Hypotension of The Intracranial Circulation with CSF Leakage: A Rare Etiology of Misdiagnosed Orthostatic Headache; Using A Successful Blood Patching Technique: A Case Report and Literature Review
A B S T R A C T
Background: Spontaneous intracranial hypotension (SIH) is typically caused by spontaneous spinal leakage of the CSF, with unknown exact etiology, causing CSF volume depletion and craniospinal elasticity alterations. Often, SIH is misdiagnosed condition.
Case Presentation: A 37-year-old female patient, presented with a four-month history of severe headaches. The first attack of headache, which was preseeded by one month of tinnitus, was in the fifth month of pregnancy. Physical examination and laboratory investigations were unremarkable. Brain MRI with and without contrast revealed thick diffuse meningeal enhancement. The MRA and MRV studies were unremarkable. Then, the patient’s headache worsens despite conservative therapy. MRI myelogram revealed a leak from the cervical nerve roots. Once the location of the leak was confirmed, a cervical epidural blood patch was performed successfully. The postoperative period, four days, was uneventful with clinical improvement of the patient’s headache and tinnitus.
Discussion: Spontaneous intracranial hypotension is a challenging event that requires rapid diagnosis and management. Usually, the clinical history is suggestive of SIH diagnosis but still, it is underdiagnosed. Both imaging modalities and diagnostic criteria are important diagnostic tools for SIH. Several treatment modalities are available, including conservative options, epidural blood patches, and surgical intervention.
Conclusion: Targeted epidural blood patch is a valid approach to managing the SIH that has been performed after a failed trial of conservative measures. We report a 37-year-old patient with a 4-month history of severe headaches and tinnitus found to be caused by SIH and managed by a cervical epidural blood patch.
Keywords
Intracranial hypotension, CSF leak, epidural blood patch, orthostatic headache, low-pressure headache, CSF hypovolemia, myelography
Introduction
Spontaneous intracranial hypotension (SIH) is uncommon but is usually misdiagnosed and co-exists with reduced spinal cerebrospinal fluid (CSF) pressure due to CSF leak [1-3]. With an estimated annual incidence of five in 100,000, SIH is primarily diagnosed in women, peaking at the age of 40 with approximately a female-to-male ratio of 2:1 [1, 2, 4].
SIH is one of the diagnostic dilemmas that physicians face [2, 5]. Variable treatment options are available, including conservative measures, epidural blood patching, and lastly surgical techniques [4, 6, 7]. Multiple studies demonstrate the effectiveness of epidural blood patch (EBP) in managing SIH symptomatology [8, 9]. In our review of the latest english literature worldwide, the terms were used “spontaneous intracranial hypotension”, “CSF leak”, epidural blood patch”, “low-pressure headache”, and “CSF hypovolemia” to search in PubMed. Here we report a 37-year-old female patient who presented with a four-month history of headache and tinnitus.
Case Presentation
A 37-year-old female patient presented with a four-month history of severe headaches. The first attack of headache, which was preseeded by one month of tinnitus, was in the fifth month of pregnancy. The patient’s headache was associated with photophobia. Her headache was continuous and located in the occipital area and occasionally become generalized with a severity scale of 9 out of 10. Its intensity progressively worsens and temporarily gains benefits from regular painkillers and caffeinated beverages. Headache reached its maximum intensity in the seventh month of pregnancy and suddenly subsided in the ninth month of pregnancy. In the postpartum period, headaches started again. Otherwise, she had no other past medical history or similar complaints in her previous pregnancies. Her family history of similar conditions and connective tissue diseases is unremarkable.
The physical examination, including the neuro-ophthalmological assessment, and laboratory investigations were insignificant. The patient reported a history of using combined oral contraceptive pills. Moreover, she had a previous surgical history of gastric bypass surgery in 2009 followed by small bowel resection in 2011 and laparoscopic cholecystectomy in the same year. She had multiple consultations with an otolaryngologist and neurologist with no improvement in her clinical condition. An electrophysiology study was performed, showing normal findings.
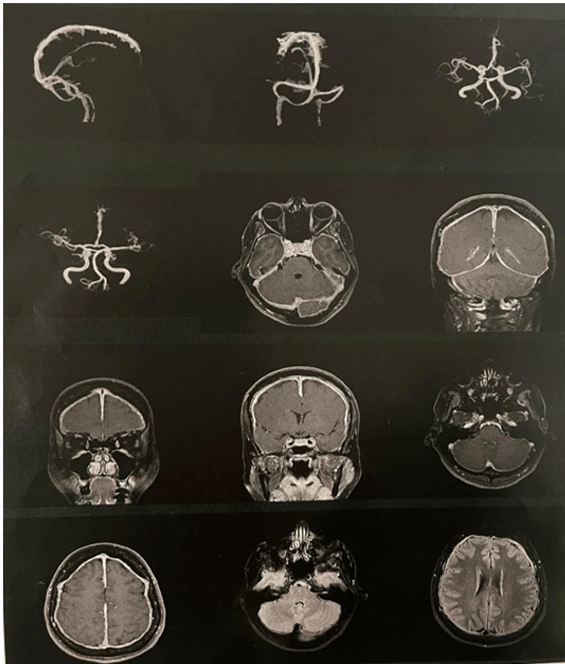
MRI of the brain with and without contrast was done (Figure 1), showing: thick diffuse meningeal enhancement of the entire brain with a vague signal abnormality of possible previous subdural hematoma of peri mesencephalic region and some features concerning mild intra cranial hypotension including slightly reduced pontomesencephalic angle and prominent occipital venous sinus. The MRA and MRV studies were unremarkable.
Figure 1: Brain MRI with and without contrast showed thick diffuse meningeal enhancement of the entire brain with a vague signal abnormality of possible previous subdural hematoma of peri mesencephalic region and some features concerning mild intra cranial hypotension including slightly reduced pontomesencephalic angle and prominent occipital venous sinus.
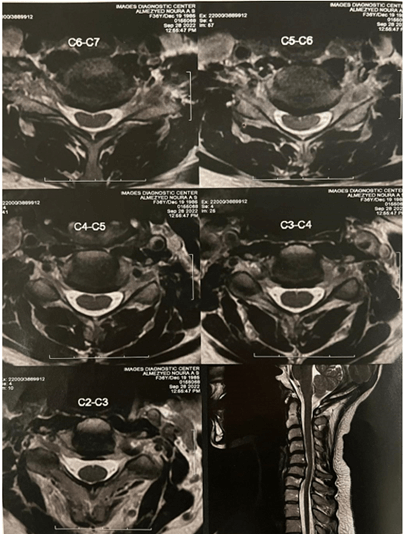
MRI of the whole spine showed an epidural collection, mainly along the posterior and/or the left lateral aspects of the theca opposite to C3-T7. Also, it revealed the suspected site of the CSF leak along the left side nerve sleeves of C5-T1 (Figure 2).
Figure 2: Spinal MRI an epidural collection, mainly along the posterior and/or the left lateral aspects of the theca opposite to C3-T7. Also, it revealed the suspected site of the CSF leak along the left side nerve sleeves of C5-T1.
MRI myelogram revealed a leak from the cervical nerve roots. As a result, the features were suggestive of low-pressure headaches, and conservative therapy was initiated. It includes bed rest, good hydration, and increase caffeine ingestion in order to improve her symptoms. Later, the conservative measures were ineffective and the decision was made to proceed with cervical-targeted EBP.
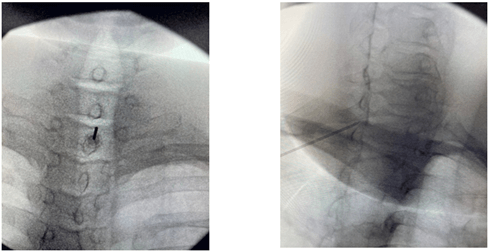
So, after obtaining the consent and explaining the procedure risks, the patient was brought to an AP supine position. Initially, the procedure started by securing the left radial arterial line through a strict aseptic technique using a 20 G needle. Then, the patient’s vitals were monitored using standard ASA monitoring. The X-ray guidance was used to perform the procedure starting with an AP image to locate the C7-T1 interlaminar epidural space followed by freezing the skin with 5cc lidocaine using a 25 G hypodermic needle (Figure 3). After that, an epidural needle 8cm 17 G, tuohy curved epidural needle, was inserted. Loss of resistance was achieved using saline and the depth of the needle was checked using a lateral view. Once loss of resistance was achieved, it was confirmed by 1 ml of omnipaque contrast, in both AP and lateral views. Withdraw 15 ml of the patient’s own blood to the arterial line in a sterile fashion. Then, blood was injected while communicating with the patient and assessing any pressure symptoms. The operating surgeons manage to inject about 14 ml of blood to create the epidural blood patch.
Figure 3: Epidural blood patching under X-ray guidance.
The patient was fully awake during the procedure without sedation, tolerating the procedure well, with mild pressure symptoms around her shoulders which subsided 2 days later. The patient was monitored for 30 minutes in the recovery area and then sent to the floor in stable condition. The postoperative period was uneventful. The patient was discharged after 4 days. She follows up a week later in the neurosurgery outpatient clinic where she reported a 70% improvement in her symptoms.
Discussion
In 1898, the first description of low-pressure CSF headache was made by the anaesthesiologist Bier following the administration of spinal anaesthesia [1, 4]. Then in 1938, George Schaltenbrand is credited with the first description of spontaneous intracranial bleeding as aliquorrhea [1]. According to Dr. William Bell in 1959, there are five types of intracranial hypotension: i) primary or spontaneous, ii) postoperative, iii) head trauma, iv) nerve sleeve tear or post lumbar puncture, and v) secondary to other medical condition [4].
It is now thought that SIH is a volumetric pathology arising from CSF leakage through the arachnoid membrane along the spine. Structural abnormalities from congenital connective tissue disorders, lack of dura around nerve root sheaths, osteophyte protrusions, and spinal disc herniation contribute to leaks [1, 10]. Among those prone to leaks, arachnoid diverticula commonly form in the thoracic and lumbar spine. Sequelae of SIH is due to drops in the CSF volume leading to a decrease in the buoyancy provided to the brain [1, 5]. This leads to sagging within the cranial vault likely causing traction on the sensory nerves of the meninges. According to the Monro-Kellie doctrine, low CSF causes tandem venous dilation and increased blood volume, resulting in a painful stretch of nerve fibers [1]. This compensatory mechanism and traction may contribute to subdural hematomas in patients with SIH [1, 11].
The exact etiology of SIH is unknown [4, 6]. Typically, the spinal CSF leak can be caused by the following etiologies: i) weakness of the dura involving the nerve root sleeves, ii) CSF-venous fistula, and iii) tears of the ventral dura in association with disk herniation [12]. SIH can be triggered by several predisposing factors like connective tissue disorders, trauma, especially valsalva-related events such as straining, heavy lifting, spine disorders, spine disorders, and unknown factors [4, 6]. The underlying cause of SIH was unrecognized in our case.
Postural or orthostatic headache is the hallmark of intracranial hypotension [4, 7, 13, 14]. This kind of headache originates within seconds to hours, improves with recumbency, and worsens with an upright position. It has variable degrees of severity [10, 14]. The associated symptoms are typically due to meningeal irritation such as tinnitus, photophobia, nausea, vomiting, vertigo, neck stiffness, and hearing abnormalities [3, 4, 6, 10]. Also, there have been reports of involvement of the cranial nerves, including diplopia, paresthesias, facial weakness, and taste alteration [1]. Furthermore, there is an association between SIH and compression of the brain and spinal cord structures, causing movement disorders, ataxia, paresis, and reduction in the level of consciousness [1, 13].
In the current case, tinnitus precedes the headache, which is considered very rare, and was first experienced in the fifth month of pregnancy [5]. The patient’s headache was associated with photophobia, continuous, located in the occipital area, and occasionally becoming generalized with a severity scale of 9 out of 10. Its intensity progressively worsens, becoming positional, and temporarily gains benefits from regular painkillers and caffeinated beverages. Headache reached its maximum intensity in the seventh month of pregnancy and suddenly subsided in the ninth month of pregnancy. Then headaches started again in the postpartum period. Ferrante et al. reported that the clinical presentation of continuous headache, instead of orthostatic, preceded by hearing disturbance, and tinnitus, is considered a rare condition [10].
In general, spinal CSF leak is associated with delayed local clinical features, postponing SIH diagnosis [2]. A clinical history can often provide valuable information about a diagnosis [4, 6]. The diagnostic criteria for SIH and CSF leaks in mentioned in (Table 1) [6, 7, 15].
Table 1: Diagnostic criteria for spontaneous
cerebrospinal fluid leak and intracranial hypotension.
|
A:
Demonstration of a spinal CSF leak
Or, if criterion A not met |
|
B: Cranial MRI
changes of intracranial hypotension and the presence of at least one of the
following: 1. Low opening pressure (£ 60 mm H2O) 2. Spinal meningeal diverticulum 3. Improvement of symptoms after epidural
blood patching Or, if criteria A and B not met |
|
C:
The presence of all of the following or a least two of the following if
typical orthostatic headaches are present: 1.
Low opening pressure (£ 60 mm H2O) 2.
Spinal meningeal symptoms 3.
Improvement of symptoms after epidural blood patching |
Imaging studies and lumbar punctures confirm the diagnosis and localization of a CSF leak [4, 16]. Lumbar puncture is an easy bedside test that can be performed. Intracranial hypotension is usually characterized by low opening pressure of 60 mm H2O or less [4]. Elevated both CSF cells and protein levels are expected, indicating increased permeability of dilated meningeal vessels and decreased CSF circulation [4, 16]. This bedside test was not performed on our patient due to the misdiagnosis of SIH as idiopathic intracranial hypertension based on her drug history and vague headache presentation initially.
Imaging involves the following modalities: brain and spinal MRI, CT myelography, and radionuclide cisternography [4, 17]. Brain MRI provides a diagnostic value for intracranial hypotension by demonstrating characteristic radiological findings such as a fluid collection in the subdural space, pachymeningeal enhancement, venous engorgement, brain sagging, and pituitary hyperemia [4, 15, 16]. The detected imaging abnormalities can be illustrated by the Monroe-Kellie hypothesis [4]. In 2003, a study demonstrated that the vast majority of SIH patients revealed diffuse pachymeningeal enhancement, sparing leptomeninges [16].
Moreover, spinal MRI is a crucial modality to detect spinal manifestations like dural enhancement, meningeal diverticula, epidural and intradural veins, C1-C2 retrospinal fluid collection, and extra-thecal CSF collection [4]. CT myelography is the diagnostic method chosen to define the extent and location of the CSF leak. Also, the localization of spinal dural tears by digital subtraction myelography was reported [4, 7]. Radionuclide cisternography is an alternative diagnostic tool that is used to confirm CSF leak in patients with normal CT myelography and clinical suspicion of intracranial hypotension [4, 7]. In our case, the diagnosis of SIH was achieved by the brain and spinal MRI in association with CT myelogram radiological findings, mentioned in the case presentation section.
Several treatment strategies are available to manage SIH. These include conservative measures, targeted epidural blood patches, and lastly surgical treatment [4, 6, 8]. Due to the lack of randomized controlled trials, the choice of treatment depends solely on the preference and expertise of the physician [4]. In general, conservative treatments are ineffective [6, 7]. These treatment options include bed rest, hydration, caffeine ingestion, and analgesia [4, 18]. Couch et al. highlighted different approaches for EBP application, either cervical or lumbar, with no evidence if any of these have a distinct advantage over the others [18]. Our patient started to use caffeinated drinks, caffeine capsules, and magnesium supplemental tablets for more than 2 weeks with no evidence of clinical improvement.
The standard first line of management of SIH is an epidural blood patch [4, 6, 7]. This technique can be considered a diagnostic and therapeutic modality [4]. To achieve the required mechanism of epidural patching, 10-20 ml of blood tend to be used. It acts in the spinal epidural space, restricting the CSF flow, and dural tamponade to seal the CSF leak sites [4, 9] This procedure can be repeated more than once with intervals of 5 days and a large amount of blood should be during the repeated setting [4, 8]. In the presented case, cervical-targeted EBP was performed after a failed trial of conservative options (The intraoperative details of the performed EBP were mentioned in the case presentation section).
In 2011, Cho et al. demonstrated the benefits of repeated EBP sessions for SIH patients [9]. A case series reported SIH cases with variable clinical and radiological features that were treated with EBP, showing complete treatment of the abnormalities [19]. In 2017, Kranz et al. reported three retrospective studies revealed improved outcomes and achievement of successful management of SIH symptoms [12]. Piechwiak et al. reported 88% complete or partial improvement of symptoms in 51 SIH patients treated with EBP [8]. Additionally, Belena et al. published a study of successful authors’ clinical experience of EBP in patients with SIH [13]. In case of failed attempts of epidural blood patch, fibrin sealant placement is advised to provide better symptomatic management [4].
Surgical management is kept as the last option of treatment modalities for those who resist other management plans or are presented with critical situations, requiring urgent surgical intervention [4, 7]. These interventions involve surgical repair of the detected site of the CSF leak [4]. The majority of patients with spontaneous intracranial hypotension experience positive outcomes while a 10% risk of headache recurrence was reported. Studies demonstrate a good prognosis among patients with abnormal cranial MRI that is associated with identified CSF leak [4]. In 2020, Villamil et al. highlighted a higher recurrence rate of SIH among patients with brain MRI findings of the distorted brainstem, collapsed ventricle, and posterior fossa crowding [15]. On the other hand, rebound intracranial hypertension was reported after successful treatment of CSF leakage that is temporary and resolved after days or months [4, 7].
Conclusion
SIH is considered a diagnostic challenge and dilemma that can be managed conservatively, by minimal invasive epidural blood patching, or surgically. The current case demonstrates the role of epidural blood patching in symptomatology and management. Due to the low incidence of SIH, documentation of such cases is highly encouraged the documentation of such cases to enhance the identification of the SIH presentation spectrum that is essential to the diagnosis and treatment of patients accurately and in a timely manner.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 08, May 2023Accepted: Wed 31, May 2023
Published: Mon 12, Jun 2023
Copyright
© 2023 Athary Saleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.02.05
Author Info
Athary Saleem Saqer Alenezi Hasan Behbehani Ayoub Dackson
Corresponding Author
Athary SaleemNeurosurgery Department, Jaber Al Ahmad Hospital, State of Kuwait
Figures & Tables
Table 1: Diagnostic criteria for spontaneous
cerebrospinal fluid leak and intracranial hypotension.
|
A:
Demonstration of a spinal CSF leak
Or, if criterion A not met |
|
B: Cranial MRI
changes of intracranial hypotension and the presence of at least one of the
following: 1. Low opening pressure (£ 60 mm H2O) 2. Spinal meningeal diverticulum 3. Improvement of symptoms after epidural
blood patching Or, if criteria A and B not met |
|
C:
The presence of all of the following or a least two of the following if
typical orthostatic headaches are present: 1.
Low opening pressure (£ 60 mm H2O) 2.
Spinal meningeal symptoms 3.
Improvement of symptoms after epidural blood patching |
References
1.
Upadhyaya
P, Ailani J (2019) A Rreview of Spontaneous Intracranial Hypotension. Curr Neurol Neurosci Rep 19: 22. [Crossref]
2. Schievink WI (2006)
Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. Jama 295: 2286-2296. [Crossref]
3. Hughes J, Chavez B
(2022) Magnetic Resonance-Guided Diagnosis of Spontaneous Intracranial
Hypotension in a Middle-Aged Woman. Case
Rep Neurol Medi 2022:
4438923. [Crossref]
4. Limaye K, Samant R,
Lee RW (2016) Spontaneous intracranial hypotension: diagnosis to management. Acta Neurol Belg 116: 119-125. [Crossref]
5. Ferrante E,
Trimboli M, Rubino F (2020) Spontaneous intracranial hypotension: review and
expert opinion. Acta Neurol Belg 120: 9-18. [Crossref]
6. Friedman DI (2018)
Headaches due to low and high intracranial pressure. Continuum (Minneap Minn) 24:
1066-1091. [Crossref]
7. D’Antona L, Merchan
MAJ, Vassiliou A, Watkins LD, Davagnanam I et al. (2021) Clinical presentation,
investigation findings, and treatment outcomes of spontaneous intracranial
hypotension syndrome: a systematic review and meta-analysis. JAMA Neurol 78: 329-337. [Crossref]
8. Piechowiak EI,
Aeschimann B, Häni L, Kaesmacher J, Mordasini P et al. (2022) Epidural Blood
Patching in Spontaneous Intracranial Hypotension-Do we Really Seal the Leak? Clin Neuroradiol 33: 211-218. [Crossref]
9. Cho KI, Moon HS,
Jeon HJ, Park K, Kong DS (2011) Spontaneous intracranial hypotension: efficacy
of radiologic targeting vs blind blood patch. Neurology 76:
1139-1144. [Crossref]
10. Schievink WI,
Deline CR (2014) Headache secondary to intracranial hypotension. Curr Pain Headache Rep 18: 457. [Crossref]
11. Bond KM, Benson JC,
Cutsforth Gregory JK, Kim DK, Diehn FE et al. (2020) Spontaneous intracranial
hypotension: atypical radiologic appearances, imaging mimickers, and clinical
look-alikes. AJNR Am J Neuroradiol 41: 1339-1347. [Crossref]
12. Kranz PG, Malinzak
MD, Amrhein TJ, Gray L (2017) Update on the diagnosis and treatment of
spontaneous intracranial hypotension. Curr
Pain Headache Rep 21: 37. [Crossref]
13. Beleña JM, Nuñez M,
Yuste J, Plaza Nieto JF, Jiménez Jiménez FJ et al. (2012) Spontaneous
intracranial hypotension syndrome treated with a double epidural blood patch. Acta Anaesthesiol Scand 56: 1332-1335. [Crossref]
14. Luetzen N, Dovi
Akue P, Fung C, Beck J, Urbach H (2021) Spontaneous intracranial hypotension:
diagnostic and therapeutic workup. Neuroradiology
63: 1765-1772. [Crossref]
15. Villamil F, Ruella
M, Perez A, Vernetti PM, Formenti MEP et al. (2020) Traumatic vs Spontaneous
Cerebrospinal Fluid Hypotension Headache: Our experience in a series of 137
cases. Clin Neurol Neurosurg 198: 106140. [Crossref]
16. Schievink WI (2003)
Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol 60:
1713-1718. [Crossref]
17. Farb RI, Nicholson
PJ, Peng PW, Massicotte EM, Lay C et al. (2019) Spontaneous intracranial
hypotension: a systematic imaging approach for CSF leak localization and
management based on MRI and digital subtraction myelography. AJNR Am J Neuroradiol 40: 745-753. [Crossref]
18. Couch JR, Persson J (2012) Treatment of spontaneous intracranial hypotension with epidural blood patch: is a complex approach necessary or better than a simple one? Acta Anaesthesiol Scand 56: 1207-1209. [Crossref]
19. Renowden SA, Gregory R, Hyman N, Hilton Jones D (1995) Spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry 59: 511-515. [Crossref]
