Hemorrhagic Shock from Massive Retroperitoneal and Pelvic Hematoma After Stapled Hemorrhoidopexy
A B S T R A C T
Background: Massive retroperitoneal and pelvic hematoma leading to hemorrhagic shock following stapled hemorrhoidectomy is rare. To the best of our knowledge at the time of this publication, there are no reported cases of postoperative pelvic or retroperitoneal hematoma without intraluminal bleeding reported after stapled hemorrhoidopexy. We describe such a case in a patient with grade III internal hemorrhoid who was treated with colonoscopy and stapled hemorrhoidectomy.
Case Summary: A 64-year-old female with a past medical history significant for deep vein thrombosis and pulmonary embolism for which she was anticoagulated with warfarin presented with hemorrhoids and rectal bleeding and associated iron deficiency anemia. The warfarin was held five days prior to the planned combined colonoscopy and hemorrhoidectomy procedure. While still recovering in the post-anaesthesia care unit (PACU) a few hours post-operatively, she was found to be hypotensive, tachycardic, and somnolent. A CT abdomen/pelvis was obtained, which identified a large collection of blood in the pelvis and retroperitoneum. She was taken back to the OR for an emergent exploratory laparotomy and flexible sigmoidoscopy. She was admitted to the ICU where she required placement on BiPAP for respiratory acidosis and resuscitation with a total of seven units of pRBCs and two units of FFP. She was clinically stable three days later.
Conclusion: In a patient with a history of chronic anticoagulation, one should consider intraluminal, retroperitoneal, and pelvic bleeding if the patient is in hemorrhagic shock after stapled hemorrhoidectomy. Furthermore, one should not rule out the possibility of retroperitoneal or pelvic bleeding even if there is no evidence of intraluminal bleeding. Emergent laparotomy and sigmoidoscopy may be considered for unstable patients with unidentified external bleeding.
Keywords
Hemorrhoidopexy, hemorrhoidecotomy, PPH, laparotomy, hemorrhagic shock, laparotomy
Introduction
Stapled hemorrhoidopexy, also known as Procedure for Prolapsed Hemorrhoids (PPH) is a transanal circular stapling technique that has been used as a treatment of hemorrhoidal disease for more than two decades. The technique uses circumferential rectal mucosectomy and mucosal lifting to reconstitute healthy anatomical and physiological aspects of the hemorrhoidal plexus [1]. Thus, it restores fixation of hemorrhoidal cushions to the underlying internal sphincter, reduces hemorrhoidal prolapse and minimizes hemorrhoidal blood flow [2]. PPH provides a shorter operative time and less painful alternative to excisional hemorrhoidectomy and is associated with an earlier return to normal activity [3, 4]. Common complications of this procedure are higher recurrence rates, rectal bleeding, tenesmus, and fecal urgency [5, 6].
We report a case of hemorrhagic shock as an early postoperative complication of a stapled hemorrhoidectomy. The patient ultimately required laparotomy and balanced fashion in our intensive care unit. This case highlights the importance of consideration of retroperitoneal and pelvic hematoma after PPH, especially in patients with a history of anticoagulation use.
Case Presentation
A 64-year-old female presented to our clinic with iron deficiency anemia in the setting of hemorrhoids and rectal bleeding. The patient had a history of recurrent, prolonged hemorrhoidal bleeding, for which surgery was indicated. She had a history of recurrent venous thromboembolism (DVT and pulmonary embolism) for which she was on warfarin with a target INR range of 2.0 to 3.0 since 2014. Her INR prior to surgery was within her target range. Other significant medical history included left-sided breast cancer (T2N0M0) diagnosed in 2010, three episodes of DVT, and two episodes of pulmonary embolism (most recently on 2018). She had undergone a hysterectomy in 1982, hiatal hernia repair in 2010, and partial mastectomy with chemotherapy and radiotherapy for breast cancer in 2011.
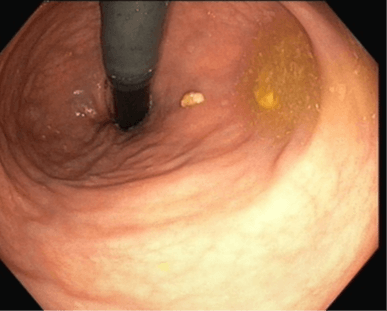
The patient was scheduled for a colonoscopy and PPH (circular stapled hemorrhoidectomy) after holding warfarin and bridging with heparin. She did not have any history of adverse reactions to heparin or heparin products and had previously undergone heparin bridging multiple times without complications. Under general anaesthesia, the colonoscopy noted hemorrhoids and no other pathologies to explain her lower gastrointestinal bleeding, serving as an indication for PPH (Figure 1). A circular stapled hemorrhoidectomy/hemorrhoidopexy was performed in the usual fashion. The circular anoscope was placed over the dentate line. A Prolene purse string suture was placed at about 3 cm proximal to the dentate line. The 33 mm circular stapler anvil was placed in the lumen of the rectum and the purse string was tied against it. The stapler was assembled, closed completely, and kept closed for 30 seconds. The posterior vaginal wall and septum were inspected, noted to be free from the stapler, then the stapler was fired. The staple line was intact and some minor bleeding was noted, which was controlled with 2-0 Vicryl sutures. The vaginal posterior wall and septum were inspected again along with proctoscopic evaluation. No abnormalities were identified. The patient was brought to the PACU for observation with the plan for same-day discharge.
Figure 1: Retroflex view of hemorrhoids on colonoscopy.
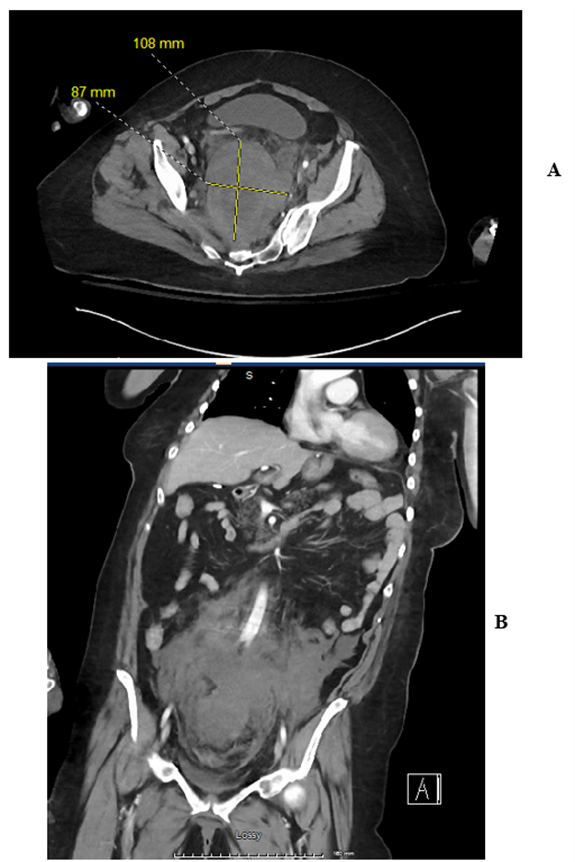
Three hours after the procedure, the patient was tachycardic, hypotensive, and complained of abdominal pain and distension. A CT of the abdomen and pelvis with IV and without oral contrast was performed and demonstrated a large pelvic and retroperitoneal hematoma with the largest component measuring up to 8.7 × 10.8 cm (Figures 2A & 2B). There was no active extravasation of contrast seen on the scan suggesting slow venous bleeding.
The patient was emergently taken from PACU back to the OR. The rectal examination did not identify any intraluminal bleeding. Laparotomy was performed, which showed retroperitoneal and pelvic hematoma. There were no injuries to the colon or small bowel and the intra-abdominal compartment was free of fluid or blood. Flexible sigmoidoscopy showed an intact PPH staple line without any bleeding component. Two 19 French blake drains were placed intra-abdominally in the paracolic gutters. The patient was extubated and brought to the ICU postoperatively. She required seven units of pRBCs, two units of FFP, and BiPAP for respiratory acidosis. She was downgraded to the surgical floor on postoperative day three and was discharged postoperative day seven.
Figure 2: A) Large post retroperitoneal hematoma seen on axial CT imaging following PPH. B) Large retroperitoneal hematoma seen on coronal CT imaging following PPH.
Discussion
Hemorrhoidal disease is one of the most common benign proctological conditions. It is estimated that the prevalence of hemorrhoids in the United States is 4.4%, with peak prevalence in age 45-65 years [7]. Many have sought to optimize the non-operative and operative management of hemorrhoids. Invasive surgical approaches include hemorrhoidectomy and stapled hemorrhoidopexy (PPH). Stapled hemorrhoidopexy was first introduced for the management of hemorrhoids by Longo in 1998 [1]. The technique was popularized due to its short operative time and reduced post-operative pain, which allowed for early return to normal activity compared with the Milligan-Morgan hemorrhoidectomy [3, 8]. One study in the United Kingdom found it less costly compared to conventional hemorrhoidectomy [9]. Though widely popular, stapled hemorrhoidopexy has not become the gold standard procedure for hemorrhoids due to the higher rates of recurrence, subsequent need for reoperation, and reports of severe adverse events [5, 6].
The most common complication following PPH is rectal bleeding, ranging from 1% to 11%, according to a 2008 review article [5]. Most bleeding resolves on its own, with 5.6% requiring readmission and only 1.8% requiring re-treatment (surgical or endoanal epinephrine injection). Bleeding after hemorrhoidopexy occurs more frequestly than hemorrhoidectomy and the risk is further increased after a PPH for fourth-degree hemorrhoids (11%) [5]. According to an anatomical dissection study done by Aigner et al., neither PPH nor doppler ligation completely interrupts the superior rectal artery branches [10]. This risk is even higher in patients with anticoagulation therapy.
One randomized controlled trial showed that biological glue application after stapled hemorrhoidopexy significantly decreased post-operative complications such as anal canal stenosis and postoperative hemorrhage after PPH [11]. Another 2017 retrospective study demonstrated that biological glue application after PPH in high-risk patients decreased the rates of bleeding in the postoperative period. However, in the case of our patient, the interventions outlined in these studies would not have improved our outcome as our patient did not have any notable mucosal bleeding under sigmoidoscopy and the bleeding was noted to be only in the presacral retroperitoneal space. Visible bleeding during the index operation was controlled by suture ligation.
In conclusion, patients can develop significant retroperitoneal, and pelvic bleeding after PPH ,which, to our knowledge, is not frequently discussed in the literature. A high index of suspicion and broad differential diagnosis may be required to acutely identify occult hemorrhagic shock in therapeutically anticoagulated patients following PPH. In such circumstances, rapid identification of the source of bleeding and intervention to stop it are critical to preventing life-threatening complications.
Article Info
Article Type
Case ReportPublication history
Received: Mon 18, Jul 2022Accepted: Fri 12, Aug 2022
Published: Mon 31, Oct 2022
Copyright
© 2023 Diwakar Phuyal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2022.02.02
Author Info
Diwakar Phuyal Elizabeth Jacob Lydia Rafferty Eunice S. Yang Luis Oceguera Raul Monzon
Corresponding Author
Diwakar PhuyalBassett Medical Center, Cooperstown, New York, USA
Figures & Tables
References
1. Longo A (1998)
Treatment of hemorrhoids disease by reduction of mucosal Prolapse and
hemorrhoidal Prolapse with a circular suturing device; a new procedure. Proc
6th Congress of Endoscopic Surgery, Rome/Italy.
2. Hussein AM (2001)
Ligation-anopexy for treatment of advanced hemorrhoidal disease. Dis Colon
Rectum 44: 1887-1890. [Crossref]
3. Mehigan BJ, Monson
JR, Hartley JE (2000) Stapling procedure for haemorrhoids versus
Milligan-Morgan haemorrhoidectomy: randomised controlled trial. Lancet
355: 782-785. [Crossref]
4. Thaha MA, Campbell
KL, Kazmi SA, Irvine LA, Khalil A et al. (2009) Prospective randomised
multi-centre trial comparing the clinical efficacy, safety and patient
acceptability of circular stapled anopexy with closed diathermy
haemorrhoidectomy. Gut 58: 668-678. [Crossref]
5. Pescatori M,
Gagliardi G (2008) Postoperative complications after procedure for prolapsed
hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech
Coloproctol 12: 7-19. [Crossref]
6. Giordano P,
Gravante G, Sorge R, Ovens L, Nastro P (2009) Long-term Outcomes of Stapled
Hemorrhoidopexy vs Conventional Hemorrhoidectomy: A Meta-analysis of Randomized
Controlled Trials. Arch Surg 144: 266-272. [Crossref]
7. Johanson JF,
Sonnenberg A (1990) The prevalence of hemorrhoids and chronic constipation. An
epidemiologic study. Gastroenterology 98: 380-386. [Crossref]
8. Rowsell M, Bello M,
Hemingway DM (2000) Circumferential mucosectomy (stapled haemorrhoidectomy)
versus conventional haemorrhoidectomy: randomised controlled trial. Lancet 355:
779-781. [Crossref]
9. Ribarić G, Kofler
J, Jayne DG (2011) Stapled hemorrhoidopexy, an innovative surgical procedure
for hemorrhoidal prolapse: cost-utility analysis. Croat Med J 52:
497-504. [Crossref]
10. Aigner F, Bodner G, Gruber H, Conrad F, Fritsch H et al. (2006) The vascular nature of hemorrhoids. J Gastrointest Surg 10: 1044-1050. [Crossref]
11. Anghelacopoulos SE, Tagarakis GI, Pilpilidis I, Kartsounis C, Chryssafis G (2006) Albumin-glutaraldehyde bioadhesive (“Bioglue”) for prevention of postoperative complications after stapled hemorrhoidopexy: a randomized controlled trial. Wien Klin Wochenschr 118: 469-472. [Crossref]
