Journals
How to Suspect and Manage an Hypoplasic Gallbladder: A Case Report and Review of Literature
A B S T R A C T
Background: Malformations related to the gallbladder are uncommon, with an incidence lower than 0,1%. The majority of them are asymptomatic, however when symptoms appear are non-specific with a similar presentation to biliary colic.
Methods: We report a case of a 29-year-old woman with persistent upper right abdominal pain and no visualization of the gallbladder in the ultrasound (US), CT scan or in the magnetic resonance cholangiopancreatography (MRCP).
Results: A laparoscopic exploration was performed due to persistent abdominal pain which confirmed an hypoplasic gallbladder. After cholecystectomy, symptoms were relieved. Herein we propose a decisional algorithm when suspecting a gallbladder with agenesis or hypoplasia.
Conclusion: Surgeons need to take into consideration congenital anomalies of the gallbladder. Performing imaging techniques is important in order not to misdiagnose hypoplasia.
Keywords
Gallbladder agenesis, malformation, hypoplasia, cholecystectomy
Introduction
Congenital gallbladder anomalies are infrequent, with gallbladder agenesis reported to have an incidence of 0.01% to 0.06% [1]. However, gallbladder hypoplasia is even less common, and its incidence is not well known. This condition is usually asymptomatic. However, when symptoms appear, they are non-specific and similar to biliary colic. Clinicians may suspect this pathology when the gallbladder is not visualized in the ultrasound, because further tests might be required [2, 3].
Case Report
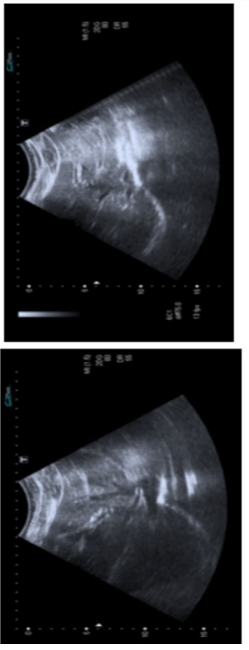
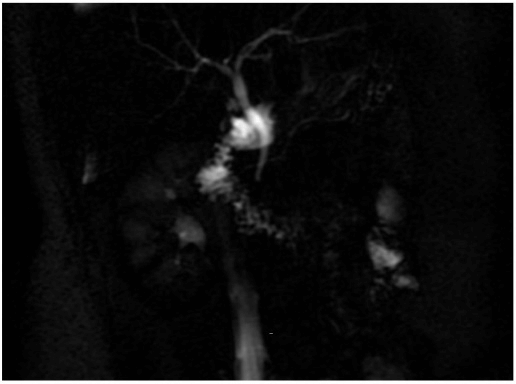
We present the case of a 29-year-old woman without previous medical history that presented a persistent, non-irradiated upper right abdominal pain for one week. It was associated with low-grade fever, nausea and vomiting. Physical examination revealed negative Murphy sign without tenderness. Biochemical investigations demonstrated no alterations in liver and pancreatic parameters. An ultrasound was performed showing no dilatation of the intrahepatic and extrahepatic bile ducts. It was not possible to visualize the gallbladder (Figure 1). During admission, the patient presented a favorable evolution after conservative treatment. Nevertheless, a residual pain was still referred and because of that a magnetic resonance cholangiopancreatography (MRCP) was performed, showing a normal bile duct with a diameter of 4 millimeters. The cystic duct was irregular and the gallbladder was not evidenced (Figure 2). Suspecting the presence of an hypoplasic gallbladder, a laparoscopic exploration was carried out. After inspection of the hepatic hilum and Calot’s triangle, an hypoplasic gallbladder was identified and a cholecystectomy was carried out using the Critical View of Safety method (Figure 3). A millimetric artery was identified and coagulated. The cystic duct was clipped and divided (Figure 4).
The postoperative course was uneventful, with the patient discharged at 24 hours. One year later she remains asymptomatic. The specimen was sent for pathology resulting in a rudimentary gallbladder presenting a chronic cholecystitis (Figure 4).
Figure 1: Ultrasound image revealing the absence of gallbladder.
Figure 2: MRCP image showing no visualization of the gallbladder.
Figure 3: Intraoperative image. Hypoplasic gallbladder measuring 1 centimeter.
Figure 4: Hypoplasic gallbladder after cholecystectomy.
Discussion
The gallbladder hypoplasia is known as the underdevelopment of the gallbladder and it is extremely uncommon. There are just a few cases reported in the literature [4, 5]. As other congenital gallbladder anomalies, it is usually diagnosed in children or young adults. In some cases, it may be an incidental discovery in the elderly. It is associated with other gallbladder malformations such as multiseptate gallbladder and also with other conditions such as cystic fibrosis, neonatal hepatitis, cholangitis and biliary atresia [5]. When it causes symptoms, they are commonly abdominal pain in the right upper quadrant, nausea, vomiting, dyspepsia and jaundice. Although these are non-specific symptoms, clinicians should suspect it when a patient without surgical history refers persistent upper-right abdominal pain and no gallbladder is identified in imaging techniques. Due to the lack of accuracy in preoperative imaging techniques, an hypoplasia might be erroneously diagnosed as gallbladder agenesis and the patient will remain symptomatic. We suggest performing a laparoscopic exploration.
Although Frey et al. proposed in 1960 that it can only be diagnosed by surgery, nowadays there are different radiological modalities when studying gallbladder diseases. Despite the high resolution of diagnostic imaging techniques, it is very difficult to make an accurate preoperative diagnosis of gallbladder hypoplasia in symptomatic patients. Usually ultrasonography is the gold standard investigation to initiate the examinations of the gallbladder (sensibility of 95%). However, it is difficult to diagnose it only by ultrasound [6]. Several authors recommend conducting a magnetic resonance cholangiopancreatography (MRCP), an endoscopic retrograde cholangiopancreatography (ERCP) or a TC scan [4]. ERCP is the gold standard to examine the biliary anatomy, nevertheless it is an invasive technique and it can cause injuries to biliary tract. In opposition, MRCP is a non-invasive and specific imaging method in the evaluation of the biliary tract and it is more accurate in the diagnosis of gallbladder malformations in comparison to ERCP. It also gives information about other biliary malformations that increase the risk of iatrogenesis during the abdominal surgery such as vascular malformations or an intrahepatic or a left-sided gallbladder [4].
Unlike gallbladder agenesis, gallbladder hypoplasia needs surgery in almost all cases in order to make the diagnosis like in our patient where ultrasound was not able to visualize the gallbladder and other imaging techniques were inconclusive. Gallbladder hypoplasia can lead to intraoperative injury of the common bile duct or other parts of the biliary tree as a result of false identification of these structures. It is essential during surgery to ensure that no structure is divided until a clear picture of the bile ducts and blood vessels is obtained [7]. In the case of a complicated dissection, it might be helpful to perform an intraoperative cholangiogram which defines biliary system anatomy, convert to an open cholecystectomy procedure or even discontinue the intervention. Further tests might be required to avoid iatrogenesis [4]. Because of that, the use of laparoscopy for definitive treatment of gallbladder disease obliges us to be familiar with different kinds of biliary malformations and to always consider them whenever we find something unusual. When the anatomy of the biliary tree is not normal, we should think about the possibility of a biliary malformation and dissection should proceed with extreme caution. Some authors support a conversion to open surgery in order to enhance the identification of the biliary structures. Yet, converting surgery could only add comorbidities to the procedure without any benefit [5, 8].
Differently to gallbladder agenesis, there are no specific guidelines to manage these patients [9, 10]. We propose a decisional algorithm when suspecting agenesis or hypoplasia of the gallbladder (Figure 5). We recommend to perform surgical exploration and a cholecystectomy. Contrarily these patients might remain unconcluded and persistently symptomatic. Some studies have determined that after cholecystectomy these patients remain asymptomatic [6].
Figure 5: Decisional algorithm of persistent upper-right abdominal pain.
Conclusion
Congenital abnormalities of the gallbladder are rare conditions and difficult to diagnose with imaging techniques. Gallbladder hypoplasia is a very unusual anomaly which must be kept in mind when is not possible to visualize gallbladder in the US in a patient with persistent upper-right abdominal pain. We propose a decisional algorithm when suspecting these malformations.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Wed 05, Aug 2020Accepted: Mon 17, Aug 2020
Published: Thu 03, Sep 2020
Copyright
© 2023 David Martínez Cecilia. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.03.09
Author Info
Anna Trinidad Borràs Jara Hernández Gutiérrez David Martínez Cecilia
Corresponding Author
David Martínez CeciliaComplejo Hospitalario de Toledo, Toledo, Spain
Figures & Tables



References
- Pashtoon Murtaza Kasi, Raymund Ramirez, Shari S Rogal, Kailey Littleton, Kenneth E Fasanella (2011) Gallbladder Agenesis. Case Rep Gastroenterol 5: 654-662. [Crossref]
- Nicolas Peloponissios, Michel Gillet, Rene Cavin, Nermin Halkic (2005) Agenesis of the gallbladder: A dangerously misdiagnosed malformation. World J Gastroenterol 11: 6228-6231. [Crossref]
- Hamed Kabiri, Orville H Domingo, Chris D Tzarnas (2006) Agenesis of the Gallbladder. Curr Surg 63: 104-106. [Crossref]
- Christophoros S Kosmidis, Georgios D Koimtzis, Maria S Kosmidou, Fotini Ieridou, Triantafyllia Koletsa et al. (2017) Gallbladder Hypoplasia, a Congenital Abnormality of the Gallbladder: A Case Report. Am J Case Rep 18: 1320-1324. [Crossref]
- P K Jena, R A Hardie, M Hobsley (1977) Multiseptate hypoplastic gallbladder. Br J Surg 64: 192-193. [Crossref]
- Sachin Malde (2010) Gallbladder agenesis diagnosed intra-operatively: a case report. J Med Case Rep 4: 285. [Crossref]
- Santosh Balakrishnan, Tarun Singhal, Starlene Grandy Smith, Shamsi El Hasani (2006) Agenesis of the gallbladder: lessons to learn. JSLS 10: 517-519. [Crossref]
- Giuseppe Bianco, Francesco Frongillo, Salvatore Agnes, Erida Nure, Nicola Silvestrini (2018) Gallbladder agenesis: A case report and brief review. Ann Hepatobiliary Pancreat Surg 22: 292-295. [Crossref]
- Eugenio Tagliaferri, Heinrich Bergmann, Sebastian Hammans, Aziz Shiraz, Eckhard Stüber et al. (2017) Agenesis of the Gallbladder: Role of Clinical Suspicion and Magnetic Resonance to Avoid Unnecessary Surgery. Case Rep Gastroenterol 10: 819-825. [Crossref]
- Atul Kumar Mittal, Dhananjay Saxena, Raju Kadam, Prashant Garg, Jeevan Kankaria et al. (2015) Agenesis of gallbladder: A diagnostic dilemma. Int J Case Rep Images 6: 296-300.
