Feasibility and Safety of a Novel Distal Radial Artery Approach for Arterial Blood Gas in COVID-19 Patients
A B S T R A C T
Background: Hypoxemia has been reported in association with the recent COVID-19 pandemic requiring serial arterial blood gas sampling in infected patients. Radial puncture remains the technique of choice for arterial blood sampling but present limitations and complications.
Aims: We presents the safety and feasibility of distal radial artery puncture in COVID-19 patients requiring arterial blood sampling.
Methods: Twenty COVID-19 patients requiring arterial blood sampling were prospectively enrolled in the emergency room upon presentation.
Results: All patients were successfully punctured with no reported complications.
Conclusion: Distal radial artery puncture for arterial blood sampling is safe and feasible in COVID-19 patients.
Keywords
Distal radial artery, arterial blood gases, radial artery puncture, COVID-19
Introduction
The coronavirus disease (COVID-19) pandemic is straining the medical sectors and economic resources worldwide. Recent statistics indicate a high second wave severe-case rate, among which a staggering mortality rate has been reported [1]. Hypoxemia has been independently associated with in-hospital mortality [2]. Hypoxemia is best assessed using arterial blood gas (ABGs) sampling and patients with moderate or severe symptoms need regular ABGs [3]. Radial artery puncture remains the method of choice for arterial blood sampling achieving high success rate. This technique is a skill easily mastered by physicians [4]. Although considered a safe procedure, complications may occur during radial artery puncture with a reported rate limited to < 5% [5-7]. The most common complications include temporary arterial occlusion, permanent ischaemia, local infection, bleeding, or hematoma formation with reported mean incidence rates of 19.7%, 0.09%, 0.72%, 0.53% and 14.4%, respectively [7]. Less severe but still common complications include vasospasm, hemorrhage, and pain. With a reported incidence of 0.09%, radial artery pseudoaneurysm is a rare but serious complication of arterial puncture presenting a risk of infection and rupture [6, 7].
Radial artery puncture is relatively contraindicated in multiple clinical scenarios: occlusion of the ulnar artery (a modified Allen test can be performed to assess the adequacy of the collateral circulation of the radial artery by the ulnar artery), in patients under anticoagulants or with coagulopathies (increased risk of bleeding and hematoma formation) and patients with an overlying skin infection [3]. The most common technical difficulties associated with radial artery puncture for arterial blood sampling are vasospasm, weak pulsation of the artery and venous instead of arterial blood sampling. Hospitalized patients with moderate to severe COVID-19 symptoms need constant monitoring of ABGs providing insights on acid-base balance. The repeated test and punctures of radial vascular structures could lead to severe trauma and consequently, a higher risk of occlusion.
A new possible alternative could be a puncture of the distal radial artery which could potentially decrease the risk of vascular complication significantly and allow a faster and easier blood sampling. The distal radial artery can be punctured at two sites where the radial pulse can be found: the anatomic snuffbox and the first intermetacarpal space. The anatomical snuffbox is defined as a triangular depression on the dorsum of the hand bordered laterally by the extensor pollicis brevis tendon and the extensor pollicis longus tendon medially with the floor formed by the trapezium carpal bones. As the radial artery has reached the anatomic snuffbox, it has already given rise to some branches that, in case of vessel occlusion, could avoid flow interruption, ischaemia of the hand and occlusion of the radial artery [8].
Methods and Materials
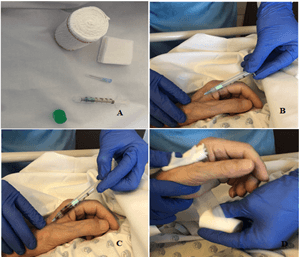
We prospectively included 20 consecutive COVID-19 patients hospitalized and requiring ABGs analysis. The procedure was performed through a distal radial artery puncture for all patients by a trained physician who has previous experience in distal radial artery puncture. We used readily available standard material for sampling ABGs that contain a small 23-Gauge needle, a standard syringe cap containing dry lithium heparin or sodium heparin, alcohol swabs, gauze, tape, nonsterile gloves, and a nonsterile gown (Figure 1A).
Figure 1: A) Used material for arterial blood gases analysis. B) Distal radial arterial puncture. C) 2-cc arterial blood sampling. D) Compressive dressing.
After careful distal radial artery pulse palpation with the patient being in a comfortable position, 1% lidocaine without epinephrine was drawn up in a 5-cc syringe and administered subcutaneously through a small 25-Gauge needle for local anaesthesia followed by a skin puncture at a 30° angle (Figure 1B). The needle was then advanced slowly, being oriented towards the proximal radial artery and towards the index over the maximal arterial pulsation area. A deep puncture was avoided as contact with the periosteum can be painful. At least 2-cc of bright red, pulsating blood were passively drawn (Figure 1C). If no blood was retrieved, the needle was slowly withdrawn and a new attempt was made. After blood sample collection and syringe withdrawal, pressure was applied to the site with sterile gauze and compression of about 10 min, after which a small compressive dressing was left in place over the punctured site (Figure 1D).
Results
Twenty patients were included in the study. Clinical and procedural characteristics are shown in (Table 1). Mean patients’ age was 66.2 ± 11.8 years and 80% (n=16) were males. Sixteen patients (80%) were hypertensive and 2 (10%) were on oral anticoagulation. An unsuccessful sampling was reported in 3 patients (15%), where a second puncture reattempt was undergone. All patients (100%) had a successful distal radial artery puncture. The intensity of the pulsation was deemed good for 12 patients (60%) and acceptable for 8 patients (40%). The mean time for performing the puncture was 100 sec ± 230 sec. No vascular complications were encountered. Two patients (10%) reported slight pain during puncture even after local anaesthesia was performed.
Table 1: Patients’ baseline clinical characteristics.
|
Parameter |
n = 20 |
|
|
Age (years) |
66.2 ± 11.8 |
|
|
Gender |
|
|
|
|
Male sex |
16 (80.0%) |
|
Diabetes |
5 (25.0%) |
|
|
Hypertension |
16 (80.0%) |
|
|
Active smoking |
4 (20.0%) |
|
|
History of coronary artery disease |
2 (10.0%) |
|
|
Peripheral artery disease |
1 (5.0%) |
|
|
Oral anticoagulation use |
2 (10.0%) |
|
|
O2 requirement |
20 (100%) |
|
|
Arterial blood gas analysis |
|
|
|
|
pH |
7.41 ± 0.08 |
|
|
PaO2 mmHg |
73.9 ± 15.9 |
|
|
PaCO2 mmHg |
36.75 ± 9.25 |
|
|
HCO3 mmol/l |
24±1 |
|
|
O2 saturation (%) |
88±9 |
In 1 patient (5%) no more than 1,5 cc of blood could be aspirated, probably related to a spasm and a loss of the arterial position which was difficult to regain. However, that amount of blood was enough for the analysis. No patient required an ultrasound-guided puncture. All access sites were reevaluated after 24 hours and no hematoma formation was noticed. The proximal radial artery was evaluated clinically through palpation with no suspected occlusion found in any of our patients.
Discussion
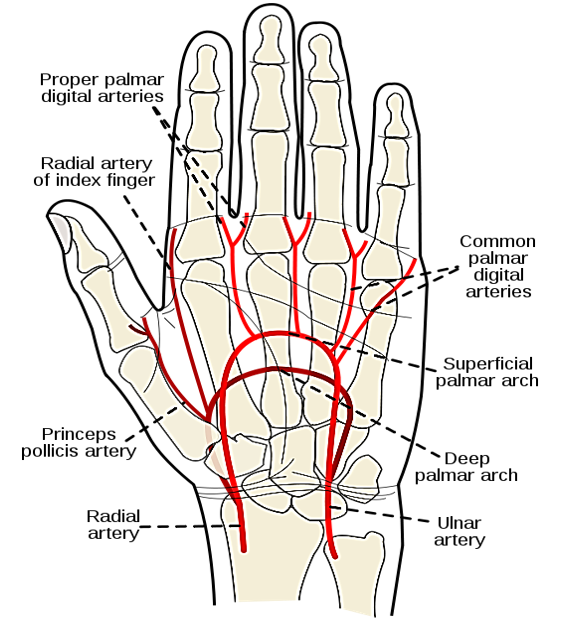
Distal radial artery access has been reported successful for coronary procedures [9]. Despite crossing with relatively larger diameter materials, the procedure was well tolerated by patients. No peripheral vascular complication was noticed. The low complication rate may be explained by the anatomical characteristics of the distal radial artery. The puncture is performed after the point where the radial artery gives origin to the branch for the superficial palmar arch (Figure 2), reducing both the risk of hand ischaemia and radial artery occlusion, while maintaining in case of occlusion an antegrade flow toward the hand with a virtually nonexistent risk of retrograde thrombus formation in the more proximal radial artery [9].
Another advantage for distal radial vascular access is the safer compression in comparison with other classical vascular access sites such as femoral artery puncture hence reducing the risk of hematoma formation. The bony floor granted by the trapezium and scaphoid along with the extremely superficial path of the artery allows for an easy compression that, together with a slightly smaller diameter when compared to the more usual radial artery access site, facilitates hemostasis while mitigating at the same time any risk for compartment syndrome [10]. The learning curve for the distal radial artery puncture would be expected to be complete after only 5 successful procedures and seems to be a straightforward process related to anatomic consideration. The artery may be difficult to palpate in some patients, in case of overlying edema or vasospasm and an ultrasound probe could be used. In our series of patients, even in difficult clinical scenarios with patients in unstable condition, all the distal radial punctures were performed without ultrasound guidance.
Figure 2: Distal radial artery anatomy. Reproduced from Wikimedia Commons Link
Our case series has several limitations, including the small number of a single-arm cohort. Punctures were done on admission in the emergency department setting. Another limitation is the fact that no repeat puncture was done for our patients.
Conclusion
Distal radial artery puncture for ABGs analysis appears to be safe and feasible for COVID-19 patients. The distal radial vascular access seems safer to puncture than other conventional vascular access related to its superficial path, its smaller diameter and easy compression. A larger cohort study should be undertaken for further evaluation in an intensive care setting, nevertheless this report serves as a proof-of-concept in the future.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 10, Nov 2020Accepted: Tue 24, Nov 2020
Published: Wed 09, Dec 2020
Copyright
© 2023 Ungureanu Claudiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.EJCR.2020.01.03
Author Info
Ungureanu Claudiu J. Auslender A. de Meester C. Ghafari Stéphane Carlier
Corresponding Author
Ungureanu ClaudiuDepartment of Cardiology, Université de Mons (UMONS), Mons, Belgium
Figures & Tables
Table 1: Patients’ baseline clinical characteristics.
|
Parameter |
n = 20 |
|
|
Age (years) |
66.2 ± 11.8 |
|
|
Gender |
|
|
|
|
Male sex |
16 (80.0%) |
|
Diabetes |
5 (25.0%) |
|
|
Hypertension |
16 (80.0%) |
|
|
Active smoking |
4 (20.0%) |
|
|
History of coronary artery disease |
2 (10.0%) |
|
|
Peripheral artery disease |
1 (5.0%) |
|
|
Oral anticoagulation use |
2 (10.0%) |
|
|
O2 requirement |
20 (100%) |
|
|
Arterial blood gas analysis |
|
|
|
|
pH |
7.41 ± 0.08 |
|
|
PaO2 mmHg |
73.9 ± 15.9 |
|
|
PaCO2 mmHg |
36.75 ± 9.25 |
|
|
HCO3 mmol/l |
24±1 |
|
|
O2 saturation (%) |
88±9 |
References
- Wu Z, McGoogan JM (2020) Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 323:1239-1242. [Crossref]
- Xie J, Covassin N, Fan Z, Singh P, Gao W et al. (2020) Association Between Hypoxemia and Mortality in Patients With COVID-19. Mayo Clin Proc 95: 1138-1147. [Crossref]
- Tobin MJ (2020) Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med 201: 1319-1320. [Crossref]
- Dev SP, Hillmer MD, Ferri M (2011) Videos in clinical medicine. Arterial puncture for blood gas analysis. N Engl J Med 364: e7. [Crossref]
- Weiner R, Ryan E, Yohannes Tomicich J (2016) Arterial Line Monitoring and Placement. AccessAnesthesiology | McGraw-Hill Medical.
- Patel KN, Gandhi SP, Sutariya HC (2016) Radial artery pseudoaneurysm: A rare complication after a single arterial puncture for blood-gas analysis. Indian J Crit Care Med 20: 622-626. [Crossref]
- Scheer B, Perel A, Pfeiffer UJ (2002) Clinical review: Complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care 6: 199-204. [Crossref]
- Yoo BS, Yoon J, Ko JY, Kim JY, Lee SH et al. (2005) Anatomical consideration of the radial artery for transradial coronary procedures: Arterial diameter, branching anomaly and vessel tortuosity. Int J Cardiol 101: 421-427. [Crossref]
- Kiemeneij F (2017) Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention 13: 851-857. [Crossref]
- Corcos T (2019) Distal radial access for coronary angiography and percutaneous coronary intervention: A state-of-the-art review. Catheter Cardiovasc Interv 93: 639-644. [Crossref]
