Epithelial Inclusion Cyst of the Foot Causing Pressure Ulcer and Skin Breach
A B S T R A C T
Epithelial inclusion cysts are benign lesions that rarely occur in the extremities in the absence of trauma. They may demonstrate slow but progressive enlargement.
This case relates to a 50 year old female who presented with a grade 1 pressure ulcer to the plantar surface of her right foot, associated with discomfort mobilising and pain upon wearing traditional footwear.
Surgical excision was performed, and histology demonstrated an epithelial inclusion cyst, leading to complete recovery and resolution of the plantar pressure ulcer.
Introduction
Epithelial inclusion cysts, also known as epidermal cysts or infundibular cysts are benign cutaneous or subcutaneous lesions lined by stratified squamous epithelium. They are common in areas that bare hair, primarily forming from the infundibular portion of a hair follicle, the result of a blocked sebaceous gland. They are commonly found on the face, scalp, neck, back, and scrotum. Presence in the extremities is usually secondary to inclusion of the epidermis into the dermis following trauma, or via the mechanism of Human Papilloma Virus infection causing implantation and proliferation of squamous cells into the dermis [1]. They commonly present as a freely movable cystic mass, often with a central punctum.
Epithelial inclusion cysts can range from a few millimetres to centimetres in size, with their natural history highly variable. They may remain stable or progressively enlarge over time, alongside their ability to become infected, causing significant discomfort for patients [2]. The WHO and Enzinger modification recognises up to 82 different benign and malignant soft tissue lesions of 10 histological subtypes appearing in the foot, meaning that diagnostic uncertainty is probable in the absence of histological findings [3].
Background and Presentation
A 50 year old female was referred to the foot and ankle clinic by her GP due to a persistent, progressive swelling in the right first web space. The patient did not recall any foot trauma. This swelling was becoming increasingly uncomfortable and difficult to accommodate in standard footwear options, and had led to a grade 1 pressure ulcer with callosity forming on the plantar surface of the foot (Figure 1). Prior to investigation, a ganglion cyst or bursal Neuroma complex were considered the most likely differentials.
Clinical Findings and Investigations
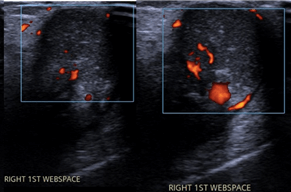
Following assessment in the foot and ankle clinic, a firm, mobile, non-pulsatile and non-transilluminant mass was identified. Plain film radiographs showed no evidence of bony injury or periosteal reaction, and so further imaging investigations including ultrasound scanning and an MRI were undertaken, demonstrating a ‘cystic lesion’. Following concerns of the presence of arteriovenous malformation (AVM) (Figure 3), vascular surgery opinion was sought. Whilst this cystic structure was supplied by a single vessel, it was deemed appropriate for removal under the care of the foot and ankle team.
Figure 1: Grade 1 pressure ulcer of the planar surface of the foot secondary to a cystic mass.
Figure 2: Weight bearing X-rays of the right foot.
Figure 3: Ultrasound doppler assessment of webspace mass.
Figure 4: T1-weighted MRI imaging of the right foot.
Figure 5: T2-weighted MRI imaging of the right foot.
Figures 6 and 7: Intraoperative image demonstrating cystic mass at the time of resection.
Interventions and Outcome
The lesion was excised in the operating theatre via a dorsal incision under spinal anaesthetic, with the surgeon describing a firm, encapsulated mass with a finger like projection. Post-operatively the patient was mobilised in forefoot weight offloading footwear and followed up at clinic with histology results.
Histologically, the lesion was described as a cystic mass measuring 30 × 20 × 15mm with a smooth, orange and white external surface. Sizing showed a thin-walled cyst with firm pale to orange contents. Microscopically the specimen was confirmed as a ruptured and inflamed epithelial inclusion cyst. The patients reported outcomes were highly satisfactory, with complete resolution of the presenting symptoms and the area of pressure ulceration post-operatively.
Relevance and Impact
Whilst benign, this epithelial inclusion cyst became large enough to cause pressure damage under the first web space of the foot. Progressive enlargement in the absence of infection, and the inability to wear footwear comfortably were the deciding factors in opting for operative management at this time, however care needed to be taken to ensure that appropriate imaging took place for identification of suspicious or important perioperative features such as the presence of an arteriovenous malformation.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 01, May 2023Accepted: Tue 16, May 2023
Published: Mon 17, Jul 2023
Copyright
© 2023 Niall Fitzpatrick. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2023.02.03
Author Info
Niall Fitzpatrick Ahmad Bilal Anand Pillai
Corresponding Author
Niall FitzpatrickWythenshawe Hospital, Manchester University NHS Foundation Trust, Manchester, United Kingdom
Figures & Tables





References
1.
Nigam JS, Bharti
JN, Nair V, Gargade CB, Deshpande AH et al. (2017) Epidermal Cysts: A
Clinicopathological Analysis with Emphasis on Unusual Findings. Int J
Trichology 9: 108-112. [Crossref]
2. Weir CB, St. Hilaire NJ (2023) Epidermal Inclusion Cyst. Statpearls [Internet]. [Crossref]
3. Goldblum J, Folpe A, Weiss S (1983) Soft tissue tumours. El Selvier, London.
