Hair Transplantation in Cicatricial Alopecia: The Role of Autologous Fat Transfer
Hair Transplantation in Cicatricial Alopecia: The Role of Autologous Fat Transfer
A B S T R A C T
Aim: The purpose of this article is to prove the importance of autologous fat transfer (AFT) in scarring alopecia.
Methods: We present a complete clinical report of 21 cases treated with a combined procedure of AFT and hair transplantation (HT) done in the last three years.
Results: The main findings of this study are the constant, early and more predictable hair regrowth after the hair transplant done on a pre-treated scarring alopecia.
Conclusion: Tissue regeneration through AFT can significantly improve hair growth in the area of scarring alopecia, underlining, once again, the tremendous potential of this approach. Future studies may need to be carried out.
Keywords
Cicatricial alopecia, hair transplantation, scalp burns, scalp radiotherapy, adipose-derived stem cells, autologous fat transfer, stromal-vascular fraction, tissue defect, regeneration, clinical applications
Background
In order to give a realistic introduction to this article, a brief digression is necessary: if a patient with cicatricial alopecia, (scalp, beard, eyebrows, etc.) wanted nowadays to find out which reconstructive options were available, his search would be difficult. Assuming he finds a few specialists with the highest expertise, he would most likely have to compare very different treatment plans. The answers he would receive are an honest reflection of the different backgrounds of the specialists involved in this field. Among them are doctors of different specialties: wigs specialists, a professional category that is often consulted by these patients as first choice; scalp micropigmentation specialists (SMP) who offer a rapid disguise solution that, especially for men, is very common nowadays (Table 1).
Table 1: Range of specialists who may be consulted for cicatricial alopecia.
|
DOCTORS |
NON-MEDICAL DOCTORS |
||
|
Maxillo Facial Surgeons |
Plastic Surgeons |
Aesthetics Surgeons |
Wigs / Prosthetics |
|
Neurosurgeon |
Radio Therapist |
Dermatologist |
SMP Specialist |
So many options often generate a great deal of uncertainty and the fear of not making the right choice. This uncertainty can, in the worst-case scenarios, turn into a paralysing confusion and it is not uncommon to visit patients who have been living with their scars for years. For a patient to make a peaceful choice, it is necessary to align their personal indications with the different reconstructive treatment plans that exist today for this pathology. This article wants to emphasize a reconstructive sequence that combines AFT and hair transplantation as an innovative and effective option.
Introduction
For many years the relative advantages of autologous scar transplantation, compared to skin expansion, was the subject of controversy because the reliability of the two procedures appeared to be different [1]. Moreover, only a few surgeons were able to perform these procedures correctly and, in many cases, the transplanted hair grew back but differed from expectations in number and quality. Today, hair transplantation (HT) is the primary indication for the coverage of the majority of cicatricial alopecia. The previous limits of its applicability have been extended and should be redefined. In the last 4 years the increase of all HT operations worldwide has been exponential and ISHRS statistics show that 2% are performed on scars (ISHRS Survey 2018) [2]. How is it possible to achieve similar results to those achievable in non-scarring alopecia? When the greatest obstacle is represented by the qualitative impairment of the receiving tissue, the adoption of regenerative medicine plans represents a real and sustainable solution to recreate the right suitability of the scar tissue for surgery.
We present this first clinical work for three main reasons:
i. Describe how the AFT technique, Microfat (Micro) and Lipostructure (Lips), is able to induce an improvement in the quality of scarring recipient areas.
ii. Specify the reasons, indications and scientific backgrounds behind the adoption of this choice.
iii. Present our clinical experience highlighting both the wide variety of indications for the use of adipose tissue, as well as the patient selection criteria, surgery plans and various technical notes.
If the exact regenerative mechanism by which the stem component of adipose tissue acts remains unclear, we have observed that the proposed approach produces a formidable effect on the follicular structure. In the field of hair care and surgery the potential of these regenerative procedures is tremendous, and few first report are available [3, 4]. It is rare, as it is shown in (Table 2), for these skills to flow into a single subject, and these patients can only be managed by open professional co-operation. This work, which stems from these synergies aims to promote this multidisciplinary approach.
Table 2: Data from Practice census survey ISHRS-2018.
|
ORIGINAL MEDICAL SPECIALTY OF HAIR TRANSPLANT SURGEONS |
% |
|
Plastic Surgery |
19,1 |
|
Cosmetic Surgery |
12,1 |
|
Maxillo-Facial Surgery |
2,7 |
|
OTHER |
66,1 |
|
Practice Census Survey ISHRS - 2018 |
|
Materials and Methods
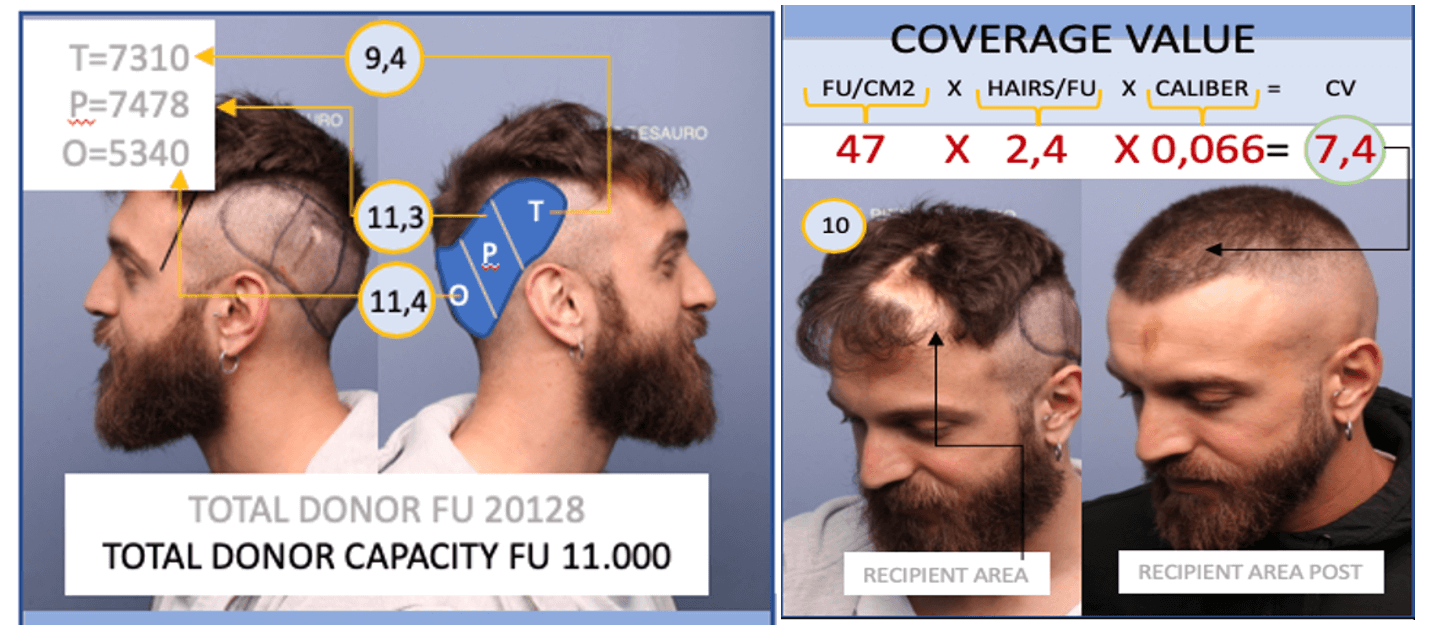
In the last three years we have observed 30 patients with scarring alopecia of the scalp or facial areas. Of these 30, 21 have completed the procedures and are now at a minimum distance of 6 months from the date of HT. 9 patients are still undergoing treatment and have been excluded from this study. Patients enrolled for this procedure plan presented one or more clinical evidence of reduced wound thickness, impaired tissue trophism, altered circulatory function and structural abnormalities with particular reference to adherence to the deep planes. Possible comorbidities were investigated through dermatoscopy and treated before the procedures were performed. Moreover, to accurately define the worth of HTs, all patient in this study underwent to a coverage value (CV), a routine investigation we have identified as an important tool to meet this purpose. The CV is a method to measure the total donor capacity (TDC) of a patient during the preliminary assessment. TDC is the maximum number of FUs that a surgeon can harvest (respecting the hairs/FU ratio) in each procedure while avoiding depletion. It is based on an arithmetical calculation using quantitative (number of FU/cm2 e number of hair/FU) and qualitative (hair caliber) data. The CV is the ratio of Hair/cm2 multiplied by the Average Caliber of the FU. A CV of 5, 4 is the value that represents the lightest coverage necessary to reach a good aesthetic result (Table 3). So far, we can determine how many grafts will be required in the recipient area in order to allow a minimum coverage or a specific coverage value [4, 5]. This density will come from the grafts placed and a precise calculation of the real recipient area (which can often differ from the perceived recipient area) [5].
Table 3: Coverage value formula.
|
$$CV=\frac{FU}{{cm}^2}x\frac{Hair}{FU}x\ Caliber$$ |
|
Cleaning the formula .. |
|
$$CV={cm}^2x\ Hair\ x\ Caliber$$ |
|
COVERAGE VALUE FORMULA |
This data will also help to choose if HT will cover completely or partially the scar, using the available resources to transplant exclusively the areas of primary importance from an aesthetic perspective. More importantly, within this specific use on unhealthy tissue, it highlights what useful reserve of follicles the patient has in case of partial success of the procedure. The CV analysis takes about 30 minutes. Recently two apps have been proposed in order to increase the speed and the accuracy of this procedure [6, 7]. An example of CV calculation is shown in (Figure 1). Of the 21 patients examined for the purpose of this study, 19 had lesions which originated from secondary causes while 2 had lesions which originated from primary pathologies (GVHD and Romberg scleroderma. The latter two cases have been included because they have been stable for more than three years. All patients underwent a reconstructive sequence consisting of one or two AFT interventions and then one HT. Table 4 provides a summary of the operations performed.
Table 4: Summary of the operations performed.
|
|
AGE SEX |
ETIOLOGY |
|
AFT |
|
HT -N° UF |
|
|
OP |
Micro |
Lips |
OP |
|
|||
|
1 |
36♀ |
TRAUMA |
PT |
1 |
1 |
PT |
1366 FUE |
|
2 |
|
BURN |
PT |
2 |
|
PT |
1427 FUE |
|
3 |
29♂ |
ACID BURN (BEARD AND EYEBROW) |
AI |
1 |
1 |
PT |
1816 FUE |
|
4 |
27♀ |
RADIOTHERAPY |
PT |
1 |
1 |
PT |
2660 STRIP |
|
5 |
46♂ |
NEGATIVE HAIR TRANPLANTATION OUTCOME |
PT |
2 |
|
PT |
1954 FUE |
|
6 |
53♂ |
ELECTROCUTION |
PT |
2 |
|
PT |
1560 FUE |
|
7 |
51♂ |
TRICHOTILLOMANIA (MOUSTACHE) |
AN |
2 |
|
PT |
320 FUE |
|
8 |
25♀ |
BIRTH SCAR |
PT |
1 |
|
PT |
1350 STRIP |
|
9 |
17♂ |
HIGH FLOWAVM EMBOLIZATION SEQUELAE |
LC |
1 |
1 |
PT |
875 FUE |
|
10 |
35♂ |
NEUROSURGICAL SCAR |
GG |
1 |
|
PT |
520 FUE |
|
11 |
16♂ |
FACIAL PARALYSIS SCAR |
GG |
1 |
1 |
PT |
641 FUE |
|
12 |
39♀ |
OTOPLASTY COMPRESSION |
AN |
1 |
|
PT |
183 FUE |
|
13 |
39♀ |
NEUROFIBROMATOSIS -VON RECKLINGHAUSEN |
LC |
1 |
2 |
PT |
2620 STRIP |
|
14 |
28♀ |
TRAUMA (EYEBROW) |
AN |
2 |
|
PT |
134 FUE |
|
15 |
71♂ |
ARTIFICIAL HAIR SCAR |
PT |
2 |
|
PT |
2159 FUE |
|
16 |
48♂ |
HAIR TRANSPLANT (CICATRICIAL OUTCOME) |
PT |
2 |
|
PT |
2127 FUE |
|
17 |
22♂ |
RADIOTHERAPY - ORBITAL RHABDOMYOSARCOMA |
LC |
2 |
|
PT |
453 FUE |
|
18 |
30♂ |
CLEFT LIP SEQUELAE |
LC |
|
2 |
PT |
197 FUE |
|
19 |
38♀ |
|
LP |
2 |
|
PT |
1400 FUE |
|
20 |
31♀ |
ROMBERG SY/LINEAR SCLERODERMA |
LC |
|
2 |
PT |
900 STRIP |
|
21 |
34♂ |
TRAUMA |
LC |
|
2 |
PT |
250 FUE |
PT: Piero Tesauro; LG: Luigi Clauser; AN: Andrea Nunziata; GG: Giulio Gherardini; AI: Alessandro Innocenti; LP: Luca Piovano.
Figure 1: Coverage value in donor and recipient area. Pre-transplantation (Numbers in Black) (10). Coverage value only in recipient area Post-transplantation (Numbers in Red). A CV equal to 30% less than the normal scar surrounding area provides a good coverage (7, 4).
I Autologous Fat Transfer (AFT)
Two different AFT techniques, Microfat and Lipostructure, have been performed. The choice falls on the preference of the surgeons and the need for a greater or lesser volumetric increase.
i Microfat
a Preparation
The microfat procedure is performed under local anaesthesia. The fat collection is made using 1mm diameter microperforated and microuncinate cannula with 0.8mm holes, significantly smaller than traditional ones (SEFFIHAIR® produced by SEFFILINE S.r.l. Bologna - Italy). The tunnelings are performed in the subcutaneous tissue adjacent to the dermis; this layer has been proven to hold more mesenchymal and vascular stem cells [8, 9]. Once the adipose tissue is harvested, it is transferred into 1ml luer lock syringes. The details of this technique are described in a previous article [10].
b Technical Notes
Under ring block anaesthesia of the receiving area, the suspension is injected using 21 or 23G needles into the subcutaneous layer at different levels. A fan pattern is followed using a retrograde injection technique to reduce thromboembolic risks. Some scarring lesions of the scalp have an extremely reduced thickness (1-2 mm) and in these cases, in order to overcome the limited thickness, we performed a preliminary infiltration of the receiving area with 1-2cc of PRP in order to expand the tissue promoting a multi-layer placement of the cellular fraction. The use of needles as an infiltration tool is necessary for two reasons. The first is to be referred to the frailty of some scar tissue, that is hard to penetrate with blunt micro-cannulas without running the risk of lacerations that could compromise the whole procedure. The second concerns the structural stiffness of some lesions, that may appear as a single block attached to the deep planes. In the latter, as other authors have highlighted, the cannula would not allow the positioning of the microfat in multiple layers [11].
ii Lipostructure
The lipostructure procedure is performed under local, local assisted or general anaesthesia using Dr. Coleman's technique [12, 13]. In the most penetrable tissues a cannula has been used for fat positioning, in other tissues needles have been used for the same reasons described above. AFT interventions have been spaced from a minimum of 3 months to a maximum of 10 months. The greater the amount of fat grafted, the longer the waiting time for a second session.
II Hair Transplantation (HT)
Both Strip and FUE HT techniques were used in the cases presented [14, 15]. The following are some technical peculiarities relevant to the procedures performed after the grafting of adipose fractions.
Technical Notes
HTs on previously grafted scarring lesions must consider four factors that differentiate them substantially from hair transplantations on healthy tissue.
1) The intense ischaemic response to vasoconstrictor use.
2) The lower graft retention by the tissue.
3) The greater frailty of the skin.
4) The greater vulnerability to infection.
i. Under normal circumstances, adipose tissue can withstand prolonged ischaemia, but recent experimental studies show that under stress conditions it is able to release inflammatory molecules [16]. At subsequent reperfusions, these can cause arteriolar vasoconstriction resulting in stagnation and blockage of capillary flow. These secondary phenomena can compromise the yield of the FU [17]. Hence the need not to use or severely restrict the use of vasoconstrictors in the receiving area by limiting them to peripheral use.
ii. AFT procedures can restore and regenerate the thickness and texture of the scar tissue by reducing the need to exaggerate the inclination of the follicles during positioning. The drawback is the reduction in the graft-retention-capacity of the tissue, due to the decreased number of elastic fibres. This can cause ‘popping’ during placement. The best prevention is to perform multiple preliminary tests to define the exact proportion between the incisions and the available grafts. For this purpose, it is important to have a wide range of blades or implanters of various sizes available. In addition, it is preferable to use the “stick and place” technique for the placement of ‘oversize’ grafts (single or wide three).
iii. The skin, while improving in quality with the adipose graft, loses stability due to a looser connection to the deep structures; the resulting abnormal mobility on the underlying planes may make it more prone to lacerations during the graft’s placement. The manoeuvre must be adapted accordingly. To improve the visibility of the operating field, multiple sprays of saline solution are preferable to gauze padding.
iv. The increased vulnerability to infection, due to the absence of skin appendages, requires the adoption of sterility measures for this operation that are usually not required in normal HT. All patients are required to start antibiotic therapy beforehand. A short video summary of the method described is available online (Link) [18].
Results
The results of the surgical plans carried out were documented photographically and dermatoscopically. In many cases a video recording was also performed to allow a better understanding of the density obtained in a dynamic situation. The photos and videos were submitted by the authors and two colleagues with experience in hair restoration surgery. The percentages of FU yield and their quality preservation appear comparable to that of procedures performed in healthy tissue. The results are considered very satisfactory and proportional to the FUs used. A high percentage of patients obtained a definitive result in a single session. The authors’ overall assessment is shown in (Table 5). The feedback from the patients was largely positive for everyone and for those who had already experienced challenging surgical experiences due to underlying pathologies. It should be mentioned that even in the case of electrocution, where a superficial infection occurred, the patient stated that they had very little discomfort and showed excellent compliance.
Table 5: The authors' overall assessment of the results of the operations in the 21 patients.
|
GRAFTS YIELD % |
QUALITY OF GRAFTS PRESERVATION |
GLOBAL RESULT |
SECOND HT NEEDS |
||||
|
80-100% |
15 |
80-100% |
16 |
EXCELLENT |
16 |
CERTAIN |
2 |
|
60-80%, |
5 |
60-80%, |
4 |
VERY GOOD |
4 |
PROBABLE |
3 |
|
40-60%. |
1 |
40-60%. |
1 |
GOOD |
1 |
UNCERTAIN |
1 |
|
20-40%. |
|
20-40%. |
|
FAIR |
|
UNPROBABLE |
5 |
|
0-20%, |
|
0-20%, |
|
POOR |
|
IMPOSSIBLE (almost) |
11 |
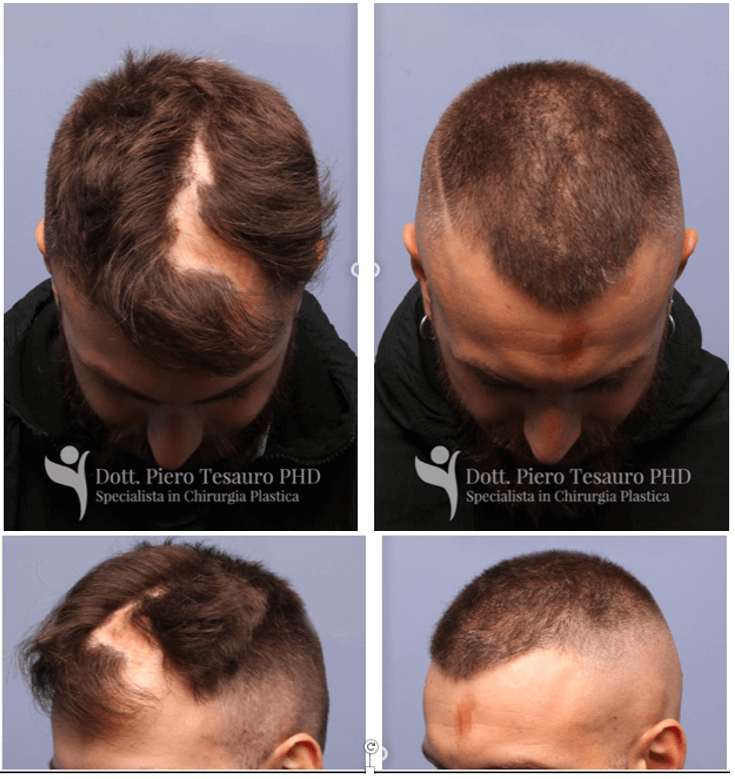
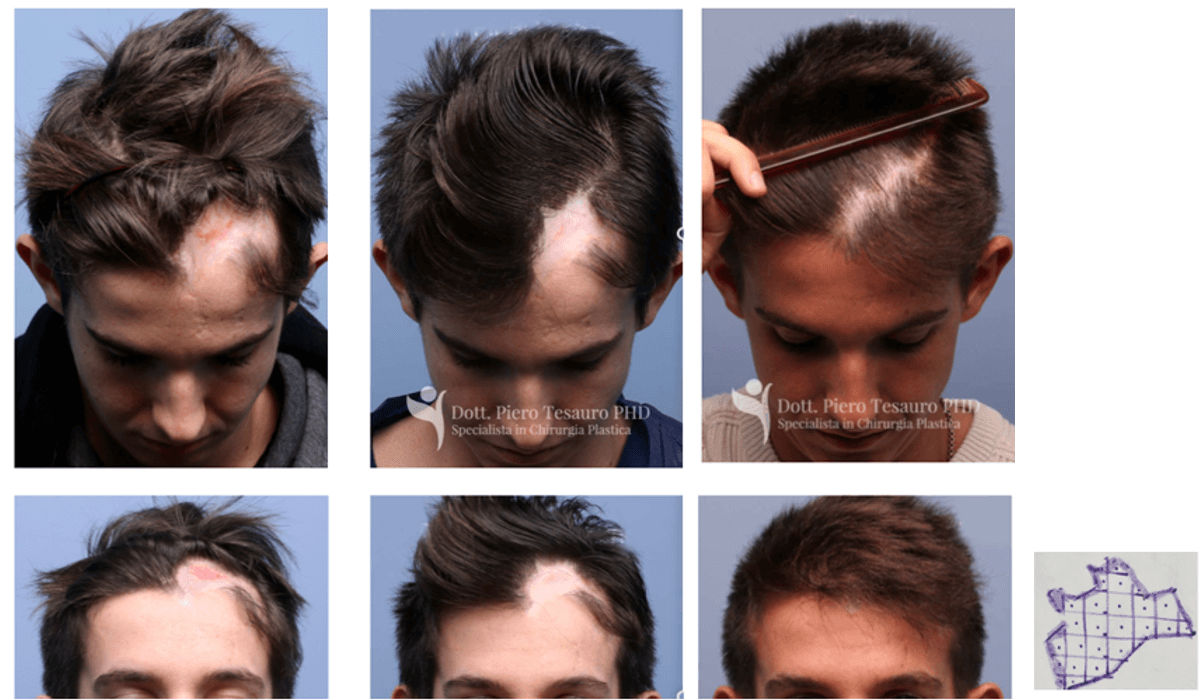
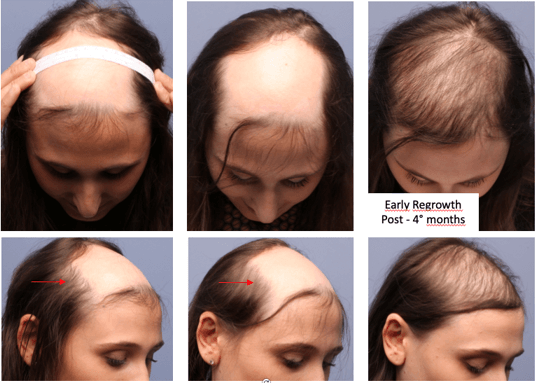
Three results are shown in (Figures 2-4). The most noticeable difference from the numerous cases of HT performed in the past years on scarring lesions was the constant and early hair regrowth that started between the second and third month after the transplant. It is unusual to observe the first results of the procedure after only four months (Figures 5 & 6). This phenomenon is to be considered in relation to a synergy of circumstances and positive actions and has often been the premise of excellent and stable results. The contrast with the past, characterized by interventions without preliminary regenerative operations, has represented for the authors a perfect litmus test based on which it is possible to state here that the benefits of these procedures are clear and evident.
Figure 2: Man, 31-year-old. Childhood scalp burn by hot water. Two AFT session respectively 10 and 14cc. Area size 30 cm2. Total Donor Capacity 11.000 FU, CV of the areas close to the scar = 10. FU Placed = 1427 UF Density 47 UF/ cm2. CV after transplant = 7,4. Before (left), 2 AFT and 9 months after a single FUE hair transplantation (right).
Figure 3: Boy, 16-year-old childhood-scalp scar related to high flow AVM embolization sequelae Two AFT session, respectively 15 and 20cc. Area size 23 cm2 (side photo). Total Donor Capacity 13.000 UF, CV Areas near the scar = 12. FU Placed = 875 UF, Density 38 UF/ cm2. CV after transplant = 6,5 (38 x 2,6 x 0.066). Before (left), After 2 session of AFT (center) After FUE (right).
Figure 4: Woman, 38-year-old. GWHD (Grafts Versus Host Disease), New onset lichenoid alopecia Two AFT session respectively 20 and 20cc. Area size 30 cm2. Total Donor Capacity 6.000 FU, CV of the areas close to the scar = 10. Placed = 1400 UF, Density 45 UF/cm2. CV after transplant = 7,2 (45 x 2,5 x 0, 064). Before (left), 12 months after 2 session of AFT and FUE hair transplantation (right).
Figure 5: Woman, 27-year-old, Scalp scar related to radiotherapy for osteoid osteomas bone metastases. Two AFT session respectively 15 and 22cc. Area size 75 cm2. Total Donor Capacity 13.000 UF, Placed = 2660 UF. Density 35 UF/cm2. CV after transplant (24 x 2,73 x 0.066) = 4,32. Red arrow indicates the quality improvement of the hairs at the border of the lesion. This early and homogenous regrowth is a common feature of the vast majorities of our cases. Before (left), After 2 session AFT (center) 4 months after strip hair transplantation (right).
Figure 6: Woman, 36-year-old. Trauma caused by car accidents. Two AFT session respectively 10 and 14cc. Area size 26 cm2. Total Donor Capacity 12.000 UF, CV Areas near the scar 10. Placed = 1366 UF, Density 47 UF/cm2. CV after transplant = 6,84 (48 x 2,5 x 0,057). Before (left), 4 months after 2 session AFT and FUE hair transplantation (right). A) Pre-AFT. B) Evidence of improvement after AFT only.
Discussion
Recent technical improvements, inherent to HT’s two main procedures, have mainly focused on a myriad of changes aimed at perfecting a "secure transfer" of FUs from the donor site to the recipient site. The new procedures have reduced all kind of damages to the grafts during both the harvesting and the placement phases. Moreover, improved storage solutions improved their homeostasis during the ischaemia-reperfusion period. These changes have had a significant impact on the quality and reliability of the results and have undoubtedly contributed to the explosive demand for HT in the aesthetic field. Minor attention has been given to the receiving area. Mesotherapy, PRP and regenerative medicine (ADSCs) have been used in a very diversified way and mainly to consolidate the results of medical therapy and to stabilize the results after HT. This retrospective study comes from the observation of increasing clinical evidence of complete and early regrowth of follicular units after HT in AFT pre-treated scarring areas. The selection process when approaching patients for this scientific work, was based solely on a well-structured clinical evaluation. There is, therefore, a lack of instrumental evaluation of results in quantitative (counting) and qualitative (hair thickness) terms. The authors reserve the right to investigate these aspects further in a future study. These evaluations are based on the authors’ expert clinical judgement, dermatoscopy and global video photography data.
Why replace a single operation with a multi-step sequence? Which considerations about past experiences have led to this point? We know that several types of resident cells are needed for a tissue to be functional, able to maintain homeostasis and to perform its regenerative functions. So far enriching an impoverished tissue seems intuitively an advantage, but this has proven to be not enough. Equally, it could be said that hair transplantation was already an ideal tool for this purpose. [19, 20]. The hair follicle already enriched the tissues with all its components and one single HT could achieve the same goal. In fact, the positive effects of HTs alone in cicatricial alopecia has been known for years and both HT (strip and FUE) have been widely use. Strip technique was predominantly used for these cases until 2015, giving also the option of maintaining a habitual hair style [21]. Moreover, grafts derived from a Strip preserved a greater amount of adipose perifollicular tissue, they were less skeletonized, offering the chance to implant a true composite graft.
It was clear that FUs richer in adipose tissue required more nourishment to ensure their survival particularly in damaged scar tissue. These limitations ended in a tendency to perform conservative transplants at low density. In order to be more predictable. the reconstructive path was frequently divided into several steps of HT’s. Beyond the common sense that derives from experience, the surgeon had no tools to determine the right number of grafts to use in a previously compromise area. The unsatisfactory yield of the FUs would have led to a frustrating result, worsening the clinical picture due to a significant waste of hair follicles. Given that the FU availability is not only exhaustible but often limited. In this context, patients were frequently disappointed with the partial results, many of which could have led them to abandon the reconstructive path. The refinement of the FUE technique has offered many new options. Among them is worth mentioning the PAHT (peripheral areas HT), a recent proposal by Dr. Sebastián Yriart to extend the harvesting area to the regions surrounding the scar considering the AGA evolution scenario [22]. Even considering all these new strategies, the necessity to improve the trophism of the receiving tissue prior to perform HT to overcome the reliability of the results remains the same [23].
The reasons for the need to change course are resumable in two main points:
i. Improve the reproducibility and consistency of results.
ii. Significantly reducing the risks of the procedures and improving their course of action.
Significant advantages have been obtained when comparing this approach to interventions carried out "tout court" and not combined with preliminary steps. A previous treatment of the scar tissue means that it can be transplanted with greater density and reduces need for multiple sessions of HT. Not only this procedure plans accelerate the achievement of the final result, but frequently a satisfactory result for the patient can be seen from the first HT and reduces the risks of unsuccessful operation.
The surgeon’s work is more predictable and more options to create this “safe starting point”, prior to an HT are available:
1) Amount of fat to be transplanted.
2) Numbers of sessions.
3) Time-intervals between each session.
4) Standardized protocol to harvest and manipulate the micro fragmented adipose tissue.
i. The amount of AFT used in each single treatment can be proportional to the characteristics of the area to be treated and it can be progressively increased.
ii. The number of sessions, in our clinical experience, is limited to two but can be adapted to each case.
iii. Intervals between session must be chosen to maximize the final result.
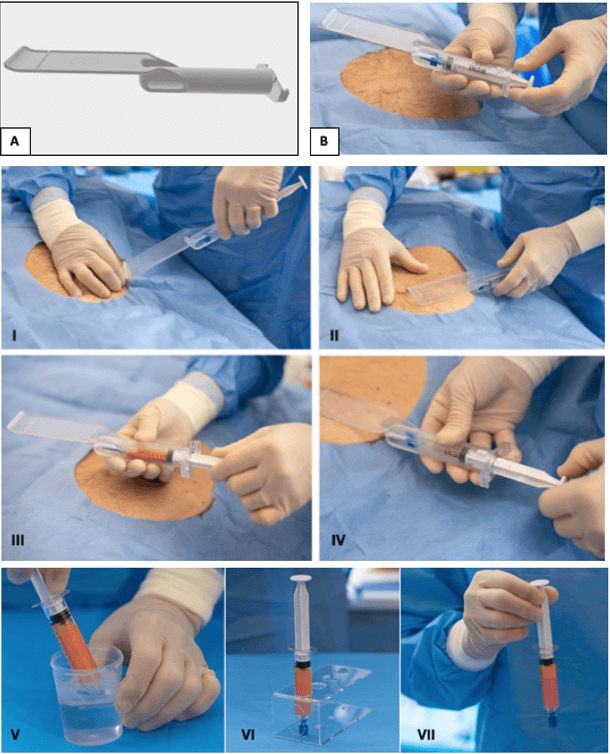
iv. In 50% of the cases presented, the preparation of the autologous fat was carried out using a single standardised protocol (SEFFI). This system, created with the purpose of being used in a similar way by surgeons with different backgrounds and skills, always offers the advantage of performing the harvesting with the same instrumentation and guidance. The adipose tissue fragments are aspirated from the same subcutaneous layer and do not require any substantial manipulation prior to grafting (Figure 7). This has created a standard that allows for a better results comparison and which we intend to investigate further in the future.
The Procedure Manual aspiration/selection of the adipose tissue. (I) Cannula introduction perpendicular to the skin through a hole in the skin performed with a 18G needle; (II) Rotation of the guide 90 degree and introduction of the cannula in the superficial subcutaneous plan; (III) lock the plunger in aspiration position and move back and forth to select the adipose tissue clusters; (IV) micro fragmented adipose tissue in the syringe. (V) After aspiration, the fat was mixed with cold Ringer’s solution to rinse it from the anaesthetic to facilitate tissue precipitation (VI, VII).
Figure 7: The Device A) The special guide allows to select the adipose tissue in the superficial and standardized plan even if the physician has not specific liposuction skills. B) The guide assembled with syringe and cannula.
A further advantage is the long-term durability of the HT. This factor, frequently underestimated, is of crucial importance. This study has in fact shown how this technique promotes a longer and increasingly stable lifespan of the FUs in HT’s. The immunomodulatory action provided by ADSCs and SVF fragments could allow a greater predictability of long-term results also of HTs in primary scarring lesions (Lichen, AFF, etc.) that today are strongly conditioned by recrudescence of the same pathology. The two cases included in this study have been monitored for more than three years and present a stable clinical picture.
Despite all these considerations, a reflection to be considered in the therapeutic proposal, as far as the density to be achieved is concerned, comes from the analysis of cases of women who have developed chemotherapy-induced alopecia (CIA). A picture of widespread alopecia that is not very responsive to treatment and that leads to a thinning of various degrees. These data provide precise elements to decide whether to operate or not by suggesting alternative techniques to patients with particular reference to prosthetic ones. For many of these patients, the density of a prosthetic is necessary to restore a satisfactory image. This experience leads us today to judge with greater criticality surgical results amongst females with previous scarring alopecia, whose expectations on density are measured on a different scale when compared to male patients. Managing expectations has to be part of a comprehensive patient discussion that needs to be crystal clear prior to approaching a surgical path, which can often only reach a partially satisfactory result.
Conclusion
This work further widens the field of application of the AFT which, like it already happened in maxillo-facial, plastic and cosmetic surgery, proves to be successful to transform complex procedures, associated with higher risks, into simpler procedures [24-27]. It aimed to explore how tissue regeneration through AFT can significantly improve hair growth in the area of scarring alopecia, underlining, once again, the tremendous potential of this approach. Since surgeons have been debating the causes responsible for reduced yield or loss of results in the long term, this article opens two big questions:
1) Will combining the preliminary clinical evaluation with instrumental evaluation redefine the concept of eligibility of a scar tissue to HT?
2) Will it be useful to extend the benefits of this method from scarring cases to those with only aesthetic purposes that, especially having already undergone a previous HT, are not free of these problems?
New strategies are being studied today to improve the results and survival of fat grafting. We believe that HTs and their results, easy to judge by their clinical evidence, could be a useful tool in the future to evaluate the real effectiveness of these improvements in clinical practice. This year we celebrate 500 years since Raphael's death, Italian renaissance painter and architect, who inspired the metaphor which we would like to conclude this article. The genius looking at a rough block of marble perceives the presence of a wonderful shape inside it. The disciple is the one who investigates what wonderful ‘instruments’ act silently in his master's mind. In this article the ‘instruments’ are represented by a series of preliminary actions; meetings between specialists, measurements, calculations and, only when possible, with operations capable of restoring the beauty in a wounded person's life.
Acknowledgements
Some of the cases of this work relied on the work of other colleagues. Their contribution was invaluable: Thanks a lot to Dr Andrea Nunziata, Dr. Alessandro Innocenti, Dr. Giulio Gherardini, Dr. Luca Piovano, Dr. Massimo Gabellini and Dr. Niccolò Rivetti. The authors would also like to thank Fabiana Tesauro for her valuable contribution to the English translation of the article.
Author Contributions
Piero Tesauro, Luigi Clauser: The authors made a substantial contribution in the surgical work and to conception and design of the article. Angelo Trivisonno, Alessandro Gennai, Andrea Marliani: The authors contributed to conception and design of the study to the article with numerous insight and suggestions.
Availability of Data and Materials
Not Applicable.
Funding
None.
Conflicts of Interest
None.
Ethical Approval and Consent to Participate
Not applicable.
Consent for Publication
A written informed consent for publication was obtained.
Article Info
Article Type
Original ArticlePublication history
Received: Tue 07, Jul 2020Accepted: Fri 17, Jul 2020
Published: Sat 25, Jul 2020
Copyright
© 2023 Piero Tesauro. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RGM.2020.02.06
Author Info
Piero Tesauro Angelo Trivisonno Alessandro Gennai Andrea Marliani Luigi Clauser
Corresponding Author
Piero TesauroPlastic Surgeon, Private Practice, Milano, Italy
Figures & Tables
Table 1: Range of specialists who may be consulted for cicatricial alopecia.
|
DOCTORS |
NON-MEDICAL DOCTORS |
||
|
Maxillo Facial Surgeons |
Plastic Surgeons |
Aesthetics Surgeons |
Wigs / Prosthetics |
|
Neurosurgeon |
Radio Therapist |
Dermatologist |
SMP Specialist |
Table 2: Data from Practice census survey ISHRS-2018.
|
ORIGINAL MEDICAL SPECIALTY OF HAIR TRANSPLANT SURGEONS |
% |
|
Plastic Surgery |
19,1 |
|
Cosmetic Surgery |
12,1 |
|
Maxillo-Facial Surgery |
2,7 |
|
OTHER |
66,1 |
|
Practice Census Survey ISHRS - 2018 |
|
Table 3: Coverage value formula.
|
$$CV=\frac{FU}{{cm}^2}x\frac{Hair}{FU}x\ Caliber$$ |
|
Cleaning the formula .. |
|
$$CV={cm}^2x\ Hair\ x\ Caliber$$ |
|
COVERAGE VALUE FORMULA |
Table 4: Summary of the operations performed.
|
|
AGE SEX |
ETIOLOGY |
|
AFT |
|
HT -N° UF |
|
|
OP |
Micro |
Lips |
OP |
|
|||
|
1 |
36♀ |
TRAUMA |
PT |
1 |
1 |
PT |
1366 FUE |
|
2 |
|
BURN |
PT |
2 |
|
PT |
1427 FUE |
|
3 |
29♂ |
ACID BURN (BEARD AND EYEBROW) |
AI |
1 |
1 |
PT |
1816 FUE |
|
4 |
27♀ |
RADIOTHERAPY |
PT |
1 |
1 |
PT |
2660 STRIP |
|
5 |
46♂ |
NEGATIVE HAIR TRANPLANTATION OUTCOME |
PT |
2 |
|
PT |
1954 FUE |
|
6 |
53♂ |
ELECTROCUTION |
PT |
2 |
|
PT |
1560 FUE |
|
7 |
51♂ |
TRICHOTILLOMANIA (MOUSTACHE) |
AN |
2 |
|
PT |
320 FUE |
|
8 |
25♀ |
BIRTH SCAR |
PT |
1 |
|
PT |
1350 STRIP |
|
9 |
17♂ |
HIGH FLOWAVM EMBOLIZATION SEQUELAE |
LC |
1 |
1 |
PT |
875 FUE |
|
10 |
35♂ |
NEUROSURGICAL SCAR |
GG |
1 |
|
PT |
520 FUE |
|
11 |
16♂ |
FACIAL PARALYSIS SCAR |
GG |
1 |
1 |
PT |
641 FUE |
|
12 |
39♀ |
OTOPLASTY COMPRESSION |
AN |
1 |
|
PT |
183 FUE |
|
13 |
39♀ |
NEUROFIBROMATOSIS -VON RECKLINGHAUSEN |
LC |
1 |
2 |
PT |
2620 STRIP |
|
14 |
28♀ |
TRAUMA (EYEBROW) |
AN |
2 |
|
PT |
134 FUE |
|
15 |
71♂ |
ARTIFICIAL HAIR SCAR |
PT |
2 |
|
PT |
2159 FUE |
|
16 |
48♂ |
HAIR TRANSPLANT (CICATRICIAL OUTCOME) |
PT |
2 |
|
PT |
2127 FUE |
|
17 |
22♂ |
RADIOTHERAPY - ORBITAL RHABDOMYOSARCOMA |
LC |
2 |
|
PT |
453 FUE |
|
18 |
30♂ |
CLEFT LIP SEQUELAE |
LC |
|
2 |
PT |
197 FUE |
|
19 |
38♀ |
|
LP |
2 |
|
PT |
1400 FUE |
|
20 |
31♀ |
ROMBERG SY/LINEAR SCLERODERMA |
LC |
|
2 |
PT |
900 STRIP |
|
21 |
34♂ |
TRAUMA |
LC |
|
2 |
PT |
250 FUE |
PT: Piero Tesauro; LG: Luigi Clauser; AN: Andrea Nunziata; GG: Giulio Gherardini; AI: Alessandro Innocenti; LP: Luca Piovano.
Table 5: The authors' overall assessment of the results of the operations in the 21 patients.
|
GRAFTS YIELD % |
QUALITY OF GRAFTS PRESERVATION |
GLOBAL RESULT |
SECOND HT NEEDS |
||||
|
80-100% |
15 |
80-100% |
16 |
EXCELLENT |
16 |
CERTAIN |
2 |
|
60-80%, |
5 |
60-80%, |
4 |
VERY GOOD |
4 |
PROBABLE |
3 |
|
40-60%. |
1 |
40-60%. |
1 |
GOOD |
1 |
UNCERTAIN |
1 |
|
20-40%. |
|
20-40%. |
|
FAIR |
|
UNPROBABLE |
5 |
|
0-20%, |
|
0-20%, |
|
POOR |
|
IMPOSSIBLE (almost) |
11 |


References
- Epstein JS (2006) Scalp Reconstruction: The Role of Tissue Expansion. Hair Transplant Forum Int 16: 171-172.
- International Society of Hair Restoration Surgery (2017) Practice Census Results.
- Rachael Kay, Ball EAM, Williams G, D’Souza CM (2018) Review of the 26th World Congress of the ISHRS Hollywood, California October 10-14, 2018. Hair Transplant Forum Int 28: 239-243.
- Akdag O, Evin N, Karamese M, Tosun Z (2018) Camouflaging Cleft Lip Scar Using Follicular Unit Extraction Hair Transplantation Combined With Autologous Fat Grafting. Plast Reconstr Surg 141: 148-151. [Crossref]
- Lorenzo J https://www.youtube.com/watch?v=k2HX2eHmSIc.
- Erdogan K (2020) Session 18, from 6to Workshop Latino Americano de FUE- Mexico. Cancun Mexico.
- Piamphongsant P, Pathomvanich D, Piyadumrongkit P, Sriphojanart T (2019) Rapid and Accurate Digital Measurement of the Recipient Area in Hair Transplantation Using a Tablet Application. Hair Transplant Forum Int 29: 228-230.
- Clauser L, Lucchi A, Tocco Trussardi I, Gardin C, Zavan B (2018) Autologous fat transfer for facial augmentation and regeneration: Role of mesenchymal stem cells. Atlas Oral Maxillofac Surg Clin North Am 26: 25-32. [Crossref]
- Trivisonno A, Di Rocco G, Cannistra C, Finocchi V, Farr ST et al. (2014) Harvest of superficial layers of fat with a microcannula and isolation of adipose tissue-derived stromal and vascular cells. Aesthet Surg J 34: 601-613. [Crossref]
- Gennai A, Zambelli A, Repaci E, Quarto R, Baldelli I et al. (2017) Skin Rejuvenation and Volume Enhancement with the Micro Superficial Enhanced Fluid Fat Injection (M-SEFFI) for Skin Aging of the Periocular and Perioral Regions. Aesthet Surg J 37: 14-23. [Crossref]
- Zeltzer AA, Tonnard PL, Verpaele AM (2012) Sharp-needle intradermal fat grafting (SNIF). Aesthet Surg J 32: 554-561. [Crossref]
- Coleman SR, Katzel EB (2015) Fat Grafting for Facial Filling and Regeneration. Clin Plast Surg 42: 289-300. [Crossref]
- Clauser L, Zavan B, Galiè M, Vittorio LD, Gardin C et al. (2019) Autologous fat transfer for facial augmentation: surgery and regeneration. J Craniofac Surg 30: 682-685. [Crossref]
- Farjo B, Farjo N, Williams G (2015) Hair transplantation in burn scar alopecia. Scars Burn Heal 1: 2059513115607764. [Crossref]
- Yoo H, Moh J, Park J (2019) Treatment of Postsurgical Scalp Scar Deformity Using Follicular Unit Hair Transplantation. Biomed Res Int 2019: 3423657. [Crossref]
- Gust MJ, Hong SJ, Fang RC, Lanier ST, Buck DW et al. (2017) Adipose Tissue Drives Response to Ischemia-Reperfusion Injury in a Murine Pressure Sore Model. Plast Reconstr Surg 139: 1128e-1138e. [Crossref]
- Wang WZ, Baynosa RC, Zamboni WA (2011) Update on ischemia reperfusion injury for the plastic surgeon: 2011. Plast Reconstr Surg 128: 685e-692e. [Crossref]
- Tesauro P https://www.youtube.com/watch?v=xOtHT0Tdwxs&feature=emb_logo
- Barrera A (2001) The Use of Micrografts and Minigrafts for the Treatment of Burn Alopecia. Hair Transplant Forum Int 11: 43-44.
- Shao H, Hang H, Yunyun J, Hongfei J, Chunmao H et al. (2014) Follicular unit transplantation for the treatment of secondary cicatricial alopecia. Plastic Surg (Oakville) 22: 249-253. [Crossref]
- Devroye J (2016) Powered FU Extraction with the Short-Arc-Oscillation Flat Punch FUE System (SFFS). Hair Transplant Forum Int 26: 129-136.
- Yriart S (2020) Hair Transplant in Reconstructive Surgery (PAHT), Session 18 from 6to Workshop Latino Americano de FUE. Cancun Mexico.
- Kuka G, Epstein J, Aronowitz J, Glasgold MJ, Rogal JG et al. (2020) Cell Enriched Autologous Fat Grafts to Follicular Niche Improves Hair Regrowth in Early Androgenetic Alopecia. Aesthetic Surg J 40: NP328-NP339. [Crossref]
- Clauser L, Consorti G, Elia G, Galié M, Tieghi R (2014) Three-dimensional volumetric restoration by structural fat grafting. Craniomaxillofac Trauma Reconstr 7: 63-70. [Crossref]
- Denadai R, Raposo Amaral CA, Raposo Amaral CE (2019) Fat grafting in managing craniofacial deformities. Plast Reconstr Surg 143: 1447-1455. [Crossref]
- Rigotti G, Marchi A, Galie M, Baroni G, Benati D et al. (2007) Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 119: 1409-1422. [Crossref]
- Egro FM, Coleman SR (2020) Facial Fat Grafting: The Past, Present, and Future. Clin Plast Surg 47: 1-6. [Crossref]
