Factors Influencing the Prognosis of Acute Myeloid Leukemia
A B S T R A C T
Objective: To investigate the prognostic factors of adult acute myeloid leukemia (AML).
Methods: A total of 51 patients with AML initially treated in Zhongda Hospital affiliated to Southeast University in the past 7 years were selected to investigate the gender, age (60-year-old) and WBC count (>=30*109/L), whether there is a history of MDS and other factors related to survival rate.
Results: The results showed that age and the history of MDS prodrome were independent prognostic factors affecting OS. The OS rates of CD19 negative, CD11b positive and CD64 negative patients were significantly lower than those without the above factors at the onset of the disease, and the differences were statistically significant (all P<0.05).
Conclusion: The prognosis of AML patients is affected by multiple factors, so prognosis should be stratified according to risk factors, and appropriate chemotherapy regimens should be selected for patients of different age groups.
Keywords
Acute myeloid leukemia, survival rate, influencing factors
Introduction
Acute myeloid leukemia (AML) is a common malignancy of the blood system. Most patients are so ill that if not treated promptly and effectively, it often results in death. In recent years, with the development and improvement of chemotherapy drugs and regimens, the complete remission rate of this disease has been significantly improved, but there is still much room for improvement in the long-term survival rate. Acute leukemia is a malignant clonal disease of hematopoietic stem cells, characterized by infection, bleeding, anemia and infiltration of extramedullary tissues and organs. The disease progresses rapidly with a natural course of only weeks to months. Acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) can be divided into two groups according to the series of leukemic cells. Acute myeloid leukemia (AML) is a common hematopoietic tumor characterized by the proliferation and accumulation of leukemia cells in the bone marrow and other hematopoietic tissues, resulting in suppression of normal hematopoietic activity and infiltration of other organs and tissues.
Most AML patients are so severe that untreated treatment can result in death. With the improvement of chemotherapeutic drugs and chemotherapy methods, the complete response rate of patients can reach 70%-90%, but the duration of complete response and GT; the 5-year survival rate for adult AML is 20% to 40% [1]. Previous studies have pointed out that individualized treatment regiments are adopted in clinical practice in addition to timely treatment, and treatment regiments according to patients’ actual conditions are beneficial to patients’ long-term survival, which is also an important reason for patients with acute myeloid leukemia to achieve a high rate of complete remission and disease-free survival [2]. Therefore, it is necessary to find out the factors affecting the long-term survival of leukemia so as to provide some help for the formulation of an individualized treatment plan in clinical practice so that more patients can prolong their lives and achieve the goal of cure. Xiaoli Wang had performed such a study on survival in acute myeloid leukemia a negative phase relationship with age, but Claudia Bănescu et al. has shown that FLT3-ITD mutation or not, lactate dehydrogenase (LDH) levels, such as level of platelet count in acute myeloid leukemia have a certain influence on the total survival [3, 4]. In addition, many previous studies have proposed the relationship between cytogenetics, molecular biology, first-induced remission and overall survival [5]. The prognostic factors of acute myeloid leukemia were further investigated by retrospective analysis.
Materials and Methods
I The Research Object
A total of 51 patients with acute myeloid leukemia in the past 7 years were selected from Zhongda Hospital, except the patients with acute promyelocytic leukemia and allogeneic hematopoietic stem cell transplantation. There were 28 males and 23 females, aged from 26 to 90 years old, among whom there were a large number of elderly patients. All patients met the diagnostic criteria for AML.
II To Observe the Standard
Including the patient's age, sex, the number of white blood cells initially treated, the proportion of bone marrow original cells, whether there is a history of MDS, immune typing and other indicators.
III Evaluation Standard
Overall survival (OS) time was defined as the cut-off date of self-diagnosed solstice death or follow-up, and the overall survival (OS) time was defined as the cut-off date of abandoned or lost follow-up cases. The follow-up ended on June 1, 2020.
Results
I Clinical Characteristics of Patients
Among the 51 patients, 28 were male (54.9%) and 23 were female (45.1%). The median age was 66 years old (26 ~ 90 years old), and the elderly patients were the majority. White blood cell count in blood routine examination and GT; there are 16 cases of 30 times 10 to the ninth over L; 9 patients had a history of MDS in the prodrome.
II Analysis of Patient Survival and Related Influencing Factors
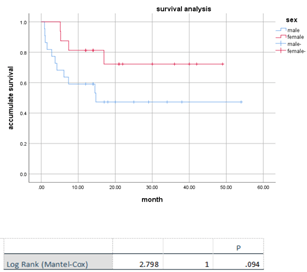
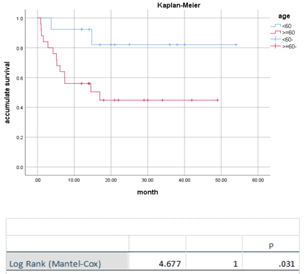
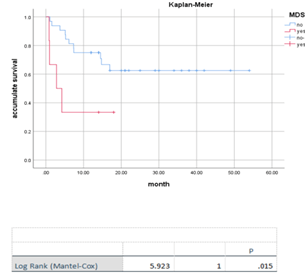
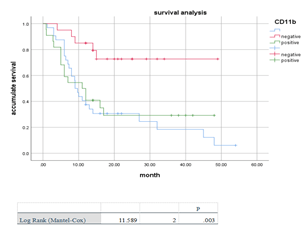
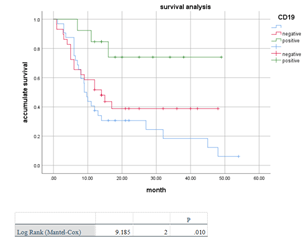
Of the 51 patients, 23 survived and 28 died, with an average survival time of 34.001 (±3.994) months. Of the 9 MDS patients, only 2 survived. The efficacy analysis showed that the overall survival rate of patients aged ≥60 years with a history of MDS prodrome was significantly lower than that of patients without the above factors, and the difference was statistically significant(P>0.05) (Figures 1-3). Univariate survival analysis was performed on 51 patients with age (≥60 years old), history of precursor MDS, gender, number of newly diagnosed white blood cells, percentage of bone marrow original cells and other factors. The results showed that age and history of precursor MDS were independent prognostic factors affecting OS. The survival curves of patients with different influencing factors are shown in (Figures 4 & 5). At the same time, univariate survival analysis showed that the OS rates of patients with negative CD19, positive CD11b and negative CD64 at the onset of the disease were significantly lower than those without the above factors, and the differences were statistically significant(P<0.05) (Figures 6-8).
Figure 1: Survival curves of AML patients based on gender (P>0.05).
Figure 2: Survival curve of patients with AML based on initial white blood cell count (P>0.05).
Figure 3: Survival curves of AML patients based on different proportions of primitive cells (P>0.05).
Figure 4: Survival curves of AML patients based on different ages (P=0.031).
Figure 5: Survival curves of AML patients based on the history of precursor MDS (P=0.015).
Figure 6: Survival curve of AML patients based on cell CD11b expression (P=0.003).
Figure 7: Survival curve of AML patients based on cell CD64 expression (P=0.02).
Figure 8: Survival curve of AML patients based on cell CD19 expression (P=0.01).
Discussion
In recent years, considerable progress has been made in achieving higher rates of mitigation and long-term survival through programme optimization, but long-term survival remains unsatisfactory. Studies have shown that many factors are related to the treatment effect and long-term survival of patients with leukemia. In order to better guide the decision of clinical treatment plan and the judgment of prognosis of patients, it is increasingly important to analyse the factors affecting the treatment effect and prognosis of patients with leukemia. It has been reported that age is an independent factor in the long-term prognosis of AML patients, with a CR rate of only 50% in elderly AML patients and a median survival of only 5-6 months [5].
There is a certain correlation between the long-term survival of patients and their age of onset because the older the patients are the worse the prognostic effect will be. It is generally believed that this is related to the elderly patients’ susceptibility to death due to infectious bleeding and systemic organ failure at the early stage of chemotherapy. Through the observation of the clinical situation, the long-term survival of patients with clinical symptoms and the long-term survival in patients with no evident difference between the original amount of young cells and bone marrow comparative there is no obvious difference between the two, but the long-term survival of patients with a more sensitive drugs tactility, easily through chemotherapy. Immunotyping can not only help to diagnose and differentiate leukemia but also act as an independent factor for risk stratification of AML. The achievement of CR in the first induction is crucial for the long-term survival of AML. Clinical statistics show that patients who obtain CR after one course of treatment have longer disease-free survival, while patients who fail to achieve CR after one course of treatment have a poor prognosis [6].
Allogeneic hematopoietic stem cell transplantation is the main cure for acute myeloid leukemia at present. According to the analysis of data from the Fred Hutchinson Institute and the International Bone Marrow Transplant Registry, the disease-free survival rate after 3 years of AML was about 50% in patients with complete remission after the first chemotherapy, while it was only 18%-27% in patients with chemotherapy alone [7]. In this study, 51 cases of regular treatment before transplantation in AML patients, more than one-year disease-free survival rate of 34.8%, more than 2 years of disease-free survival rate was 28.8%, more than 3 years of disease-free survival rate was 25.8%, and 5-year disease-free survival rate was 20%, in comparison, excluding the 17 cases of patients who had undergone stem cell transplantation therapy in 13 cases, 4 cases of death, the survival rate was 69.23%. It also supports the efficacy of allogeneic hematopoietic stem cell transplantation in treating acute myeloid leukemia. Allogeneic hematopoietic stem cell transplantation (HSCT) combines chemoradiotherapy with immunotherapy, i.e., the graft’s anti-leukemia effect, effectively reducing the recurrence rate of leukemia.
To sum up, the prognosis of AML patients is affected by multiple factors, and the prognosis should be stratified according to risk factors. Appropriate chemotherapy regimens should be selected for patients of different age groups to achieve CR in the early stage. Allogenic HSCT should be carried out as far as possible for high-risk cytogenetics patients to extend the survival time and improve the quality of life [6]. Bone marrow transplantation is an effective treatment, but transplant-related mortality remains high, limiting further improvement in overall survival.
Funding
This work was supported by Key Medical Projects of Jiangsu Province (ZDXKB2016020) and Jiangsu Social Development Project (BE2018711).
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 24, Nov 2021Accepted: Wed 08, Dec 2021
Published: Wed 29, Dec 2021
Copyright
© 2023 Bao-An Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2021.12.01
Author Info
Yi-Qian ZHU Fei Wang Xue Wu Bao-An Chen
Corresponding Author
Bao-An ChenDepartment of Hematology (Key Department of Jiangsu Medicine), Zhongda Hospital, Medical School, Southeast University, Nanjing, Jiangsu Province, China
Figures & Tables



References
1.
Huaixiu Y (2010) Clinical analysis of 23 cases of
long-term survival acute myeloid leukemia. Dis Surveillance Control 3:
163-165.
2.
Huili X (2016) Clinical analysis of long-term survival
acute myeloid leukemia. China Prac Med 11: 15.
3.
Xiaoli W, Minzhi L, Hongbo C (2007) Clinical study of
disease - free survival in patients with acute leukemia for more than 10 years.
J Clin Hematol 20: 6.
4.
Bănescu C, Tripon F, Trifa AP, Crauciuc AG, Moldovan VG
et al. (2019) Cytokine rs361525, rs1800750, rs1800629, rs1800896, rs1800872,
rs1800795, rs1800470, and rs2430561 SNPs in relation with prognostic factors in
acute myeloid leukemia. Cancer Med 8: 5492-5506. [Crossref]
5.
Rollig C, Thine C, Gramatzki M, Aulitzky W, Bodenstein H
et al. (2010) A novel prognostic model in elderly patients with acute myeloid
leukemia: results of 909 patients entered into the prospective AML 96 trial. Blood
116: 971-978. [Crossref]
6. Estey EH, Shen Y, Thall PF (2000) Effect of time to complete remission on subsequent survival and disease-free survival time in AML, RAEB-t, and RAEB. Blood 95: 72-77. [Crossref]
7. Suijing W, Xin D, Jianyu W, Zesheng L (2003) Survival analysis of 104 adult patients with acute leukemia. Clin Focus 18: 12.
