Gallbladder Mass and Diffuse Wall Thickness in an Elderly Patient: is it Definitively a Gallbladder Cancer?
Gallbladder Mass and Diffuse Wall Thickness in an Elderly Patient: is it Definitively a Gallbladder Cancer?
A B S T R A C T
Gallbladder masses as part of gallbladder pathology are commonly encountered at clinical scenario. However, it is important to distinguish between benign and malignant conditions in terms of clinical significance and management. While few gallbladder masses may present with unusual or nonspecific imaging appearances that is not easy to characterize gallbladder pathology. This report herein showed an elderly patient with a gallbladder mass accompanied by diffuse wall thickness of gallbladder that were similar to clinical characteristic of gallbladder cancer. Under thoughtfully surgical management, this patient was recovery very well from the operation and end up with a pleasant result of chronic cholecystitis instead of gallbladder carcinoma. Therefore, patients with a gallbladder mass are not definitively related to malignancy but should also be kept in mind the possibility of carcinoma. As long as pathological diagnosis is confirmed, surgical management with a therapeutic intent based on suitable clinical circumstances should be attempted.
Keywords
Gallbladder mass, gallbladder cancer, cholecystitis, operation
Introduction
Gallbladder mass is commonly encountered at clinical scenario. However, distinguishing between benign and malignant entity is critical especially in an elderly patient. Although most gallbladder masses could be benign, they may present with unusual or nonspecific imaging appearance that is unable to differential diagnosis with gallbladder carcinoma [1]. As such, gallbladder carcinoma remains a common malignancy of the biliary tract with dismal prognosis [2]. Patients with a gallbladder mass are not definitively related to malignancy but should also be kept in mind the possibility of carcinoma. This report herein presented an elderly patient with a gallbladder mass accompanied by diffuse wall thickness of gallbladder that were similar to clinical characteristic of gallbladder cancer.
Patient information
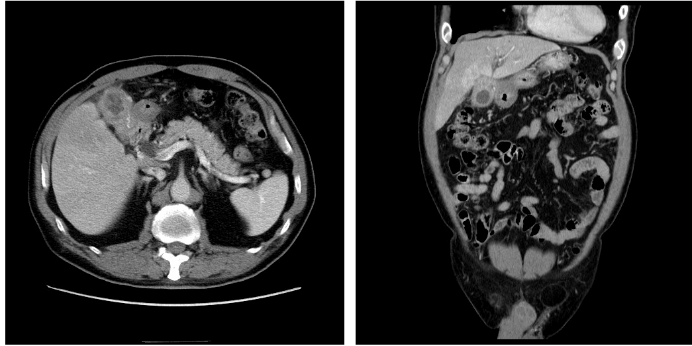
A 73-year-old man presented with intermittent post prandial nausea and abdominal fullness for 6 months. It was accompanied by decreased appetite and weight loss of 3 kg since the onset of symptoms. During this period, he had no abdominal pain associated with fever. His medical history included hypertension that was well-controlled by medication, with no previous surgical history. Physical examination found a vague palpable mass with mild local tenderness in the right upper quadrant of the abdomen. Ultrasonographic examination revealed a gallbladder mass and laboratory testing of blood samples, liver function tests, and tests for alpha fetoprotein (7.7 ng/mL), carcinoembryonic antigen (<0.5 ng/mL), and carbohydrate antigen 19-9 (9.52 ng/mL) were all within the reference ranges. Abdominal contrast-enhanced computed tomography (CT) showed a gallbladder mass with diffuse wall thickening, hyperemic change of adjacent liver tissue, and adhesions to gastric antrum and duodenal bulb. (Figure 1). Additionally, magnetic resonance cholangiopancreatography (MRCP) showed similar finding to the CT results, and mild dilatation of the biliary tree with a 1.1-cm common bile duct stone and an enlarged choledocal lymphadenopathy were also noted (Figure 2).
Figure 1: Contrast-enhanced computed tomographic imaging shows irregular wall thickening of the gallbladder with involvement of gastric antrum and hyperemic change of adjacent liver tissue.
Figure 2: Magnetic resonance cholangiopancreatography shows irregular gallbladder wall thickening with narrowing at the neck of the gallbladder and dilated biliary tree with a stone in the common bile duct. Suspicious lymphadenopathy near the gallbladder neck is also noted.
Therapeutic Intervention
Under the suspicion of a malignant tumor arising from the gallbladder with local lymph node spreading and possible duodenal bulb involvement, surgical resection including radical cholecystectomy and pancreaticoduodenectomy with curative intent was planned. Intraoperatively, an induration mass at the neck of the gallbladder associated with diffuse thickness of the gallbladder wall was noted, and the mass tightly adhered with the gastric antrum and duodenal bulb that remained separable from the gallbladder mass. Additionally, induration change of liver parenchyma near the gallbladder was also noted. Cholecystectomy was first performed for frozen section examination, and the results revealed no evidence of malignancy. Subsequently, partial hepatectomy of the gallbladder liver bed and removal of the local choledochal lymph node plus choledocholithotomy and T-tube drainage were performed. The pathological examination of surgical specimens showed marked chronic inflammation, erosion, ulceration and fibrosis in the gallbladder, and foamy cell infiltration, mild ductile proliferation, with chronic inflammation in the resected liver tissue, and focal necrotizing granulomatous inflammation in the excised lymph node, which confirmed chronic cholecystitis.
Discussion
Chronic cholecystitis is commonly associated with cholelithiasis, and its clinical presentation could vary from biliary colic to non-specific vague abdominal fullness [3, 4]. Although the ultrasound examination might be a simple tool to quickly assess cholelithiasis as well as cholecystitis, presentation of chronic cholecystitis could be diverse, especially in complicated cases. Moreover, CT could provide information on anatomy, regional lymphadenopathy, and extrahepatic disease if malignancy is suspected, and could further display details of the biliary tract and vasculature. However, the gallbladder may be enlarged or shrunken due to fibrosis, with various degrees of wall thickening and irregularity that mimic cancer in radiological imaging examination, leading to a difficulty in the differential diagnosis of chronic cholecystitis from malignancy.
Although rare, gallbladder carcinoma remains a common malignancy of the biliary tract with dismal prognosis [2]. Clinically, gallbladder carcinoma can show symptoms and imaging findings resembling cholecystitis. Additionally, gallbladder carcinoma is possibly associated with cholecystitis specifically in elderly patients [5, 6]. A gallbladder that is suspicious for malignancy requires meticulous workup, but the necessity of a pre-operative biopsy remains controversial due to concerns related to a risk of the tumor seeding to peritoneum and biopsy tracts. Nonetheless, intraoperative frozen section is usually recommended for highly suspicious cases to confirm malignancy. As such, surgical resection with curative intent remains the most effective treatment for patients with gallbladder carcinoma if malignancy is confirmed [7, 8]. In summary, patients with a gallbladder mass are not definitively related to malignancy but should also be kept in mind the possibility of carcinoma. Although the preoperative biopsy remains debatable, intra-operative frozen section is mandatory to exclude malignancy. As long as malignancy is confirmed, surgical resection with a curative intent based on suitable clinical staging could be the best treatment available for patients with gallbladder carcinoma. In contrast, surgical management in terms of relieving clinical symptoms is adequate for inflammatory cholecystitis.
Conflicts of Interest
All authors have no conflict of interest.
Article Info
Article Type
Case ReportPublication history
Received: Mon 27, May 2019Accepted: Tue 20, Aug 2019
Published: Fri 30, Aug 2019
Copyright
© 2023 Kun-Ming Chan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.01.04
Author Info
Corresponding Author
Kun-Ming ChanDepartment of General Surgery & Department of Organs Transplantation Institute, Chang Gung Memorial Hospital at Linkou, Chang Gung University College of Medicine, Taoyuan, Taiwan
Figures & Tables

References
- Levy AD, Murakata LA, Abbott RM, Rohrmann CA Jr (2002) From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics 22: 387-413. [Crossref]
- Chan KM, Yeh TS, Yu MC, Jan YY, Hwang TL et al. (2005) Gallbladder carcinoma with biliary invasion: clinical analysis of the differences from nonbiliary invasion. World J Surg 29: 72-75. [Crossref]
- Bedirli A, Sozuer EM, Yuksel O, Yilmaz Z (2001) Laparoscopic cholecystectomy for symptomatic gallstones in diabetic patients. J Laparoendosc Adv Surg Tech A 11: 281-284. [Crossref]
- Diehl AK (1992) Symptoms of gallstone disease. Baillieres Clin Gastroenterol 6: 635-657. [Crossref]
- Chao TC, Jeng LB, Jan YY, Hwang TL, Wang CS et al. (1998) Concurrent primary carcinoma of the gallbladder and acute cholecystitis. Hepatogastroenterology 45: 921-926. [Crossref]
- Liu KJ, Richter HM, Cho MJ, Jarad J, Nadimpalli V et al. (1997) Carcinoma involving the gallbladder in elderly patients presenting with acute cholecystitis. Surgery 122: 748-754. [Crossref]
- Andren-Sandberg A, Deng Y (2014) Aspects on gallbladder cancer in 2014. Curr Opin Gastroenterol 30: 326-331. [Crossref]
- Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I et al. (2015) Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg 261: 733-739. [Crossref]
