confirm acute appendicitis makes it possible to avoid unnecessary expenditure and to reduce the number of unnecessary surgical procedures, with a reduction in short and long-term morbidity, in particular post-adhesive occlusions [71, 72].
Most radiation-sensitive patients receive first-line US according to international recommendations. If the patient is young and there is a trained operator, it is best to begin the assessment with US and then continue with a CT scan in case of doubt [68]. Many papers currently praise low-dose CT, reducing radiation doses by four fold (2 mSv vs 8mSv) with the same sensitivity and specificity as the standard CT and should be favored in these young patients [55-59, 74]. In the context of pregnancy, before the advent of MRI in most major centers, some authors went so far as to propose CT when US was ineffective, provided that a targeted examination was performed. with a reduction of millimamps and using a high pitch [11, 75]. According to these studies, no more than 300 mrad are deliverated, which would be in the same order as that of a conventional pelvimetry (250 mrad); this dose is more than double the dose given to the fetal gonads during CT pelvimetry [76]. CT performed in pregnant women would reduce the current rate of 40% of the negative laparotomies. Until now, this high percentage was admitted and tolerated because of the high risk of complications in case of delayed diagnosis of appendicular perforation: the perforation rate is associated with a four-fold risk of fetal mortality [11]. In addition, an adequate preoperative diagnosis would reduce the size of the incision when surgical exploration is required.
In our practice and in agreement with the recommendations of the literature, the approach of a suspicion of appendicitis in the pregnant woman is based first on US, whose reliability is 50 to 77% in the specific context of pregnancy [77]. If US is inconclusive, MRI is the best modality to conduct. The technical difficulty in US is to identify the appendix, which moves from its usual location until the 3rd month of pregnancy to position itself at the lower part of the right hypochondrium at the 8th month [78]. Its identification is made even more complex when it moves behind the uterus. MRI is thus very efficient in the cases not solved with US and removes the option to perform a CT [77, 78]. The series include T2 sequences (with and without fat saturation) and optionally a T1 sequence without gadolinium injection. The basis of the diagnosis is identical to the CT scan, with appendicitis corresponding to dilatation of the appendix - blind tubular structure at the start of the cecum, filled with fluid (hypersignal on T2 weighted series) with an inflammatory environment at its periphery (hypersignal T2) (figure 15).
In our practice and in agreement with the recommendations of the literature, the approach of a suspicion of appendicitis in the pregnant woman is based first on US, whose reliability is 50 to 77% in the specific context of pregnancy [77]. If US is inconclusive, MRI is the best modality to conduct. The technical difficulty in US is to identify the appendix, which moves from its usual location until the 3rd month of pregnancy to position itself at the lower part of the right hypochondrium at the 8th month [78]. Its identification is made even more complex when it moves behind the uterus. MRI is thus very efficient in the cases not solved with US and removes the option to perform a CT [77, 78]. The series include T2 sequences (with and without fat saturation) and optionally a T1 sequence without gadolinium injection. The basis of the diagnosis is identical to the CT scan, with appendicitis corresponding to dilatation of the appendix - blind tubular structure at the start of the cecum, filled with fluid (hypersignal on T2 weighted series) with an inflammatory environment at its periphery (hypersignal T2) (figure 15).
Figure 15: Abdominal MRI showing acute appendicitis, confirmed on histology, this MRI having been performed following an inconclusive US scan: (A) Axial T2-weighted sequence: the appendix (arrowhead) is enlarged and filled with fluid and the surrounding fat is discreetly infiltrated. (B) Axial T2 weighted sequence with fat saturation: fine fluid effusion around the enlarged appendix (arrowheads).
Contribution of imaging to the patient's outcome
In a prospective study showing that the reliability of the CT scan was of 98%, a change of strategy was noted in 59% of the cases [72]. The changes in attitude were as follows: the cancellation of a useless appendectomy, the cancellation of an unnecessary observation on the basis of a normal CT, a surgery decided on the basis of CT, identification of another diagnosis. The authors focused on cost reduction, taking into account the value of a needless appendectomy, a day of hospitalization for observation and the cost of a CT scan: a total of US $ 447 was saved per patient. More recently, it has been shown that reducing the number of misdiagnoses from 25 to 6% still requires a 32 to 84% increase in the rate of CT examinations [12].
In the specific case of the woman admitted for acute pain of the right iliac fossa, the rate of negative appendectomy falls from 50 to 17% when CT is considered as the method of choice [47]. Another study compared CT and US performance: the rate of negative appendectomy decreases from 28 to 7% related to CT and from 28 to 8% thanks to US [76]. The authors concluded that CT is preferable, even though both techniques are equally effective in reducing the number of negative appendectomies in older women or girls [79, 80]. CT reduces the number of perforated appendicitis in the elderly, which is most often not known at the time of emergency admission [13].
In our daily practice based on the European reference publications, the first radiological approach is based on US, because of its results and its safety [73, 78]. This approach involves being integrated with the clinical approach: the combination of the scoring system (Alvarado) with first choice US has been shown to be highly specific and sensitive and significantly reduces the costs for the patient and for public health [6, 81]. CT is performed only in ambiguous cases, in case of US doubt or discordance between the clinic and imaging, especially in the obese patient [82]. However, in women, if there is a possibility of pregnancy, MRI is recommended after an inconclusive US [83]. This approach based on the use of imaging is in agreement with recent publications, showing more than 15% of unexpected diagnoses during the assessment of a suspicion of clinical appendicitis, which can be detected through imaging [84].
Conclusion
This overview illustrates the benefits of current imaging methods for the assessment of acute appendicitis, which is still one of the most frequent abdominal emergencies. It confirms the key role of the radiologist in this case. A modern radiologist has to contribute to the diagnostic process with principles of a rational use of irradiation: begin its assessment with US, followed with a CT or an MRI when US is in doubt.
Conflicts of interest
The authors declare that they have no conflict of interest.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 01, Jul 2019Accepted: Fri 26, Jul 2019
Published: Thu 08, Aug 2019
Copyright
© 2023 Etienne Danse. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2019.03.08
Author Info
C.A. Dragean V. Passoglou Etienne Danse L. Annet P. Trefois S. Van Nieuwenhove
Corresponding Author
Etienne DanseDepartment of Imaging, St Luc University Hospital, Université Catholique de Louvain, 1200 Brussels, Belgium
Figures & Tables
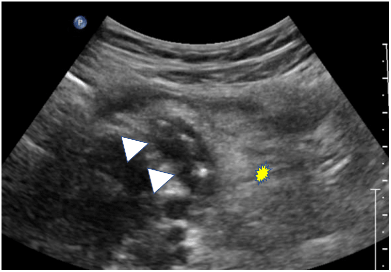
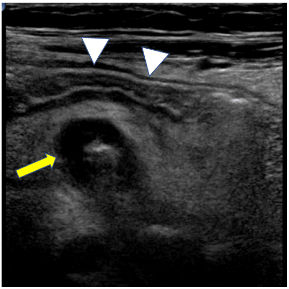
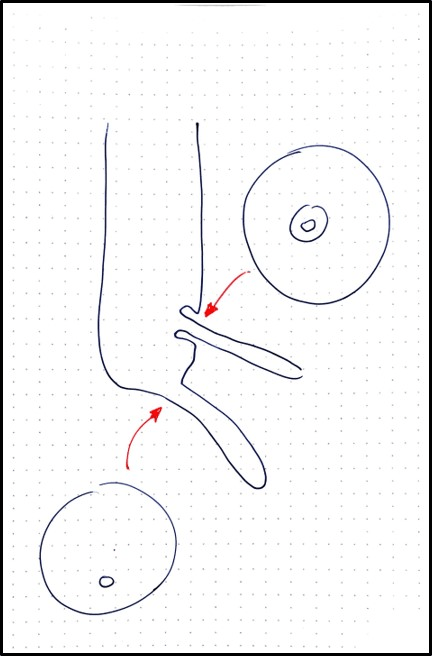
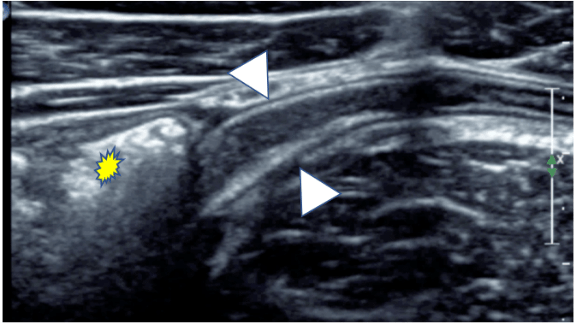
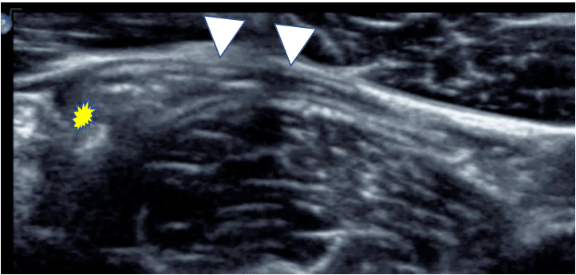
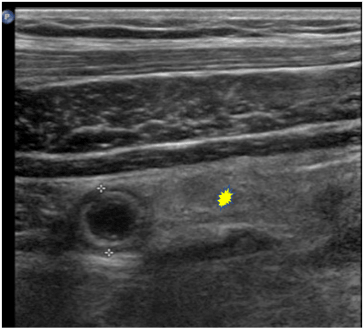
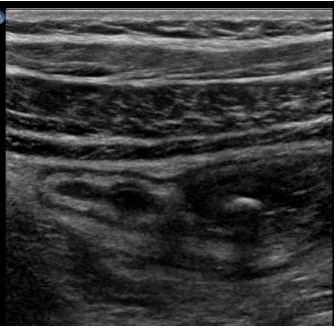
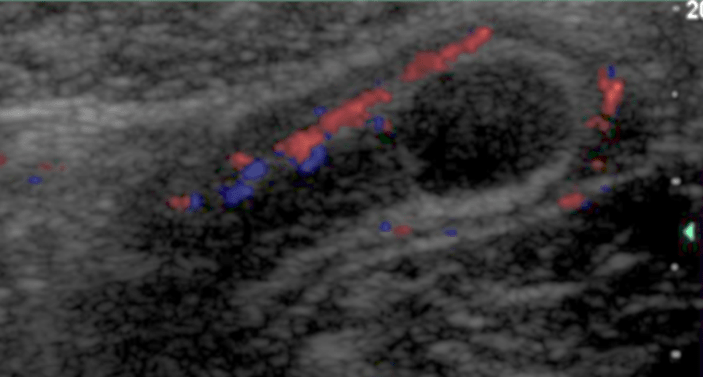
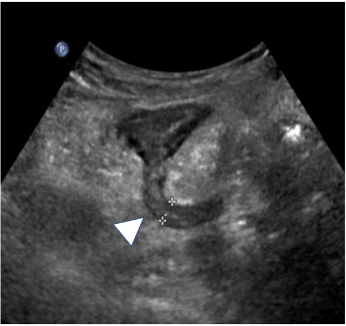
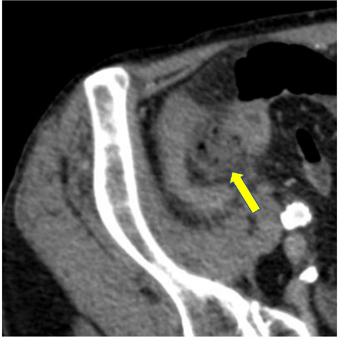
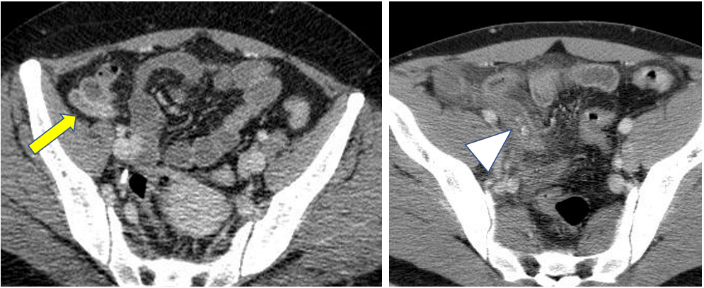
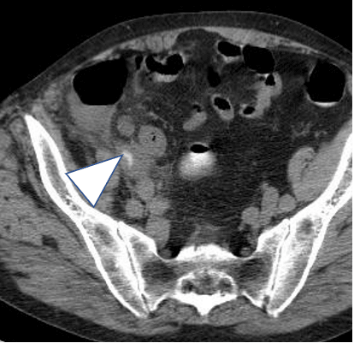
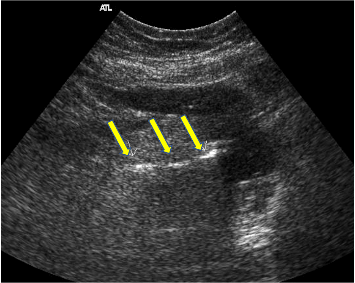
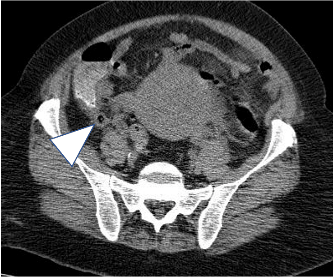
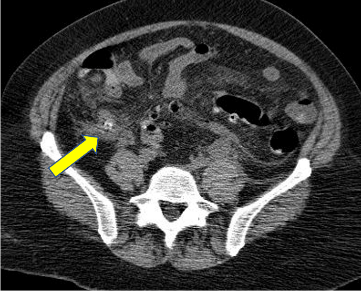
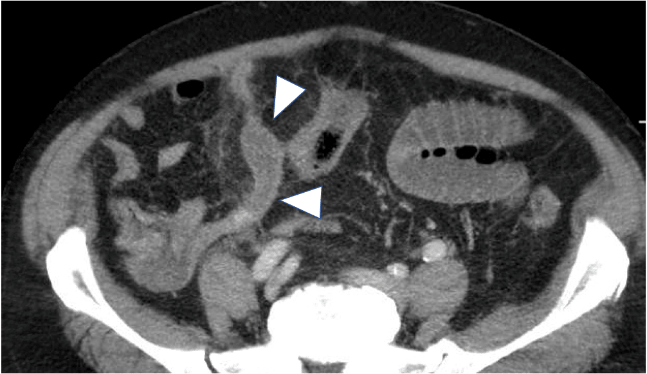
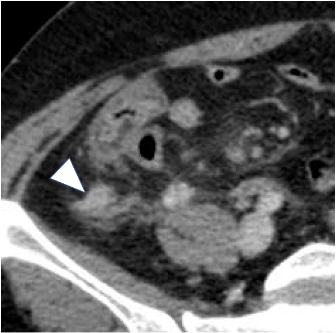
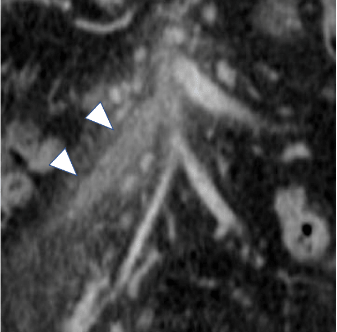

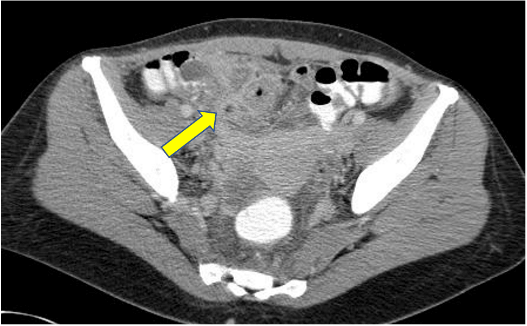
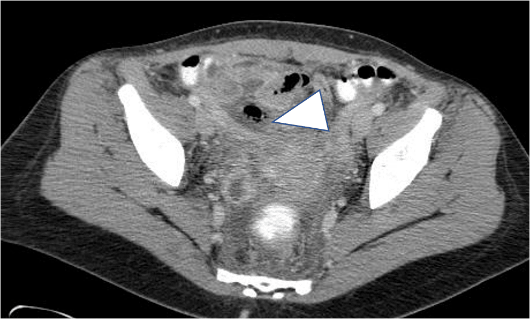

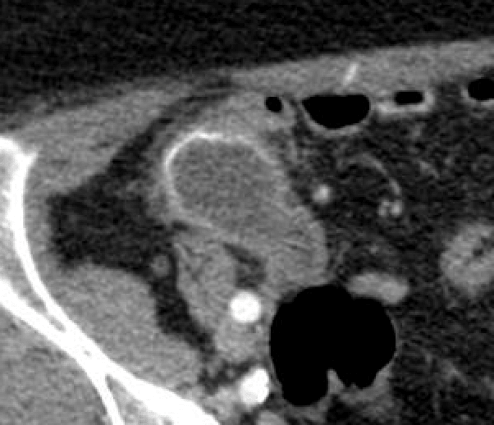
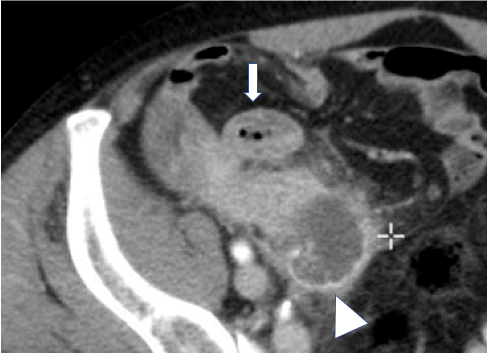
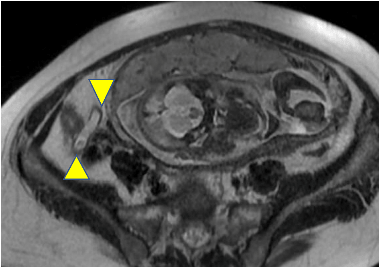
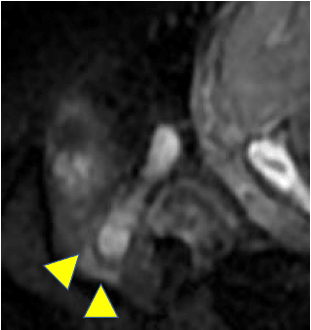
Table 1:
|
|
Clinic (%) |
US (%) |
CT (%) |
MRI |
|
sensitivity |
85,93 |
30,76,83,95,98 |
88,92,97,100 |
95-97% |
|
specificity |
74,81 |
75,90,94,100 |
85,91,95,100 |
95-97% |
|
accuracy |
77,85 |
69,94,97 |
88,90,98 |
Based on Duke (2016), Horton (2001), Kessler (2004), Morris (2002), Park (2014), Rao (1997), Rioux (1992), and Storman (1999).
References
- Clavel C (1955) Stratégie et tactique en chirurgie abdominale d’urgence. Masson, Paris.
- Paulson EK, Kalady MF, Pappas TN (2003) Suspected appendicitis. N Engl J Med 348 :236-242. [Crossref]
- Rao PM, Rhea JT, Rattner DW, Venus LG, Novelline RA (1999) Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg 229: 344-349. [Crossref]
- Bendeck SE, Nino-Murcia M, Berry GJ, Jeffrey RB Jr (2002) Imaging for suspected appendicitis: negative appendectomy and perforation rates. Radiology 225: 131-136. [Crossref]
- Krajewski S, Brown J, Phang PT, Raval M, Brown CJ (2011) Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg 54: 43-53. [Crossref]
- Kessler N, Cyteval C, Gallix B, Lesnik A, Blayac PM et al. (2004) Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology 230: 472-478. [Crossref]
- Neumayer L, Wako E, Fergestaad J, Dayton M (2002) Impact of journal articles and grand rounds on practice: CT scanning in appendicitis. J Gastrointest Surg 6: 338-341. [Crossref]
- Raptopoulos V, Katsou G, Rosen MP, Siewert B, Goldberg SN et al. (2003) Acute appendicitis: effect of increased use of CT on selecting patients earlier. Radiology 226: 521-526. [Crossref]
- Jones PF (2001) Suspected acute appendicitis: trends in management over 30 years. Br J Surg 88: 1570-1577. [Crossref]
- Morris KT, Kavanagh M, Hansen P, Whiteford MH, Deveney K et al. (2002) The rational use of computed tomography scans in the diagnosis of appendicitis. Am J Surg 183: 547-550. [Crossref]
- Ames Castro M, Shipp TD, Castro EE, Ouzounian J, Rao P (2001) The use of helical CT in pregnancy for the diagnosis of acute appendicitis. Am J Obstet Gynecol 184: 954-957. [Crossref]
- Naoum JJ, Mileski WJ, Daller JA, Gomez GA, Gore DC et all. (2002) The use of abdominal computed tomography scan decreases the frequency of misdiagnosis in cases of suspected appendicitis. Am J Surg 184: 587-589. [Crossref]
- Storm-Dickerson TL, Horattas MC (2003) What have we learned over the past 20 years about appendicitis in the elderly? Am J Surg 185: 198-201. [Crossref]
- ten Broek RP, Issa Y, van Santbrink EJ, Bouvy ND, Kruitwagen RF et al. (2013) Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ 347: f5588. [Crossref]
- Mindelzun RE, MCCort JJ (1989) Acute abdomen. In Alimentary tract radiology, 4th edition. Margulis AR and Burhenne HJ. Mosby. St-Louis Missouri.
- Ahn SH, Mayo-Smith WW, Murphy BL, Reinert SE, Cronan JJ (2002) Acute nontraumatic abdominal pain in adult patients: abdominal radiography compared with CT evaluation. Radiology 225: 159-164. [Crossref]
- Rao PM, Rhea JT, Rao JA, Conn Akt (1999) Plain abdominal radiography in clinically suspected appendicitis: diagnosis yield, resource use, and comparison with CT. Am J Emerg Med 17: 325-328. [Crossref]
- Puylaert JB, Rutgers PH, Lalisang RI, de Vries BC, van der Werf SD et al. (1987) A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med 317: 666-669. [Crossref]
- Kearl YL, Claudius I, Behar S, Cooper J, Dollbaum R et al. (2016) Accuracy of Magnetic Resonance Imaging and Ultrasound for Appendicitis in Diagnostic and Nondiagnostic Studies. Acad Emerg Med 23: 179-185. [Crossref]
- Lim HK, Bae SH, Seo GS (1992) Diagnosis of acute appendicitis in pregnant women: value of sonography. AJR Am J Roentgenol 159: 539-542. [Crossref]
- Rioux M (1995) Echographie digestive. L’échographie de l’appendice, normal ou anormal, et ses pièges. Feuillets de radiologie 35: 87-107.
- Puylaert JB (1990) Ultrasound of appendicitis and its differential diagnosis. Springer-Verlag Berlin Heidelberg.
- Han TI (2002) Improved sonographic visualisation of the appendix with a saline enema in children with suspected appendicitis. J Ultrasound in Med 21: 511-516. [Crossref]
- Birnbaum BA, Wilson SR (2000) Appendicitis at the Millenium. Radiology 215: 337-348. [Crossref]
- Lee JH, Jeong YK, Hwang JC, Ham SY, Yang SO (2002) Graded compression sonography with adjuvant use of a posterior manual compression technique in the sonographic diagnosis of acute appendicitis. AJR Am J Roentgenol 178: 863-868. [Crossref]
- Chesbrough RM, Burkhard TK, Balsara ZN, Goff WB, Davis DJ (1993) Self-localization in US of appendicitis: an addition to graded compression. Radiology 187: 349-351. [Crossref]
- Vermeulen B, Morabia A, Unger PF, Goehring C, Grangier C et al. (1999) Acute appendicitis: influence of early pain relief on the accuracy of clincial and US findings in the decision to operate--a randomized trial. Radiology 210: 639-643. [Crossref]
- Rioux M (1994) Echographie digestive : aspects échographiques des iléo-colites. Feuillets de Radiologie 34: 267-283.
- Williams RA, Myers P (1994) Pathology of the appendix and its surgical treatment. Chapman and Hall Medical.
- Simonosvsky V. Normal appendix: is there any significant difference in the maximal mural thickness at US between pediatric and adult population? Radiology 224: 333-337. [Crossref]
- Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Frass R, et al. (2000) Presence of gas in the appendix: additional criteria to rule out or confirm acute appendicitis-evaluation with US. Radiology 214: 183-187. [Crossref]
- Puylaert JB (2001) Ultrasound of acute GI tract conditions. Eur Radiol 10: 1867-1877. [Crossref]
- Wilson SR (1996) Gastrointestinal tract sonography. Abdom Imaging 21: 1-8.
- Jeffrey RB Jr, SommerG, Debatin JF (1994) Color Doppler sonography of focal gastrointestinal lesions: initial clinical experience. J Ultrasound Med 13: 473-478. [Crossref]
- Quillin SP, Siegel MJ (1994) Appendicitis: efficacity of color Doppler sonography. Radiology 191: 557-560. [Crossref]
- Lim HK, Lee WJ, Kim TH, Namgung S, Lee SJ et al. (1996) Appendicitis: usefulness of color Doppler US. Radiology 201: 221-225. [Crossref]
- Puylaert JB (1986) Acute appendicitis: US evaluation using graded compression. Radiology 158: 355-360. [Crossref]
- Rioux M (1992) Sonographic detection of the normal and abnormal appendix. AJR Am J Roentgenol 158: 773-778. [Crossref]
- Vignault F, Filiatraut D, Brandt ML, Garel L, Grignon A et al. (1990) Acute appendicitis in children: evaluation with US. Radiology 176: 501-504. [Crossref]
- Simonovsky V (1999) Sonographic detection of normal and abnormal appendix. Clin Radiol 54: 533-539. [Crossref]
- Guttierez CJ, Mariano MC, Faddis DM, Sullivan RR, Wong RS et al. (1999) Doppler ultrasound accurately screens patients with appendicitis. Am Surg 65: 1015-1017. [Crossref]
- Lim HK, Lee WJ, Lee SJ, Namgung S, Lim JH (1996) Focal appendicitis confined to the tip: diagnosis at US. Radiology 200: 799-801. [Crossref]
- Quillin SP, Siegel MJ, Coffin CM (1992) Acute appendicitis in children: value of sonography in detecting perforation. AJR Am J Roentgenol 159: 1265-1268. [Crossref]
- Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert D et al. (2016) How to diagnose acute appendicitis: ultrasound first. Insights Imaging 7: 255-263. [Crossref]
- Horton MD, Counter SF, Florence MG, Hart MJ (2000) A prospective trial of computed tomography and ultrasonography for diagnosing appendicitis in the atypical patient. Am J Surg 182: 379-381. [Crossref]
- Pena BM, Taylor GA, Fishman SJ, Mandl KD (2000) Cost and effectiveness of ultrasonography and limited computed tomography for diagnosing appendicitis in children. Pediatrics 106: 672-676. [Crossref]
- Sivit CJ, Applegate KE, Stallion A, Dudgeon DL, Salvator A et al. (2000) Imaging evaluation of suspected appendicitis in a pediatric population: effectiveness of sonography versus CT. AJR Am J Roentgenol 175: 977-980. [Crossref]
- Wilson EB, Cole JC, Nipper ML, Cooney DR, Smith RW (2001) Computed tomography and ultrasonography in the diagnosis of appendicitis.: when are they indicated? Arch Surg 136: 670-675. [Crossref]
- Wise SW, Labuski MR, Kasales CJ, Blebea JS, Meilstrup JW et al. (2001) Comparative assessment of CT and sonographic techniques for appendiceal imaging. AJR Am J Roentgenol 176: 933-941. [Crossref]
- Raman SS, Lu DS, Kadell BM, Vodopich DJ, Sayre J et al. (2002) Accuracy of nonfocused helical CT for the diagnosis of acute appendicitis: a 5-year review. AJR Am J Roentgenol 178: 1319-1325. [Crossref]
- Stroman DL, Bayouth CV, Kuhn JA, Westmoreland M, Jones RC et al. (1999) The role of computed tomography in the diagnosis of acute appendicitis. Am J Surg 178: 485-489. [Crossref]
- Wijetunga R, Tan BS, Rouse JC, Bigg-Wither GW, Doust BD (2001) Diagnostic accuracy of focused appendiceal CT in clinically equivocal cases of acute appendicitis. Radiology 221: 747-753. [Crossref]
- Wong SK, Chan LP, Yeo A (2002) Helical CT imaging of clinically suspected appendicitis: correlation of CT and histological findings. Clin Radiol 57: 741-745. [Crossref]
- Jacobs JE, Birnbaum BA, Macari M, Megibow AJ, Israel G et al. (2001) Acute appendicitis : comparison of helical CT diagnosis focused technique with oral contrast material versus nonfocused technique with oral and IV contrast material. Radiology 220: 683-690. [Crossref]
- Keyzer C, Tack D, de Maertelaer V, Bohy P, Gevenois PA et al. (2004) Acute appendicitis: comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology 232: 164-172. [Crossref]
- Kim SY, Lee KH, Kim K, Kim TY, Lee HS et al. (2011) Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology 260: 437-445. [Crossref]
- Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY et al. (2017) Comparison of Low- and Standard-Dose CT for the Diagnosis of Acute Appendicitis: A Meta-Analysis. AJR Am J Roentgenol 208: W198-W207. [Crossref]
- Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC (2005) Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology 235: 879-885. [Crossref]
- Keyzer C, Cullus P, Tack D, De Maertelaer V, Bohy P et al. (2009) MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol 193: 1272-1281. [Crossref]
- Benjaminov O, Atri M, Hamilton P, Rappaport D (2002) Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology 225: 400-406. [Crossref]
- Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN et al. (1997) Helical CT technique for the diagnosis of appendicitis : prospective evaluation of a focused appendix CT examination. Radiology 202: 139-144. [Crossref]
- Rao PM, Wittenberg J, McDowell RK, Rhea JT, Novelline RA (1997) Appendicitis: use of arrowhead sign for diagnosis at CT. Radiology 202: 363-366. [Crossref]
- See TC, Watson CJ, Dixon AK, Ng CS (2002) Appendicitis: spectrum of appearace on helical CT. Br J Radiol 75: 775-781. [Crossref]
- Willekens I, Peeters E, De Maeseneer M, de Mey J (2014) The normal appendix on CT: does size matter? PLoS One 9: e96476. [Crossref]
- Mailleux P, Maldague P, Coulier B (2012) Pylephlebitis complicating peridiverticulitis without hepatic abscess: early detection with contrast-enhanced CT of the abdomen. JBR-BTR 95: 13-14. [Crossref]
- Kim HC, Yang DM, Kim SW, Park SJ (2012) Reassessment of CT images to improve diagnostic accuracy in patients with suspected acute appendicitis and an equivocal preoperative CT interpretation. Eur Radiol 22: 1178-1185. [Crossref]
- Baker SR (1997) Unenhanced helical CT versus plain abdominal radiography: a dissenting opinion. Radiology 205: 45-47. [Crossref]
- Park G, Lee SC, Choi BJ, Kim SJ (2014) Stratified computed tomography findings improve diagnostic accuracy for appendicitis. World J Gastroenterol 20: 13942-13949. [Crossref]
- Daly CP, Cohan RH, Francis IR, Caoili EM, Ellis JH et al. (2005) Incidence of acute appendicitis in patients with equivocal CT findings. AJR Am J Roentgenol 184: 1813-1820. [Crossref]
- Madwed D, Mindelzun R, Jeffrey RB Jr (1992) Mucocele of the appendix: imaging findings. AJR Am J Roentgenol 159: 69-72. [Crossref]
- Dixon AK, Goldstone KE (2002) Abdominal CT and the Euratom Directive. Eur Radiol 12: 1567-1570. [Crossref]
- Rao PM, Rhea JT, Novelline RA, Mostafavi AA, Mc Cabe CJ (1998) Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 338: 141-146. [Crossref]
- Poletti PA, Platon A, De Perrot T, Sarasin F, Andereggen E et al. (2011) Acute appendicitis: prospective evaluation of a diagnostic algorithm integrating ultrasound and low-dose CT to reduce the need of standard CT. Eur Radiol 21: 2558-2566. [Crossref]
- Kim K, Kim YH, Kim SY, Kim S, Lee YJ et al. (2012) Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 366: 1596-1605. [Crossref]
- Forsted DH, Kalbhen CL (2002) CT of pregnant women for urinary tract calculi, pulmonary thromboembolism, and acute appendicitis. AJR Am J Roentgenol 178: 1285. [Crossref]
- Fergusson JE, Deangelis GA, Newberry YG, Finnerty JJ, Agarwal S (1996) Fetal radiation exposure is minimal after pelvimetry by modified digital radiography. AM J Obstet Gynecol 175: 260-267. [Crossref]
- Long SS, Long C, Lai H, Macura KJ (2011) Imaging strategies for right lower quadrant pain in pregnancy. AJR Am J Roentgenol 196: 4-12. [Crossref]
- Wieseler KM, Bhargava P, Kanal KM, Vaidya S, Stewart BK et al. (2010) Imaging in pregnant patients: examination appropriateness. Radiographics 30: 1215-1229. [Crossref]
- Bendeck SE, Nino-Murcia M, Berry GJ, Jeffrey RB Jr (2002) Imaging for suspected appendicitis: negative appendectomy and perforation rates. Radiology 225: 131-136. [Crossref]
- van Breda Vriesman AC, Kole BJ, Puylaert JB (2003) Effect of ultrasonography and optional computed tomography on the outcome of appendectomy. Eur Radiol 13: 2278-2282. [Crossref]
- Pickuth D, Heywang-Kobrunner SH, Spielmann RP (2000) Suspected acute appendicitis: is ultrasonography or computed tomography the preferred imaging technique? Eur J Surg 166: 315-319. [Crossref]
- Reddy SB, Kelleher M, Bokhari SAJ, Davis KA, Schuster KM (2017) A highly sensitive and specific combined clinical and sonographic score to diagnose appendicitis. J Trauma Acute Care Surg 83: 643-649. [Crossref]
- Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D et al. (2016) A Systematic Review and Meta-Analysis of Diagnostic Performance of MRI for Evaluation of Acute Appendicitis. AJR Am J Roentgenol 206: 508-517. [Crossref]
- Taourel P, Kessler N, Blayac PM, Lensik A, Gallix B et al. (2002) Imagerie de l’appendice: échographie, scanner ou rien du tout? J Radiol 83 : 1952-1960. [Crossref]
