Epidemiologic Study of Central Nervous System Tumors in Rwanda
A B S T R A C T
Introduction: Tumors of the central nervous system (CNS) are primary or secondary neoplasms located within the craniovertebral cavity. The incidence of CNS tumors is not uniform with variation between different countries, age groups and races.
Objective: Our study aim was to generate new knowledge of the epidemiology of central nervous system tumors in Rwanda.
Method: This was an observational retrospective study of all patients diagnosed with CNS tumors in Rwanda over a period of 10 years, from 1st January 2006 to 31st December 2015.
Results: 466 patients enrolled, (52.2% females, 47.8% males). The median age at diagnosis of was 37 years. Brain tumors were 82.7%; spine tumor patients were 16.4%. The average annual age-standardized incidence of CNS tumors was 0.43/100, 0000 person-years and varied with age groups. Tumors of meningothelial cells represented the majority of brain tumors (31.8%). Metastatic tumors were the far most common spine tumors category. 55.8 % of CNS tumors reported in our study were histologically confirmed and of non-malignant meningiomas were the commonest (33.9%).
Conclusion: This is the very first study done on epidemiology of CNS tumors in Rwanda, and generated data about incidence of CNS tumors in Rwanda and their location and histological distribution.
Keywords
CNS tumors, epidemiology, incidence, brain tumors, spine tumors, Rwanda, Africa
Introduction
Tumors of the central nervous system (CNS) are primary or secondary neoplasms located within the craniovertebral cavity [1]. Different types of CNS tumors have been identified and coded [1, 2]. Although CNS tumors represent a small proportion of all cancers and cancer-related mortality, most of the brain tumors are malignant and fatal and both malignant and benign brain tumors can cause significant neurological deficits that interfere with activities of daily living. Primary brain tumors are the most common solid tumors among patients aged <20 years and represent the second leading cause of cancer deaths in the same age group and the fifth leading cause of cancer-related death among women aged 20-39 years [3].
Primary spine tumors occur less frequently than metastatic spine tumors. The most common sources of metastatic spine tumors are the lungs, breast, prostate, lymphoma, and myeloma. Autopsy studies have indicated that 30%-90% lesions metastasize to the spine in patients with a history of other cancers. Among patients with other malignancies, 17% presented spinal cord compression secondary to the spinal metastatic disease [4]. With improvements in cancer diagnosis and treatment in general and the associated increase in long-term patient survival, increases in asymptomatic and symptomatic spinal metastases are expected. The thoracic spine is the leading location of metastases to the spine, followed by the lumbar and cervical spine [5].
The incidence of CNS tumors is not uniform, with variation among countries, age groups, and races. There is also a temporal increase in the incidence of CNS tumors, possibly due to the improvement in the reporting systems for these tumors, improvement in neuroimaging technology, and probable change in environmental exposure. However, there is a paucity of data on the epidemiology of CNS tumors in Africa, particularly in East Africa, with only two studies reporting on CNS tumors in Uganda [6, 7]. In Kenya, a single center-based study was conducted at Kenyatta National Hospital, Nairobi, on 214 patients with intracranial tumors who underwent brain surgery [8]. Another study performed in the same center evaluated tumors causing spinal cord compression [9].
Both studies were limited to a single center and selected patients; thus, one cannot conclude the incidence and demographic distribution of CNS tumors in East Africa based on these data. To our knowledge, no study has reported on the epidemiology of CNS tumors in Rwanda, a country with a population of approximately 12 million and with one of the world’s youngest neurosurgical services, the Rwanda Neurosurgical Centre, which was run by two neurosurgeons in two referral hospitals during the study period. The study results provided data on the epidemiology of CNS tumors in Rwanda.
Patients and Methods
This observational retrospective study included all patients diagnosed with CNS tumors in Rwanda during a 10-year period between January 1, 2006 and December 31, 2015. The study was conducted at the Rwanda Neurosurgical Centre, the unique neurosurgery center in Rwanda run by two neurosurgical services of two referral hospitals—Kigali University Teaching Hospital (Centre Hospitalier Universitaire de Kigali [CHUK]) and King Faisal Hospital (KFH) – and in the three anatomopathology departments of the following 3 referral hospitals of the country: KFH, CHUK, and Butare University Teaching Hospital (Centre Hospitalier Universitaire de Butare [CHUB]).
This study included all patients diagnosed with CNS tumors in Rwanda during the study period. We excluded CNS tumor recurrence and CNS tumors diagnosed by autopsy. Overlapping sources were used to identify the maximum number of eligible cases, including patient registries from the neurosurgery unit; operating room; and outpatient, pediatric, and radiology departments of CHUK and KFH as well as patient registries and pathology reports from the anatomopathology departments of CHUK, KFH, and CHUB. The patients’ files were consulted to verify the date of diagnosis and to ensure that the identified patients fit the inclusion criteria. Population estimates by age, sex, and calendar year were obtained from the reports of the National Institutes of Statistics and United Nations Demographic Statistics Yearbooks. The variables that were recorded included patient age and sex as well as tumor location, histological type, and grade.
Data collection forms were used to collect patient information. STATA 13.0 was used for data entry and statistical analysis. The statistical analysis involved computing the frequencies of demographic variables (age and sex). Frequencies of histological types and location of CNS tumors were also computed. The average age-adjusted incidence of CNS tumors were calculated using the standard populations proposed by the World Health Organization (WHO) in 2000 (Ahmad et al. 2000). Cross-tabulations between sex and other variables such as tumor location and histology were also computed. Furthermore, the analysis also included calculating the frequencies of histological types of CNS tumors according to locations within the cranial and vertebral compartments.
This study did not involve any physical or psychological injury or discomfort to the subjects. The potential risk was an exposure of subjects’ confidentiality and privacy. To maintain confidentiality and protect subject privacy, the participants’ names and hospital numbers were not recorded on the data collection sheets and each questionnaire was coded. Before starting this study, ethical approval was obtained from the Institutional Board Review (IRB) of the College of Medicine and Health Sciences of the University of Rwanda and the from hospital ethics committees. As this study was of minimal risk to participants, a waiver of consent was granted by the IRB of the College of Medicine and Health Sciences of the University of Rwanda.
Study Results
This study enrolled 466 patients (223 males and 243 females) diagnosed with CNS tumors in Rwanda between January 2006 and December 2015. The number of recorded cases increased from 1 case in 2006 to 141 cases in 2015 (Figure 1). Among these cases, 259 (55.8%) of them had histological diagnoses. Women were more often affected by CNS tumors (52.2%) than men (47.8%). CNS tumors were more common in adults (84.5%) than in the pediatric population (15.5%). The age range of our study population was 5 months to 94 years, with a median age at diagnosis of 37 years. Tumors of the brain, spine, and both occurred in 383 (82.7%), 76 (16.4%), and 4 patients, respectively (Table 1). The average annual age-standardized incidence of CNS tumors in Rwanda from 2006 to 2015 was 0.43/100, 0000 person-years, varied across age groups (Table 2 & Figure 2), and increased from 0.01/100,000 person in 2006 to 1.22/100,000 in 2015 (Figure 3).
Figure 1: Age adjusted incidence rates of CNS tumors.
Figure 2: Age-adjusted incidence rates of CNS tumors by year from 2006 to 2015.
Table 1: Demographic characteristics.
|
Characteristics |
n |
% |
||
|
Socio demographics |
Sex |
Male |
223 |
47.85 |
|
female |
243 |
52.15 |
||
|
Age group |
pediatric <14 years) |
72 |
15.45 |
|
|
Adult |
394 |
84.55 |
||
|
CNS part involved |
BRAIN |
383 |
82.72 |
|
|
SPINE |
76 |
16.41 |
||
|
|
BRAIN AND SPINE |
4 |
0.86 |
|
Figure 3: Age groups distribution of primary spine tumors.
Table 2: Age-group and gender specific incidence rates of CNS tumors.
|
Age groups |
male |
|
female |
|
Age standardised incidence rate |
|
|
|||
|
|
population size |
n |
average annual incidence (/100 000) |
population size |
n |
average annual incidence (/100,000) |
person-years at risk |
n |
WHO standard population |
Annual age standardised incidence rate (/100,000) |
|
0-4 |
815244 |
16 |
0.20 |
816355 |
9 |
0.11 |
16315992 |
25 |
8860 |
0.01 |
|
5-9 |
735332 |
16 |
0.22 |
736127 |
10 |
0.14 |
14714593 |
26 |
8690 |
0.02 |
|
10-14 |
619258 |
11 |
0.18 |
628950 |
10 |
0.16 |
12482078 |
21 |
8600 |
0.01 |
|
15-19 |
551430 |
17 |
0.31 |
563950 |
12 |
0.21 |
11153799 |
29 |
8470 |
0.02 |
|
20-24 |
522025 |
15 |
0.29 |
494595 |
8 |
0.16 |
10166195 |
23 |
8220 |
0.02 |
|
25-29 |
447497 |
24 |
0.54 |
486170 |
20 |
0.41 |
9336669 |
44 |
7930 |
0.04 |
|
30-34 |
324318 |
11 |
0.34 |
373770 |
19 |
0.51 |
6980885 |
30 |
7610 |
0.03 |
|
35-39 |
223797 |
23 |
1.03 |
274635 |
27 |
0.98 |
4984317 |
50 |
7150 |
0.07 |
|
40-44 |
177162 |
18 |
1.02 |
225474 |
23 |
1.02 |
4026359 |
41 |
6590 |
0.07 |
|
45-49 |
152985 |
13 |
0.85 |
201292 |
22 |
1.09 |
3542765 |
35 |
6040 |
0.06 |
|
50-54 |
124734 |
11 |
0.88 |
172905 |
15 |
0.87 |
2976384 |
26 |
5370 |
0.05 |
|
55-59 |
91838 |
11 |
1.20 |
131175 |
22 |
1.68 |
2230124 |
33 |
4550 |
0.07 |
|
60-64 |
67047 |
14 |
2.09 |
96459 |
7 |
0.73 |
1635058 |
21 |
3720 |
0.05 |
|
65-69 |
41590 |
3 |
0.72 |
64829 |
11 |
1.70 |
1064188 |
14 |
2960 |
0.04 |
|
70-74 |
31319 |
3 |
0.96 |
46154 |
6 |
1.30 |
774727 |
9 |
2210 |
0.03 |
|
75-79 |
23046 |
5 |
2.17 |
30484 |
4 |
1.31 |
535305 |
9 |
1520 |
0.03 |
|
80+ |
19358 |
4 |
2.07 |
25386 |
5 |
1.97 |
447436 |
9 |
1510 |
0.03 |
|
Total |
4967878 |
215 |
0.43 |
5368710 |
230 |
0.43 |
103840826 |
445 |
100000 |
0.43 |
Table 3: CNS tumors location.
|
|
BRAIN |
SPINE |
|||||
|
n |
% |
n |
% |
||||
|
cranial |
supratentorial |
Intraaxial |
hemispheric |
128 |
33.4 |
|
|
|
basal ganglia |
1 |
0.3 |
|||||
|
pineal |
2 |
0.5 |
|||||
|
ventricular |
2 |
0.5 |
|||||
|
extraaxial |
olfactory groove |
12 |
3.1 |
||||
|
sellar |
33 |
8.6 |
|||||
|
suprasellar/parasellar |
35 |
9.1 |
|||||
|
cavernous sinus |
3 |
0.8 |
|||||
|
sphenoid wing |
18 |
4.7 |
|||||
|
parasagittal |
16 |
4.2 |
|||||
|
|
not specified |
10 |
2.6 |
||||
|
ALL |
265 |
69.2 |
|||||
|
infratentorial |
Intraaxial |
cerebellar |
31 |
8.1 |
|||
|
brainstem |
10 |
2.6 |
|||||
|
4th ventricle |
6 |
1.6 |
|||||
|
|
extraaxial |
cerebello-pontine angle |
15 |
3.9 |
|||
|
tentorial |
1 |
0.3 |
|||||
|
clival |
2 |
0.5 |
|||||
|
NOS |
10 |
2.6 |
|||||
|
|
ALL |
75 |
19.6 |
||||
|
supratentorial and infratentorial |
2 |
0.5 |
|||||
|
not specified |
23 |
6.0 |
|||||
|
spinal |
spine segment |
cervical |
9 |
11.8 |
|||
|
thoracic |
27 |
35.5 |
|||||
|
lumbar |
19 |
25.0 |
|||||
|
all segments |
3 |
3.9 |
|||||
|
not specified |
21 |
27.6 |
|||||
|
Spine compartment |
extradural |
38 |
50.0 |
||||
|
intradural-extramedullary |
17 |
22.4 |
|||||
|
intramedullary |
4 |
5.3 |
|||||
|
not specified |
22 |
28.9 |
|||||
I CNS Tumor Locations
Supratentorial tumors occurred in 265 patients (69.2% of brain tumors), among which intra-axial hemispheric tumors comprised almost half (n=128; 33.4% of all brain tumors). The thoracic spine was the most common segment affected by spine tumors (n= 27; 35.5%) followed by lumbar and cervical spine segments (25% and 11.8% respectively). Spine tumors most commonly affected the vertebral body (n=34; 44.7%), as well as the extradural and intramedullary compartments (5.3% of cases each), whereas intradural-extradural spine tumors comprised 22.4% of spine tumors (n=17) (Table 3). Brain tumors occurred most frequently in the cerebral hemispheres of both adult and pediatric patients. However, the distribution of brain tumors in the supratentorial and infratentorial compartments differed between these patient populations. Only 14.2% of brain tumors in adults were located infratentorial compared to 42.3% in children (Table 4).
Table 4: Brain tumors location in adults and children(0-14 years).
|
Location site |
adult |
pediatric |
|||
|
n |
% |
n |
% |
||
|
supratentorial |
hemispheric |
112 |
30.5 |
18 |
25.4 |
|
sellar |
31 |
8.4 |
2 |
2.8 |
|
|
suprasellar/parasella |
19 |
5.2 |
16 |
22.5 |
|
|
pineal |
2 |
0.5 |
0 |
0.0 |
|
|
ventricular |
2 |
0.5 |
0 |
0.0 |
|
|
not specified |
39 |
10.6 |
3 |
4.2 |
|
|
parasaggital |
16 |
4.4 |
0 |
0.0 |
|
|
olfactory groove |
12 |
3.3 |
0 |
0.0 |
|
|
sphenoid wing |
17 |
4.6 |
1 |
1.4 |
|
|
cavernous sinus |
3 |
0.8 |
0 |
0.0 |
|
|
basal ganglia |
1 |
0.3 |
0 |
0.0 |
|
|
Total |
254 |
69.2 |
40 |
56.3 |
|
|
infratentorial |
cerebellar |
16 |
4.4 |
17 |
23.9 |
|
brainstem |
7 |
1.9 |
4 |
5.6 |
|
|
Cerebello-pontine ang |
16 |
4.4 |
1 |
1.4 |
|
|
fourth ventricle |
4 |
1.1 |
2 |
2.8 |
|
|
tentorial |
1 |
0.3 |
0 |
0.0 |
|
|
clival |
2 |
0.5 |
0 |
0.0 |
|
|
NOS |
6 |
1.6 |
6 |
8.5 |
|
|
Total |
52 |
14.2 |
30 |
42.3 |
|
|
Total |
|
367 |
|
71 |
|
II CNS Tumor Categories According to 2016 WHO CNS Tumor Classification
The largest proportion of brain tumors were meningothelial cell tumors, which occurred in 105 patients (31.8%), followed by diffuse astrocytic and oligodendroglial tumors (30%). The other common tumor categories were tumors of the sellar region (n=54; 16.4%), metastatic tumors (n=21; 6.4%), mesenchymal and non-meningothelial tumors (n=14; 4.2%), and embryonal tumors (n=13; 3.9%). Among spine tumors, metastatic tumors were the most common category (49.3%), followed by tumors of meningothelial cells (14.9%), mesenchymal and non-meningothelial tumors (13.4%), and tumors of cranial and paraspinal nerves (11.9%) (Table 5).
Table 5: CNS tumors category.
|
CNS Tumor category |
brain |
spine |
Concomitant brain and spine |
||
|
n |
% |
n |
% |
n |
|
|
Diffuse astrocytic and oligodendroglial |
99 |
30.0 |
2 |
3.0 |
0 |
|
Other astrocytic tumor |
7 |
2.1 |
0 |
0.0 |
0 |
|
Ependymal tumors |
6 |
1.8 |
0 |
0.0 |
2 |
|
Other gliomas |
1 |
0.3 |
0 |
0.0 |
0 |
|
Choroid plexus tumors |
1 |
0.3 |
0 |
0.0 |
0 |
|
Embryonal tumors |
13 |
3.9 |
1 |
1.5 |
0 |
|
Tumors of cranial and paraspinal nerve |
3 |
0.9 |
8 |
11.9 |
0 |
|
Tumors of meningothelial cells |
105 |
31.8 |
10 |
14.9 |
0 |
|
Mesenchymal, non-meningothelial tumors |
14 |
4.2 |
9 |
13.4 |
0 |
|
Lymphomas |
5 |
1.5 |
4 |
6.0 |
0 |
|
Germ cell tumors |
1 |
0.3 |
0 |
0.0 |
0 |
|
Tumors of the sellar region |
54 |
16.4 |
_ |
_ |
_ |
|
metastatic tumors |
21 |
6.4 |
33 |
49.3 |
2 |
III Distribution of CNS Tumor Histology Types
Glioblastoma multiforme and diffuse astrocytoma accounted for 8.9 % of all CNS tumors, each, and were the most frequent histology types of diffuse astrocytic and oligodendroglial tumors. WHO grade I astrocytic tumors were 3.1% of all CNS tumors and Ependymal tumors made 2.7% of all CNS tumors histological types (Table 6). Meningothelial meningioma was the most common histology type amongst all tumors of meningothelial cells (11.6% of all CNS tumors). WHO grade I meningiomas histology types comprised a total of 33.7 % of all CNS tumors. Hemangioblastomas were the most common type of mesenchymal non-meningothelial cell tumors (1.9% of all CNS tumors histology types) (Table 7). Histology types of other CNS tumors are shown in (Tables 8, 9, & 10). Histology diagnosis was obtained for 15 metastatic tumors to the CNS. Lungs were the most frequent site of primary lesions as either adenocarcinoma (0.8%) or small cell carcinoma (0.8%). Metastases from melanomas were found in 3 cases (1.2% of all CNS tumors) (Table 11).
Table 6: Distribution of histology types of diffuse astrocytic and oligondroglial tumors, other astrocytic Tumors, ependymoma tumors and choroid plexus tumors.
|
Histology type |
n |
% |
|
Diffuse astrocytic and oligodendroglial tumors |
66 |
25.5 |
|
anaplastic oligoastrocytoma |
1 |
0.4 |
|
anaplastic oligodendroglioma |
1 |
0.4 |
|
astrocytoma NOS |
4 |
1.5 |
|
anaplastic astrocytoma |
8 |
3.1 |
|
diffuse astrocytoma |
23 |
8.9 |
|
glioblastoma multiforme |
23 |
8.9 |
|
high grade astrocytoma |
1 |
0.4 |
|
oligoastrocytoma |
2 |
0.8 |
|
oligodendroglioma |
3 |
1.2 |
|
other astrocytic tumors |
8 |
3.1 |
|
pilocystic astrocytoma |
7 |
2.7 |
|
pleomorphic xanthoastrocytoma |
1 |
0.4 |
|
Ependymal tumors |
7 |
2.7 |
|
anaplastic ependymoma |
1 |
0.4 |
|
ependymoma |
4 |
1.5 |
|
myxopapillary ependym |
1 |
0.4 |
|
papillary ependymoma |
1 |
0.4 |
|
Choroid plexus tumors |
1 |
0.4 |
|
Choroid plexus carcinoma |
1 |
0.4 |
IV Adults Brain Tumor Distribution
Tumors of meningothelial cells were more prevalent than diffuse gliomas in adults (30.57% versus 24.38%). Tumors of the sellar region were the third-most common brain tumors among adults (12.59%), while metastatic brain tumors occurred in 16.18% of brain tumors in adults (Figure 4).
Figure 4: Brain tumors categories in adults.
V Pediatric Brain Tumor Distribution
In the pediatric subgroup of our study population, diffuse astrocytic and oligodendroglial tumors were more prevalent than tumors of meningothelial cells (29% versus 18%). Tumors of the sellar region were as frequent as meningothelial cells tumors (18%). Embryonal tumors including medulloblastomas occurred in 13% of all pediatric brain tumors, while ependymoma comprised 5% of “other astrocytic tumors” (including pilocytic astrocytomas), which represented 8% of all brain tumors in children (Figure 2).
Figure 5: Brain Tumors categories in pediatric patients (age 0-14 years).
VI Primary Brain Tumors
Primary brain tumors occurred in 66.9% (n=312) of the study population. Females were more affected than males, with a female: male ratio of 1.2:1. Adults were significantly more frequently affected than children (81.1% versus 18.9%) (Table 12). Primary brain tumors were more commonly located in the supratentorial (74.7%) than the infratentorial compartment (21.8%) and tumors of meningothelial cells were significantly more common (33.7%), followed by diffuse astrocytic and oligodendroglial tumors (31.7%) (Tables 13 & 14). Primary brain tumors were more common in adults than in children (81.1% versus 18.9%; p=0.003). The differences in sex distribution and age groups distribution of primary brain tumors were not significant (Table 15). Among primary brain tumors, 74.7% were supratentorial and 45.9% were located in the cerebral hemispheres. The most common infratentorial locations of the primary brain tumors were the cerebellar hemispheres (44.1%) followed by the cerebellopontine angle (20.6%) (Table 13). Tumors of meningothelial cells represented 33.7% and diffuse astrocytic and oligodendroglial tumors comprised 31.7% of primary brain tumors (Table 14).
Table 7: Histology types of meningothelial cells Tumors and mesenchymal non-meningothelial cells tumors.
|
Histology type |
n |
% |
|
Tumors of meningothelial cells |
95 |
36.7 |
|
anaplastic meningioma |
5 |
2 |
|
atypical meningioma |
3 |
1.2 |
|
clear cell meningioma |
1 |
0.4 |
|
fibrous meningioma |
8 |
3.1 |
|
meningioma NOS |
23 |
8.9 |
|
Meningothelial meningioma |
30 |
11.6 |
|
metaplastic meningoma |
1 |
0.4 |
|
microscystic meinigioma |
5 |
1.9 |
|
psamomatous meningioma |
10 |
3.9 |
|
transitional meningioma |
9 |
3.5 |
|
Mesenchymal, non-meningotheial cell Tumors |
20 |
7.7 |
|
chondrofibroma |
1 |
0.4 |
|
chondroma |
4 |
1.5 |
|
chondrosarcoma |
1 |
0.4 |
|
hemangioblastoma |
5 |
1.9 |
|
hemangioma |
2 |
0.8 |
|
lipoma |
1 |
0.4 |
|
osteoma |
4 |
1.5 |
|
sarcoma |
1 |
0.4 |
|
skull bone tumor |
1 |
0.4 |
Table 8: Histology types of Tumors of cranial and paraspinal tumors.
|
Histology type |
n |
% |
|
Plexiform neurofibroma |
1 |
0.4 |
|
biphasic schwannoma |
1 |
0.4 |
|
neurofibroma NOS |
2 |
0.8 |
|
schwannoma |
6 |
2.3 |
Table 9: Histology types of CNS lymphomas.
|
Histology type |
n |
% |
|
Lymphomas |
8 |
3.1 |
|
B cell lymphoma |
3 |
1.2 |
|
burkitt lymphoma |
3 |
1.2 |
|
hystiolytic lymphoma |
1 |
0.4 |
|
lymphoblastic lymphoma |
1 |
0.4 |
Table 10: Histology types of embryonal tumors and germ cell tumors.
|
Embryonal Tumors |
5 |
1.9 |
|
medullobastoma |
4 |
1.5 |
|
neuroectodermal Tumor |
1 |
0.4 |
|
Germ cell Tumors |
1 |
0.4 |
|
germinoma |
1 |
0.4 |
Table 11: Histology types of CNS metastatic tumors.
|
Histology type |
n |
% |
|
Metastatic Tumors |
15 |
5.8 |
|
adenocarcinoma NOS |
2 |
0.8 |
|
adenocarcinoma lung |
2 |
0.8 |
|
adenocarcinoma prostate |
1 |
0.4 |
|
carcinoma breast |
2 |
0.8 |
|
carcinoma from RCC |
1 |
0.4 |
|
lung SCC |
2 |
0.8 |
|
melanoma NOS |
3 |
1.2 |
|
metastatic bone Tumor NOS |
1 |
0.4 |
|
papillary carcinoma |
1 |
0.4 |
Table 12: Demographic characteristics of patients with primary brain tumors.
|
characteristics |
n |
% |
p value |
|
|
Gender |
female |
170 |
54.5 |
0.150 |
|
male |
142 |
45.5 |
||
|
age category |
adult |
253 |
81.1 |
0.003 |
|
paediatric |
59 |
18.9 |
||
|
Age group |
0-4 |
22 |
7.5 |
0.064 |
|
5-9 |
22 |
7.5 |
||
|
10-14 |
15 |
5.1 |
||
|
15-19 |
19 |
6.5 |
||
|
20-24 |
15 |
5.1 |
||
|
25-29 |
29 |
9.9 |
||
|
30-34 |
19 |
6.5 |
||
|
35-39 |
32 |
10.9 |
||
|
40-44 |
29 |
9.9 |
||
|
45-49 |
21 |
7.1 |
||
|
50-54 |
18 |
6.1 |
||
|
55-59 |
22 |
7.5 |
||
|
60-64 |
15 |
5.1 |
||
|
65-69 |
4 |
1.4 |
||
|
70-74 |
4 |
1.4 |
||
|
75-79 |
5 |
1.7 |
||
|
80+ |
3 |
1.0 |
||
VII Diffuse Astrocytic and Oligodendroglial Tumors
Diffuse astrocytic and oligodendroglial tumors were the second most common primary brain tumors (31.7%), with an annual age-standardized incidence rate of 0.095/100,000 person-years. The mean age of patients with brain diffuse astrocytic and oligodendroglial tumors was 35.2 years. The incidence was higher in males (0.11/100,000) than in females (0.08/100,000) and the age-standardized incidence was higher in adults (0.1/100,000) than in pediatric patients (0.011/100,000). The differences in incidence rates between sex and between adult and pediatric patients were not statistically significant (p=0.084 for sex and 0.397 for age categories). Diffuse astrocytic and oligodendroglial tumors were predominantly located in the supratentorial compartment (72.7%). The most common histological types were glioblastoma multiforme and diffuse astrocytoma (34.8% for both), followed by anaplastic astrocytoma (12.1%). The majority of diffuse astrocytic and oligodendroglial tumors were WHO grade II (40.9%) and IV (39.4%) (p=0.000) (Table 16).
Table 13: Primary brain tumors location.
|
Location |
n |
% |
P value |
||
|
supratentorial |
hemispheric |
107 |
45.9 |
0.000 |
|
|
basal ganglia |
1 |
0.4 |
|||
|
pineal |
2 |
0.9 |
|||
|
ventricular |
0 |
0.0 |
|||
|
olfactory groove |
12 |
5.2 |
|||
|
sellar |
32 |
13.7 |
|||
|
suprasellar/parasellar, |
31 |
13.3 |
|||
|
cavernous sinus |
3 |
1.3 |
|||
|
sphenoid wing |
18 |
7.7 |
|||
|
parasagittal |
16 |
6.9 |
|||
|
not specified |
11 |
4.7 |
|||
|
ALL |
233 |
74.7 |
|
||
|
infratentorial |
|
cerebellar |
30 |
44.1 |
0.010 |
|
brainstem |
9 |
13.2 |
|||
|
4th ventricle |
6 |
8.8 |
|||
|
|
|
cerebello-pontine angle |
14 |
20.6 |
|
|
tentorial |
1 |
1.5 |
|||
|
clival |
2 |
2.9 |
|||
|
NOS |
6 |
8.8 |
|||
|
|
ALL |
68 |
21.8 |
|
|
|
supratentorial and infratentorial |
|
1 |
|
|
|
|
not specified |
|
10 |
|
|
|
Table 14: Primary brain tumors categories according to 2016 WHO CNS tumors classification.
|
WHO CNS Tumor category |
n |
% |
P value |
|
Diffuse astrocytic and oligodendroglial |
99 |
31.7 |
0.000 |
|
Other astrocytic tumor |
7 |
2.2 |
|
|
Ependymal tumors |
8 |
2.6 |
|
|
Other gliomas |
1 |
0.3 |
|
|
Choroid plexus tumors |
1 |
0.3 |
|
|
Embryonal tumors |
13 |
4.2 |
|
|
Tumors of cranial and paraspinal nerve |
3 |
1.0 |
|
|
Tumors of meningothelial cells |
105 |
33.7 |
|
|
Mesenchymal, non-meningothelial tumors |
14 |
4.5 |
|
|
Lymphomas |
6 |
1.9 |
|
|
Germ cell tumors |
1 |
0.3 |
|
|
Tumors of the sellar region |
54 |
17.3 |
Table 15: Diffuse astrocytic and oligodendroglial tumors.
|
characteristics |
|
diffuse astrocytic and oligodendroglial tumors |
|
p value |
|
|
|
|
n |
% |
age-standardised incidence rate |
|
|
Gender |
female |
44 |
44.4 |
0.08 |
0.084 |
|
male |
55 |
55.5 |
0.11 |
||
|
age category |
adult |
81 |
81.8 |
0.1 |
0.397 |
|
pediatric |
18 |
18.2 |
0.011 |
||
|
location |
supratentorial |
72 |
72.7 |
|
0.000 |
|
infratentorial |
22 |
22.2 |
|
||
|
not specified |
4 |
4.0 |
|
||
|
histology type |
anaplastic oligoastrocytoma |
1 |
1.5 |
|
0.000 |
|
anaplastic oligodendroglioma |
1 |
1.5 |
|
||
|
astrocytoma NOS |
4 |
6.1 |
|
||
|
anaplastic astrocytoma |
8 |
12.1 |
|
||
|
diffuse astrocytoma |
23 |
34.8 |
|
||
|
glioblastoma multiforme |
23 |
34.8 |
|
||
|
high grade astrocytoma |
1 |
1.5 |
|
||
|
oligoastrocytoma |
2 |
3.0 |
|
||
|
oligodendroglioma |
3 |
4.5 |
|
||
|
tumor grade |
II |
27 |
40.9 |
|
0.000 |
|
III |
13 |
19.7 |
|
||
|
IV |
26 |
39.4 |
|
||
Table 16: Tumors of meningothelial cells: demographic characteristics and location.
|
characteristics |
n |
% |
Incidence rate |
p value |
|
|
female |
68 |
64.8 |
0.13 |
0.003 |
|
|
male |
37 |
35.2 |
0.07 |
||
|
adult |
|
94 |
89.5 |
0.12 |
0.109 |
|
pediatric |
|
11 |
10.5 |
0.007 |
|
|
supratentorial |
convexity |
30 |
28.6 |
|
0.000 |
|
suprasellar/parasellar |
6 |
5.7 |
|
||
|
parasaggital |
16 |
15.2 |
|
||
|
olfactory groove |
12 |
11.4 |
|
||
|
sphenoid wing |
18 |
17.1 |
|
||
|
cavernous sinus |
3 |
2.9 |
|
||
|
not specified |
4 |
3.8 |
|
||
|
Total |
89 |
84.8 |
|
||
|
infratentorial |
tentorial |
2 |
1.9 |
|
0.000 |
|
clival |
2 |
1.9 |
|
||
|
cerebeo-pontine angle |
6 |
5.7 |
|
||
|
Total |
10 |
9.5 |
|
||
VIII Meningothelial Cell Tumors
A total of 105 intracranial meningiomas were observed, which represented 33.7% of all primary brain tumors. The age-standardized incidence rate of meningiomas was 0.101/100,000 person-years and was statistically higher in females (0.13/100,000) than in males (0.07/100,000) p=0.003), with a female: male ratio of 1.84 (p=0.003). Young adults were more often affected but the differences were not statistically significant. The age-standardized incidence rate of meningiomas in children was 0.007/100,000, which was lower than that in adults (0.12/100,000). The most common location was the convexity (28.6%) followed by the sphenoid wing (17.1%), parasagittal region (15.1%), and the olfactory groove (11.4%) (Table 17). Most meningothelial cell meningiomas were WHO grade I (91.8%) and the predominant histology type was meningothelial meningioma (34.1%) (Table 18).
Table 17: Histology type distribution of brain tumors of meningothelial cells.
|
histology type |
n |
% |
|
anaplastic meningioma |
5 |
5.9 |
|
atypical meningioma |
3 |
3.5 |
|
fibrous meningioma |
6 |
7.1 |
|
meningioma NOS |
22 |
25.9 |
|
Meningothelial meningioma |
29 |
34.1 |
|
metaplastic meningoma |
1 |
1.2 |
|
microscystic meinigioma |
5 |
5.9 |
|
psamomatous meningioma |
7 |
8.2 |
|
transitional meningioma |
7 |
8.2 |
Table 18: Tumors of sellar region.
|
Characteristics |
n |
% |
age-standardised incidence rate |
p value |
||
|
Gender |
female |
34 |
63.0 |
0.06 |
0.91 |
|
|
male |
20 |
37.0 |
0.04 |
|||
|
age category |
adult |
43 |
79.6 |
0.05 |
0.287 |
|
|
pediatric |
11 |
20.4 |
0.007 |
|||
|
Radiological diagnosis |
pituitary macroadenoma |
30 |
55.6 |
|
|
|
|
craniopharyngioma |
20 |
37.0 |
|
|||
|
invasive pituitary adenoma |
1 |
1.9 |
|
|||
|
suprasellar tumors NOS |
3 |
5.6 |
|
|||
|
Histology type |
Pituitary adenoma |
acidophilic pituitary adenoma |
1 |
|
|
0.000 |
|
basiohilic pituitary adenoma |
2 |
|
|
|||
|
infilitrating pituitary adanoma |
1 |
|
|
|||
|
pituitary adenoma |
3 |
|
|
|||
|
craniopharyngioma |
adamantinomatous craniopharyngioma |
5 |
|
|
||
|
craniopharyngioma NOS |
11 |
|
|
|||
IX Tumors of The Sellar Region
The 54 tumors of the sellar region comprised 16.4 % of all brain tumors. Adults and females were more frequently affected. The age-standardized incidence rate of seller region tumors (0.05/100,000) was seven times higher in adults than in children and was also higher in females (0.06/100,000) than in males. The most common radiological diagnoses were pituitary macroadenoma (55.6%) and craniopharyngioma (37%). Histological diagnosis was documented in 26 cases (48.14%), of which 16 (61.5%) were craniopharyngiomas and 10 (38.5) were pituitary adenoma (Table 18).
X Primary Spine Tumors
The 34 primary spine tumors comprised 7.3% of all CNS tumors and 44.7% of all spine tumors. The table 19 shows that there was the predominance of females (52.9%) among primary spine tumors patients was not statistically significant. Pediatric patients represented only 5.9% of primary spine tumors (p=1.09) (Table 19).
The thoracic spine was the most affected segment (42.4%), followed by the cervical and lumbar segments (21.2% of cases each) (p=0.000). The highest percentage of primary spine tumors were located in the intradural-extramedullary compartment (44.1%); the rest occurred in the vertebral body (29.4%) and extradural (8.8%) and intramedullary (5.9%) compartments (p=0.000). Meningothelial cell tumors, mesenchymal tumors, non-meningothelial tumors, and cranial and paraspinal nerve tumors comprised 29.4%, 26.5%, and 23.5% of primary spine tumors, respectively (Table 20). Primary spine tumors affected more patients in their fourth decade (30.7%), second (23.5%), third, and fifth decades (Figure 3).
Table 19: Primary spine Tumors demographic characteristics.
|
characteristics |
primary spine tumors |
p value |
||
|
n |
% |
|||
|
Gender |
female |
18 |
52.9 |
0.923 |
|
male |
16 |
47.1 |
||
|
age category |
adult |
32 |
94.1 |
0.109 |
|
pediatric |
2 |
5.9 |
||
|
age groups |
0-4 |
0 |
0.0 |
0.184 |
|
5-9 |
1 |
2.9 |
||
|
10-14 |
1 |
2.9 |
||
|
15-19 |
5 |
14.7 |
||
|
20-24 |
4 |
11.8 |
||
|
25-29 |
2 |
5.9 |
||
|
30-34 |
5 |
14.7 |
||
|
35-39 |
6 |
17.6 |
||
|
40-44 |
5 |
14.7 |
||
|
45-49 |
2 |
5.9 |
||
|
50-54 |
1 |
2.9 |
||
|
55-59 |
1 |
2.9 |
||
|
60-64 |
0 |
0.0 |
||
|
65-69 |
1 |
2.9 |
||
|
70-74 |
0 |
0.0 |
||
|
75-79 |
0 |
0.0 |
||
|
80-84 |
0 |
0.0 |
||
Table 20: Primary spine tumors location and category.
|
Characteristic |
n |
% |
p value |
||
|
location |
spine segment |
cervical |
7 |
21.2 |
0.000 |
|
thoracic |
14 |
42.4 |
|||
|
lumbar |
7 |
21.2 |
|||
|
all segments |
1 |
3.0 |
|||
|
not specified |
4 |
12.1 |
|||
|
Spine compartment |
vertebral body |
10 |
29.4 |
0.000 |
|
|
extradural |
3 |
8.8 |
|||
|
intradural-extramedullary |
15 |
44.1 |
|||
|
intramedullary |
2 |
5.9 |
|||
|
not specified |
4 |
11.8 |
|||
|
WHO CNS Tumor category |
Diffuse astrocytic and oligodendroglial |
2 |
5.9 |
0.000 |
|
|
Other astrocytic Tumor |
0 |
0.0 |
|||
|
Ependymal Tumors |
0 |
0.0 |
|||
|
Other gliomas |
0 |
0.0 |
|||
|
Embryonal Tumors |
1 |
2.9 |
|||
|
Tumors of cranial and paraspinal nerve |
8 |
23.5 |
|||
|
Tumors of meningothelial cells |
10 |
29.4 |
|||
|
Mesenchymal, non-meningothelial Tumors |
9 |
26.5 |
|||
|
Lymphomas |
4 |
11.8 |
|||
|
Germ cell Tumors |
0 |
0.0 |
|||
XI Metastatic Tumors
Among the 56 cases of CNS metastatic tumors, 21, 33, and 2 occurred in the brain, 33, and both brain and spine, respectively. Male and female patients were similarly affected (51.8% and 48.2%, respectively). Adults were significantly more frequently affected than children (98.2% versus 1.8%), p=0.003 (Table 21). The majority of metastatic brain tumors were located in the supratentorial compartment (47.6%, p=0.000). The lumbar region was the most frequent location of metastasis to the spine (36.4%), followed by the thoracic region (33.3%) (p=0.000) and lesions most frequently involved the vertebral bodies (Table 22).
Table 21: Metastatic CNS Tumors demographic characteristics.
|
characteristics |
brain metastatic tumor |
p value |
spine metastatic tumors |
p value |
|||
|
n |
% |
n |
% |
||||
|
Gender |
female |
11 |
52.4 |
0.982 |
16 |
48.5 |
0.662 |
|
male |
10 |
47.6 |
17 |
51.5 |
|||
|
age category |
adult |
20 |
95.2 |
|
33 |
100.0 |
0.011 |
|
pediatric |
1 |
4.8 |
0.165 |
0 |
0.0 |
||
Table 22: Location of CNS metastatic tumors.
|
Location |
brain metastatic tumor |
spine metastatic tumors |
||||||
|
|
n |
% |
p value |
n |
% |
p value |
||
|
|
intracranial |
supratentorial |
10 |
47.6 |
0.000 |
|
||
|
infratentorial |
2 |
9.5 |
||||||
|
infratentorial and supratentorial |
1 |
4.8 |
||||||
|
Not specified |
7 |
33.3 |
||||||
|
spinal segment |
cervical |
1 |
3.0 |
0.000 |
||||
|
Thoracic |
11 |
33.3 |
||||||
|
Lumbar |
12 |
36.4 |
||||||
|
All segments |
2 |
6.1 |
||||||
|
Not specified |
7 |
21.2 |
||||||
|
spine part |
vertebral body |
12 |
36.4 |
0.000 |
||||
|
Extradural |
0 |
0.0 |
||||||
|
intradural-extramedullary |
0 |
0.0 |
||||||
|
Intramedullary |
0 |
0.0 |
||||||
|
Not specified |
10 |
30.3 |
||||||
During the study period, 21 patients were diagnosed with metastatic brain tumors. Their mean age was 51.05 years and included 11 (52.4%) female and 10 male 10 (47.6%) patients. Histological diagnosis was documented for 11 patients, five (23.08%), one (4.76%), and two (9.5%) of which had primary tumors the lung, prostate, and melanoma. The tumor locations included the supratentorial (47.6%) and infratentorial (9.5 %) compartments (Tables 21 & 22). Among 33 patients with metastatic tumors, 51.5% were male and 48.5% were female. All were adult and their mean age was 58.5 years (p=0.011). The lumbar spine was the most frequently involved segment (36.3%), followed by the thoracic spine (33.3%); the cervical spine was the least involved segment (3.0%). The lesions were located in the vertebral body in 36.4% of cases. However, the location was not documented in 30% of patients with spinal metastatic tumors (Tables 21 & 22).
Discussion
Primary and secondary tumors of the central nervous system constitute a heterogeneous group of malignancies for which epidemiological data are derived from mortality and population-based cancer registries. The established cancer registries that collect data on CNS tumors include the Central Brain Tumor Registry of the United States (CBTRUS), which collects data on malignant and benign CNS tumors in the US; the National Brain Tumor Registry in the UK; and the French Brain Tumor Database (FBTD). Compared to the surveillance tools for other tumors, these CNS tumor registries are recent and provide heterogeneous data due to different policies and procedures for case acquisition. Despite the geographical and temporal discrepancies in the epidemiological data on CNS tumors, it is well established that the incidence rates have been increasing, mainly due to advances in diagnostic modalities and improved documentation of diagnosed cases [10].
The results of our study showed that the number of documented cases of CNS tumors increased dramatically from 2006 to 2015; in this time, health care insurance increased, the availability of CT scans and MRI increased, and documentation improved significantly in centers that diagnose and treat CNS tumors. The first objective of our study was to determine the incidence of CNS tumors in Rwanda between 2006 and 2015, which was 0.43/100,000 person-years. This incidence rate is much lower than the worldwide incidence of CNS tumors reported by the International Agency for Research on Cancer (3.8/100,000 persons in males and 3.1/100,000 persons in females; IARC 2008). The rates in this study were also lower than those in less developed countries (3.2/100,000 persons in males and 2.8/100,000 persons in females) reported by the same agency.
The low annual incidence rate of CNS tumors in our study may be a result of under diagnosis and poor documentation, as we observed an exponential increase in documented cases each year during the study period, which was marked by increased access to health care and imaging modalities (MRI and CT), as well as an increase in the of number of full-time permanent neurosurgeons in the two tertiary referral hospitals with neurosurgical services. The temporal increase in the incidence rates of CNS tumors in our study is consistent with data from other studies such as the French CNS registry, which reported a 2.3% annual increase in the incidence of CNS tumors in 2000-2007 [11].
The second specific objective of our study was to determine the sex and age distribution of CNS tumors in Rwanda. We found that both female and male patients were equally affected (0.43/100,000), a finding inconsistent with other published data that report a predominance of female patients [10]. In terms of age distribution, the median age at diagnosis in our study was 37 years (range: 5 months to 94 years). Another African country study on the epidemiology of CNS tumors reported an average patient age of 40 years [12]. The CBTRUS reported a median age at diagnosis of CNS tumors of 59 years. This discrepancy may be explained by the difference in general age structure between the US and countries in sub-Saharan Africa, including Rwanda. In our study the age-standardized annual incidence of CNS tumors increased with age, from 0.01/100,000 in those 0-4 years to 0.07 in those 34-39 years of age, then remaining consistent between the 4th and the 6th decades and around 0.03/100,000 69 years of age. The Gironde registry reported a similar trend but with higher incidence rates of CNS tumors among different age groups. In that study, the incidence rates in children were 4.3/100,000 in the first years of life and exceeded 10/100,000 after 40 years, 20/100,000 after 50 years, and 30/100,000 after 55 years of age [11].
The fourth specific objective of our study was to determine the histological types and grades of the CNS tumors. We found that meningothelial cell tumors were more common (0.101/100,000) than gliomas (0.095/100,000) and tumors of the sellar region (0.05/100,000). The incidence of meningiomas was higher in females than males (0.13/100,000 versus 0.07/100,000) (p=0.003). Diffuse astrocytic and oligodendroglial tumors occurred slightly more frequently in males (0.11/100,000) than in females (0.08/100,000) but the trend was not statistically significant (p=0.084). Our results are consistent with those of the CBTRUS, in which meningioma was the most common brain tumor before glioma (7.6 vs 6.5/100,000) [13]. They were also consistent with data from Korea reporting tumors of the meninges to be the most commonly reported tumors (31.2%) among 5,692 newly diagnosed CNS tumors in 2005, followed by neuroepithelial tumors (19.4%) [14].
In our study meningiomas occurred in 31.8% of cases, followed by diffuse astrocytic and oligodendroglial tumors (30%). The opposite pattern was observed in other registries like the Gironde Registry and the FBTD, which may a result of different race composition of these respective studies populations [15, 16]. As the incidence of meningiomas was statistically higher in blacks than that in whites, the higher incidence of meningiomas than gliomas could be explained by the racial composition of our study population as exclusively black. However, our results are similar to those of other studies results regarding the predominance of neuroepithelial tumors in males and meningothelial cells tumors in females [10].
Available data support the significant variation in the distribution of CNS tumor histology in different age groups. In France, neuroepithelial tumors represented 80% of all primary CNS tumors in children younger than 15 years old and 40.8% of those in adults aged between 25 and 64 years, with a proportion of meningiomas of 36.6% [11]. In the US, neuroepithelial tumors comprised 44.7% of primary CNS tumors in children younger than 15 years, compared to 15.7% for embryonal tumors in the same population [13]. In Korea, gliomas were also the most common of all pediatric primary CNS tumors (52.6%), followed by germ cell tumors (13.5%) [14]. Similarly, in the present study, neuroepithelial tumors were the most common CNS tumors in children (29%), followed by meningioma and tumors of the sellar region (18% each) and embryonal tumors (13%). In adults, meningothelial cell tumors were the most common (30.5%), followed by diffuse astrocytic and oligodendroglial tumors (24.38%) and metastatic tumors (16.18%).
In the present study, 259 (55.8%) of CNS tumors were histologically confirmed, compared to 58% in Korea, 73% in the US, 79.3% in France, and 86% in Japan [11, 13-15]. Thus, 44.2% of the final diagnoses in our cases were made without histological confirmation. Among the histologically confirmed cases, the most frequently reported histological types were meningothelial meningioma (11.8%) and glioblastoma multiforme (8.6%). Histological types comprising non-malignant meningiomas represented 33.9% of all histologically confirmed CNS tumors. This distribution is similar to that reported by the CBTRUS in which non-malignant meningiomas accounted for more than one-third of all tumors, followed by glioblastoma [13]. Similarly, glioblastomas comprised 9.6% of histologically confirmed CNS tumors in Korea [14].
In terms of the third specific objective of this study to determine the CNS tumor location, we found that 82.72% and 16.4% of CNS tumors were intracranial and spinal, respectively. The most frequent site of intracranial tumors was in the brain parenchyma (33.4%), followed by the suprasellar/parasellar region (9.6%). Similarly, in the US, 20.6% of primary brain tumors were located in the brain parenchyma. We observed a difference in the locations of brain tumors between adults and pediatric patients. The proportion of infratentorial tumors was higher in children than that in adults (42.3% versus 14.2%), while that for supratentorial tumors was higher in adults (69.2% versus 56.3%).
In our study, spine tumors comprised 16.4% of all CNS tumors, compared to only 7.1% in Iran [17]. A much lower percentage (3%) was also reported in the US [18]. The higher percentage of spine tumors in our study may be explained by our inclusion of metastatic tumors, unlike the Iranian and US studies. However, our results in terms of the pathological distribution of spine tumors were similar to those from Taiwan reporting metastasis, nerve sheath tumor, and meningioma rates of 45.3%, 28.2%, and 12%, respectively [19]. In Rwanda, metastasis comprised 49.3% of all spine tumors, followed by meningiomas (14.5%), nerve sheath tumors (11.9%) and mesenchymal, non-meningothelial tumors (13.4%).
In our study, spine tumors most commonly affected the thoracic spine (35.5%) and were extradural and intradural-extramedullary in 50% and 22.4% of spine tumors, respectively. Different percentages of spine tumor localization have been reported. For example, a retrospective study by Bhat et al. in Kashmir, India including 531 patients with spinal tumors treated surgically over 30 years from January 1983 to December 2014 reported intradural-extramedullary tumors in 68.73% of their study subjects, most commonly schwannoma [20]. However, when spinal metastatic tumors are included, extradural tumors are the most common spinal tumors as they are usually of metastatic origin [21].
Our study also included secondary CNS tumors. We found that brain metastasis was the fourth most frequent brain tumor after meningiomas, diffuse astrocytic and oligodendroglial tumors, and tumors of the seller region. Other studies reported metastatic tumors to be the most frequent brain tumor [22]. Our results likely reflect underdiagnosis of brain metastasis among cancer patients as it is not standard practice in our institutions to routinely perform neuroimaging for asymptomatic cancer and very sick cancer patients on palliative treatment. Among 10 brain metastatic tumors with histological confirmation, five originated from the lungs. Even if histological confirmation was obtained for the small proportion of metastatic brain tumors, our results were consistent with those of other studies reporting the lung as the origin of brain metastatic tumor in 40-50% of cases [22].
Conclusion
To our knowledge, this is the first study to report on the epidemiology CNS tumors in Rwanda. The results revealed an incidence of CNS tumors in Rwanda of 0.43/100,000 person-years, which increased from 0.01/100,000 in 2006 to 1.22/100,000 person-years in 2015. Moreover, meningothelial cell tumors were the most frequent CNS tumors followed by diffuse astrocytic and oligodendroglial tumors, while metastatic tumors were the most common spine tumors. We recommend establishing a CNS tumor registry to prospectively and systematically collect descriptive and survival epidemiologic data on CNS tumors to track the occurrence of these unique tumors and their impact on the national health system.
Abbreviations
CBTRUS: Central Brain Tumor Registry of the United States
CNS: Central Nervous System
CHUK: Centre Hospitalier Univeristaire de Kigali
CHUB: Centre Hospitalier Univeristaire de Butare
FBTD: French Brain Tumor Database
IARC: International Agency for research on cancer
IRB: Institutional Board Review
KFH: King Faisal Hospital
USA: United States of America
WHO: World Health Organization
Article Info
Article Type
Research ArticlePublication history
Received: Sat 02, May 2020Accepted: Fri 15, May 2020
Published: Fri 22, May 2020
Copyright
© 2023 David Hakizimana. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2020.02.11
Author Info
Agabe Emmy Nkusi David Hakizimana Eric Shingiro Paulin Munyemana Severien Muneza Steven Nshuti
Corresponding Author
David HakizimanaNeurosurgery Training Program, Department of Surgery, School of Medicine and Pharmacy, College of Medicine and health sciences, University of Rwanda, Rwanda
Figures & Tables
Table 1: Demographic characteristics.
|
Characteristics |
n |
% |
||
|
Socio demographics |
Sex |
Male |
223 |
47.85 |
|
female |
243 |
52.15 |
||
|
Age group |
pediatric <14 years) |
72 |
15.45 |
|
|
Adult |
394 |
84.55 |
||
|
CNS part involved |
BRAIN |
383 |
82.72 |
|
|
SPINE |
76 |
16.41 |
||
|
|
BRAIN AND SPINE |
4 |
0.86 |
|
Table 2: Age-group and gender specific incidence rates of CNS tumors.
|
Age groups |
male |
|
female |
|
Age standardised incidence rate |
|
|
|||
|
|
population size |
n |
average annual incidence (/100 000) |
population size |
n |
average annual incidence (/100,000) |
person-years at risk |
n |
WHO standard population |
Annual age standardised incidence rate (/100,000) |
|
0-4 |
815244 |
16 |
0.20 |
816355 |
9 |
0.11 |
16315992 |
25 |
8860 |
0.01 |
|
5-9 |
735332 |
16 |
0.22 |
736127 |
10 |
0.14 |
14714593 |
26 |
8690 |
0.02 |
|
10-14 |
619258 |
11 |
0.18 |
628950 |
10 |
0.16 |
12482078 |
21 |
8600 |
0.01 |
|
15-19 |
551430 |
17 |
0.31 |
563950 |
12 |
0.21 |
11153799 |
29 |
8470 |
0.02 |
|
20-24 |
522025 |
15 |
0.29 |
494595 |
8 |
0.16 |
10166195 |
23 |
8220 |
0.02 |
|
25-29 |
447497 |
24 |
0.54 |
486170 |
20 |
0.41 |
9336669 |
44 |
7930 |
0.04 |
|
30-34 |
324318 |
11 |
0.34 |
373770 |
19 |
0.51 |
6980885 |
30 |
7610 |
0.03 |
|
35-39 |
223797 |
23 |
1.03 |
274635 |
27 |
0.98 |
4984317 |
50 |
7150 |
0.07 |
|
40-44 |
177162 |
18 |
1.02 |
225474 |
23 |
1.02 |
4026359 |
41 |
6590 |
0.07 |
|
45-49 |
152985 |
13 |
0.85 |
201292 |
22 |
1.09 |
3542765 |
35 |
6040 |
0.06 |
|
50-54 |
124734 |
11 |
0.88 |
172905 |
15 |
0.87 |
2976384 |
26 |
5370 |
0.05 |
|
55-59 |
91838 |
11 |
1.20 |
131175 |
22 |
1.68 |
2230124 |
33 |
4550 |
0.07 |
|
60-64 |
67047 |
14 |
2.09 |
96459 |
7 |
0.73 |
1635058 |
21 |
3720 |
0.05 |
|
65-69 |
41590 |
3 |
0.72 |
64829 |
11 |
1.70 |
1064188 |
14 |
2960 |
0.04 |
|
70-74 |
31319 |
3 |
0.96 |
46154 |
6 |
1.30 |
774727 |
9 |
2210 |
0.03 |
|
75-79 |
23046 |
5 |
2.17 |
30484 |
4 |
1.31 |
535305 |
9 |
1520 |
0.03 |
|
80+ |
19358 |
4 |
2.07 |
25386 |
5 |
1.97 |
447436 |
9 |
1510 |
0.03 |
|
Total |
4967878 |
215 |
0.43 |
5368710 |
230 |
0.43 |
103840826 |
445 |
100000 |
0.43 |
Table 3: CNS tumors location.
|
|
BRAIN |
SPINE |
|||||
|
n |
% |
n |
% |
||||
|
cranial |
supratentorial |
Intraaxial |
hemispheric |
128 |
33.4 |
|
|
|
basal ganglia |
1 |
0.3 |
|||||
|
pineal |
2 |
0.5 |
|||||
|
ventricular |
2 |
0.5 |
|||||
|
extraaxial |
olfactory groove |
12 |
3.1 |
||||
|
sellar |
33 |
8.6 |
|||||
|
suprasellar/parasellar |
35 |
9.1 |
|||||
|
cavernous sinus |
3 |
0.8 |
|||||
|
sphenoid wing |
18 |
4.7 |
|||||
|
parasagittal |
16 |
4.2 |
|||||
|
|
not specified |
10 |
2.6 |
||||
|
ALL |
265 |
69.2 |
|||||
|
infratentorial |
Intraaxial |
cerebellar |
31 |
8.1 |
|||
|
brainstem |
10 |
2.6 |
|||||
|
4th ventricle |
6 |
1.6 |
|||||
|
|
extraaxial |
cerebello-pontine angle |
15 |
3.9 |
|||
|
tentorial |
1 |
0.3 |
|||||
|
clival |
2 |
0.5 |
|||||
|
NOS |
10 |
2.6 |
|||||
|
|
ALL |
75 |
19.6 |
||||
|
supratentorial and infratentorial |
2 |
0.5 |
|||||
|
not specified |
23 |
6.0 |
|||||
|
spinal |
spine segment |
cervical |
9 |
11.8 |
|||
|
thoracic |
27 |
35.5 |
|||||
|
lumbar |
19 |
25.0 |
|||||
|
all segments |
3 |
3.9 |
|||||
|
not specified |
21 |
27.6 |
|||||
|
Spine compartment |
extradural |
38 |
50.0 |
||||
|
intradural-extramedullary |
17 |
22.4 |
|||||
|
intramedullary |
4 |
5.3 |
|||||
|
not specified |
22 |
28.9 |
|||||
Table 4: Brain tumors location in adults and children(0-14 years).
|
Location site |
adult |
pediatric |
|||
|
n |
% |
n |
% |
||
|
supratentorial |
hemispheric |
112 |
30.5 |
18 |
25.4 |
|
sellar |
31 |
8.4 |
2 |
2.8 |
|
|
suprasellar/parasella |
19 |
5.2 |
16 |
22.5 |
|
|
pineal |
2 |
0.5 |
0 |
0.0 |
|
|
ventricular |
2 |
0.5 |
0 |
0.0 |
|
|
not specified |
39 |
10.6 |
3 |
4.2 |
|
|
parasaggital |
16 |
4.4 |
0 |
0.0 |
|
|
olfactory groove |
12 |
3.3 |
0 |
0.0 |
|
|
sphenoid wing |
17 |
4.6 |
1 |
1.4 |
|
|
cavernous sinus |
3 |
0.8 |
0 |
0.0 |
|
|
basal ganglia |
1 |
0.3 |
0 |
0.0 |
|
|
Total |
254 |
69.2 |
40 |
56.3 |
|
|
infratentorial |
cerebellar |
16 |
4.4 |
17 |
23.9 |
|
brainstem |
7 |
1.9 |
4 |
5.6 |
|
|
Cerebello-pontine ang |
16 |
4.4 |
1 |
1.4 |
|
|
fourth ventricle |
4 |
1.1 |
2 |
2.8 |
|
|
tentorial |
1 |
0.3 |
0 |
0.0 |
|
|
clival |
2 |
0.5 |
0 |
0.0 |
|
|
NOS |
6 |
1.6 |
6 |
8.5 |
|
|
Total |
52 |
14.2 |
30 |
42.3 |
|
|
Total |
|
367 |
|
71 |
|
Table 5: CNS tumors category.
|
CNS Tumor category |
brain |
spine |
Concomitant brain and spine |
||
|
n |
% |
n |
% |
n |
|
|
Diffuse astrocytic and oligodendroglial |
99 |
30.0 |
2 |
3.0 |
0 |
|
Other astrocytic tumor |
7 |
2.1 |
0 |
0.0 |
0 |
|
Ependymal tumors |
6 |
1.8 |
0 |
0.0 |
2 |
|
Other gliomas |
1 |
0.3 |
0 |
0.0 |
0 |
|
Choroid plexus tumors |
1 |
0.3 |
0 |
0.0 |
0 |
|
Embryonal tumors |
13 |
3.9 |
1 |
1.5 |
0 |
|
Tumors of cranial and paraspinal nerve |
3 |
0.9 |
8 |
11.9 |
0 |
|
Tumors of meningothelial cells |
105 |
31.8 |
10 |
14.9 |
0 |
|
Mesenchymal, non-meningothelial tumors |
14 |
4.2 |
9 |
13.4 |
0 |
|
Lymphomas |
5 |
1.5 |
4 |
6.0 |
0 |
|
Germ cell tumors |
1 |
0.3 |
0 |
0.0 |
0 |
|
Tumors of the sellar region |
54 |
16.4 |
_ |
_ |
_ |
|
metastatic tumors |
21 |
6.4 |
33 |
49.3 |
2 |
Table 6: Distribution of histology types of diffuse astrocytic and oligondroglial tumors, other astrocytic Tumors, ependymoma tumors and choroid plexus tumors.
|
Histology type |
n |
% |
|
Diffuse astrocytic and oligodendroglial tumors |
66 |
25.5 |
|
anaplastic oligoastrocytoma |
1 |
0.4 |
|
anaplastic oligodendroglioma |
1 |
0.4 |
|
astrocytoma NOS |
4 |
1.5 |
|
anaplastic astrocytoma |
8 |
3.1 |
|
diffuse astrocytoma |
23 |
8.9 |
|
glioblastoma multiforme |
23 |
8.9 |
|
high grade astrocytoma |
1 |
0.4 |
|
oligoastrocytoma |
2 |
0.8 |
|
oligodendroglioma |
3 |
1.2 |
|
other astrocytic tumors |
8 |
3.1 |
|
pilocystic astrocytoma |
7 |
2.7 |
|
pleomorphic xanthoastrocytoma |
1 |
0.4 |
|
Ependymal tumors |
7 |
2.7 |
|
anaplastic ependymoma |
1 |
0.4 |
|
ependymoma |
4 |
1.5 |
|
myxopapillary ependym |
1 |
0.4 |
|
papillary ependymoma |
1 |
0.4 |
|
Choroid plexus tumors |
1 |
0.4 |
|
Choroid plexus carcinoma |
1 |
0.4 |
Table 7: Histology types of meningothelial cells Tumors and mesenchymal non-meningothelial cells tumors.
|
Histology type |
n |
% |
|
Tumors of meningothelial cells |
95 |
36.7 |
|
anaplastic meningioma |
5 |
2 |
|
atypical meningioma |
3 |
1.2 |
|
clear cell meningioma |
1 |
0.4 |
|
fibrous meningioma |
8 |
3.1 |
|
meningioma NOS |
23 |
8.9 |
|
Meningothelial meningioma |
30 |
11.6 |
|
metaplastic meningoma |
1 |
0.4 |
|
microscystic meinigioma |
5 |
1.9 |
|
psamomatous meningioma |
10 |
3.9 |
|
transitional meningioma |
9 |
3.5 |
|
Mesenchymal, non-meningotheial cell Tumors |
20 |
7.7 |
|
chondrofibroma |
1 |
0.4 |
|
chondroma |
4 |
1.5 |
|
chondrosarcoma |
1 |
0.4 |
|
hemangioblastoma |
5 |
1.9 |
|
hemangioma |
2 |
0.8 |
|
lipoma |
1 |
0.4 |
|
osteoma |
4 |
1.5 |
|
sarcoma |
1 |
0.4 |
|
skull bone tumor |
1 |
0.4 |
Table 8: Histology types of Tumors of cranial and paraspinal tumors.
|
Histology type |
n |
% |
|
Plexiform neurofibroma |
1 |
0.4 |
|
biphasic schwannoma |
1 |
0.4 |
|
neurofibroma NOS |
2 |
0.8 |
|
schwannoma |
6 |
2.3 |
Table 9: Histology types of CNS lymphomas.
|
Histology type |
n |
% |
|
Lymphomas |
8 |
3.1 |
|
B cell lymphoma |
3 |
1.2 |
|
burkitt lymphoma |
3 |
1.2 |
|
hystiolytic lymphoma |
1 |
0.4 |
|
lymphoblastic lymphoma |
1 |
0.4 |
Table 10: Histology types of embryonal tumors and germ cell tumors.
|
Embryonal Tumors |
5 |
1.9 |
|
medullobastoma |
4 |
1.5 |
|
neuroectodermal Tumor |
1 |
0.4 |
|
Germ cell Tumors |
1 |
0.4 |
|
germinoma |
1 |
0.4 |
Table 11: Histology types of CNS metastatic tumors.
|
Histology type |
n |
% |
|
Metastatic Tumors |
15 |
5.8 |
|
adenocarcinoma NOS |
2 |
0.8 |
|
adenocarcinoma lung |
2 |
0.8 |
|
adenocarcinoma prostate |
1 |
0.4 |
|
carcinoma breast |
2 |
0.8 |
|
carcinoma from RCC |
1 |
0.4 |
|
lung SCC |
2 |
0.8 |
|
melanoma NOS |
3 |
1.2 |
|
metastatic bone Tumor NOS |
1 |
0.4 |
|
papillary carcinoma |
1 |
0.4 |
Table 12: Demographic characteristics of patients with primary brain tumors.
|
characteristics |
n |
% |
p value |
|
|
Gender |
female |
170 |
54.5 |
0.150 |
|
male |
142 |
45.5 |
||
|
age category |
adult |
253 |
81.1 |
0.003 |
|
paediatric |
59 |
18.9 |
||
|
Age group |
0-4 |
22 |
7.5 |
0.064 |
|
5-9 |
22 |
7.5 |
||
|
10-14 |
15 |
5.1 |
||
|
15-19 |
19 |
6.5 |
||
|
20-24 |
15 |
5.1 |
||
|
25-29 |
29 |
9.9 |
||
|
30-34 |
19 |
6.5 |
||
|
35-39 |
32 |
10.9 |
||
|
40-44 |
29 |
9.9 |
||
|
45-49 |
21 |
7.1 |
||
|
50-54 |
18 |
6.1 |
||
|
55-59 |
22 |
7.5 |
||
|
60-64 |
15 |
5.1 |
||
|
65-69 |
4 |
1.4 |
||
|
70-74 |
4 |
1.4 |
||
|
75-79 |
5 |
1.7 |
||
|
80+ |
3 |
1.0 |
||
Table 13: Primary brain tumors location.
|
Location |
n |
% |
P value |
||
|
supratentorial |
hemispheric |
107 |
45.9 |
0.000 |
|
|
basal ganglia |
1 |
0.4 |
|||
|
pineal |
2 |
0.9 |
|||
|
ventricular |
0 |
0.0 |
|||
|
olfactory groove |
12 |
5.2 |
|||
|
sellar |
32 |
13.7 |
|||
|
suprasellar/parasellar, |
31 |
13.3 |
|||
|
cavernous sinus |
3 |
1.3 |
|||
|
sphenoid wing |
18 |
7.7 |
|||
|
parasagittal |
16 |
6.9 |
|||
|
not specified |
11 |
4.7 |
|||
|
ALL |
233 |
74.7 |
|
||
|
infratentorial |
|
cerebellar |
30 |
44.1 |
0.010 |
|
brainstem |
9 |
13.2 |
|||
|
4th ventricle |
6 |
8.8 |
|||
|
|
|
cerebello-pontine angle |
14 |
20.6 |
|
|
tentorial |
1 |
1.5 |
|||
|
clival |
2 |
2.9 |
|||
|
NOS |
6 |
8.8 |
|||
|
|
ALL |
68 |
21.8 |
|
|
|
supratentorial and infratentorial |
|
1 |
|
|
|
|
not specified |
|
10 |
|
|
|
Table 14: Primary brain tumors categories according to 2016 WHO CNS tumors classification.
|
WHO CNS Tumor category |
n |
% |
P value |
|
Diffuse astrocytic and oligodendroglial |
99 |
31.7 |
0.000 |
|
Other astrocytic tumor |
7 |
2.2 |
|
|
Ependymal tumors |
8 |
2.6 |
|
|
Other gliomas |
1 |
0.3 |
|
|
Choroid plexus tumors |
1 |
0.3 |
|
|
Embryonal tumors |
13 |
4.2 |
|
|
Tumors of cranial and paraspinal nerve |
3 |
1.0 |
|
|
Tumors of meningothelial cells |
105 |
33.7 |
|
|
Mesenchymal, non-meningothelial tumors |
14 |
4.5 |
|
|
Lymphomas |
6 |
1.9 |
|
|
Germ cell tumors |
1 |
0.3 |
|
|
Tumors of the sellar region |
54 |
17.3 |
Table 15: Diffuse astrocytic and oligodendroglial tumors.
|
characteristics |
|
diffuse astrocytic and oligodendroglial tumors |
|
p value |
|
|
|
|
n |
% |
age-standardised incidence rate |
|
|
Gender |
female |
44 |
44.4 |
0.08 |
0.084 |
|
male |
55 |
55.5 |
0.11 |
||
|
age category |
adult |
81 |
81.8 |
0.1 |
0.397 |
|
pediatric |
18 |
18.2 |
0.011 |
||
|
location |
supratentorial |
72 |
72.7 |
|
0.000 |
|
infratentorial |
22 |
22.2 |
|
||
|
not specified |
4 |
4.0 |
|
||
|
histology type |
anaplastic oligoastrocytoma |
1 |
1.5 |
|
0.000 |
|
anaplastic oligodendroglioma |
1 |
1.5 |
|
||
|
astrocytoma NOS |
4 |
6.1 |
|
||
|
anaplastic astrocytoma |
8 |
12.1 |
|
||
|
diffuse astrocytoma |
23 |
34.8 |
|
||
|
glioblastoma multiforme |
23 |
34.8 |
|
||
|
high grade astrocytoma |
1 |
1.5 |
|
||
|
oligoastrocytoma |
2 |
3.0 |
|
||
|
oligodendroglioma |
3 |
4.5 |
|
||
|
tumor grade |
II |
27 |
40.9 |
|
0.000 |
|
III |
13 |
19.7 |
|
||
|
IV |
26 |
39.4 |
|
||
Table 16: Tumors of meningothelial cells: demographic characteristics and location.
|
characteristics |
n |
% |
Incidence rate |
p value |
|
|
female |
68 |
64.8 |
0.13 |
0.003 |
|
|
male |
37 |
35.2 |
0.07 |
||
|
adult |
|
94 |
89.5 |
0.12 |
0.109 |
|
pediatric |
|
11 |
10.5 |
0.007 |
|
|
supratentorial |
convexity |
30 |
28.6 |
|
0.000 |
|
suprasellar/parasellar |
6 |
5.7 |
|
||
|
parasaggital |
16 |
15.2 |
|
||
|
olfactory groove |
12 |
11.4 |
|
||
|
sphenoid wing |
18 |
17.1 |
|
||
|
cavernous sinus |
3 |
2.9 |
|
||
|
not specified |
4 |
3.8 |
|
||
|
Total |
89 |
84.8 |
|
||
|
infratentorial |
tentorial |
2 |
1.9 |
|
0.000 |
|
clival |
2 |
1.9 |
|
||
|
cerebeo-pontine angle |
6 |
5.7 |
|
||
|
Total |
10 |
9.5 |
|
||
Table 17: Histology type distribution of brain tumors of meningothelial cells.
|
histology type |
n |
% |
|
anaplastic meningioma |
5 |
5.9 |
|
atypical meningioma |
3 |
3.5 |
|
fibrous meningioma |
6 |
7.1 |
|
meningioma NOS |
22 |
25.9 |
|
Meningothelial meningioma |
29 |
34.1 |
|
metaplastic meningoma |
1 |
1.2 |
|
microscystic meinigioma |
5 |
5.9 |
|
psamomatous meningioma |
7 |
8.2 |
|
transitional meningioma |
7 |
8.2 |
Table 18: Tumors of sellar region.
|
Characteristics |
n |
% |
age-standardised incidence rate |
p value |
||
|
Gender |
female |
34 |
63.0 |
0.06 |
0.91 |
|
|
male |
20 |
37.0 |
0.04 |
|||
|
age category |
adult |
43 |
79.6 |
0.05 |
0.287 |
|
|
pediatric |
11 |
20.4 |
0.007 |
|||
|
Radiological diagnosis |
pituitary macroadenoma |
30 |
55.6 |
|
|
|
|
craniopharyngioma |
20 |
37.0 |
|
|||
|
invasive pituitary adenoma |
1 |
1.9 |
|
|||
|
suprasellar tumors NOS |
3 |
5.6 |
|
|||
|
Histology type |
Pituitary adenoma |
acidophilic pituitary adenoma |
1 |
|
|
0.000 |
|
basiohilic pituitary adenoma |
2 |
|
|
|||
|
infilitrating pituitary adanoma |
1 |
|
|
|||
|
pituitary adenoma |
3 |
|
|
|||
|
craniopharyngioma |
adamantinomatous craniopharyngioma |
5 |
|
|
||
|
craniopharyngioma NOS |
11 |
|
|
|||
Table 19: Primary spine Tumors demographic characteristics.
|
characteristics |
primary spine tumors |
p value |
||
|
n |
% |
|||
|
Gender |
female |
18 |
52.9 |
0.923 |
|
male |
16 |
47.1 |
||
|
age category |
adult |
32 |
94.1 |
0.109 |
|
pediatric |
2 |
5.9 |
||
|
age groups |
0-4 |
0 |
0.0 |
0.184 |
|
5-9 |
1 |
2.9 |
||
|
10-14 |
1 |
2.9 |
||
|
15-19 |
5 |
14.7 |
||
|
20-24 |
4 |
11.8 |
||
|
25-29 |
2 |
5.9 |
||
|
30-34 |
5 |
14.7 |
||
|
35-39 |
6 |
17.6 |
||
|
40-44 |
5 |
14.7 |
||
|
45-49 |
2 |
5.9 |
||
|
50-54 |
1 |
2.9 |
||
|
55-59 |
1 |
2.9 |
||
|
60-64 |
0 |
0.0 |
||
|
65-69 |
1 |
2.9 |
||
|
70-74 |
0 |
0.0 |
||
|
75-79 |
0 |
0.0 |
||
|
80-84 |
0 |
0.0 |
||
Table 20: Primary spine tumors location and category.
|
Characteristic |
n |
% |
p value |
||
|
location |
spine segment |
cervical |
7 |
21.2 |
0.000 |
|
thoracic |
14 |
42.4 |
|||
|
lumbar |
7 |
21.2 |
|||
|
all segments |
1 |
3.0 |
|||
|
not specified |
4 |
12.1 |
|||
|
Spine compartment |
vertebral body |
10 |
29.4 |
0.000 |
|
|
extradural |
3 |
8.8 |
|||
|
intradural-extramedullary |
15 |
44.1 |
|||
|
intramedullary |
2 |
5.9 |
|||
|
not specified |
4 |
11.8 |
|||
|
WHO CNS Tumor category |
Diffuse astrocytic and oligodendroglial |
2 |
5.9 |
0.000 |
|
|
Other astrocytic Tumor |
0 |
0.0 |
|||
|
Ependymal Tumors |
0 |
0.0 |
|||
|
Other gliomas |
0 |
0.0 |
|||
|
Embryonal Tumors |
1 |
2.9 |
|||
|
Tumors of cranial and paraspinal nerve |
8 |
23.5 |
|||
|
Tumors of meningothelial cells |
10 |
29.4 |
|||
|
Mesenchymal, non-meningothelial Tumors |
9 |
26.5 |
|||
|
Lymphomas |
4 |
11.8 |
|||
|
Germ cell Tumors |
0 |
0.0 |
|||
Table 21: Metastatic CNS Tumors demographic characteristics.
|
characteristics |
brain metastatic tumor |
p value |
spine metastatic tumors |
p value |
|||
|
n |
% |
n |
% |
||||
|
Gender |
female |
11 |
52.4 |
0.982 |
16 |
48.5 |
0.662 |
|
male |
10 |
47.6 |
17 |
51.5 |
|||
|
age category |
adult |
20 |
95.2 |
|
33 |
100.0 |
0.011 |
|
pediatric |
1 |
4.8 |
0.165 |
0 |
0.0 |
||
Table 22: Location of CNS metastatic tumors.
|
Location |
brain metastatic tumor |
spine metastatic tumors |
||||||
|
|
n |
% |
p value |
n |
% |
p value |
||
|
|
intracranial |
supratentorial |
10 |
47.6 |
0.000 |
|
||
|
infratentorial |
2 |
9.5 |
||||||
|
infratentorial and supratentorial |
1 |
4.8 |
||||||
|
Not specified |
7 |
33.3 |
||||||
|
spinal segment |
cervical |
1 |
3.0 |
0.000 |
||||
|
Thoracic |
11 |
33.3 |
||||||
|
Lumbar |
12 |
36.4 |
||||||
|
All segments |
2 |
6.1 |
||||||
|
Not specified |
7 |
21.2 |
||||||
|
spine part |
vertebral body |
12 |
36.4 |
0.000 |
||||
|
Extradural |
0 |
0.0 |
||||||
|
intradural-extramedullary |
0 |
0.0 |
||||||
|
Intramedullary |
0 |
0.0 |
||||||
|
Not specified |
10 |
30.3 |
||||||
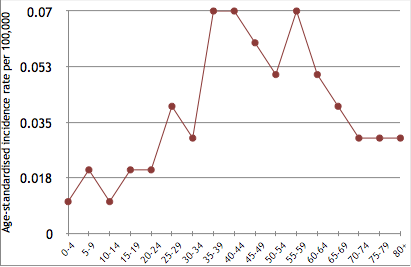
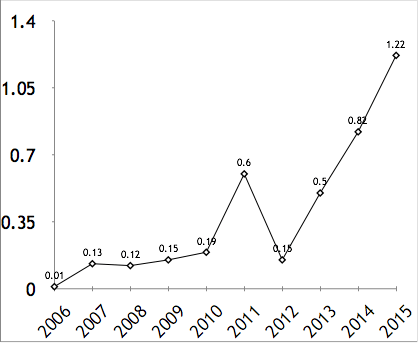
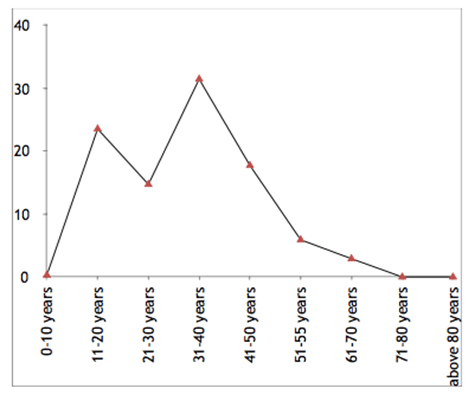
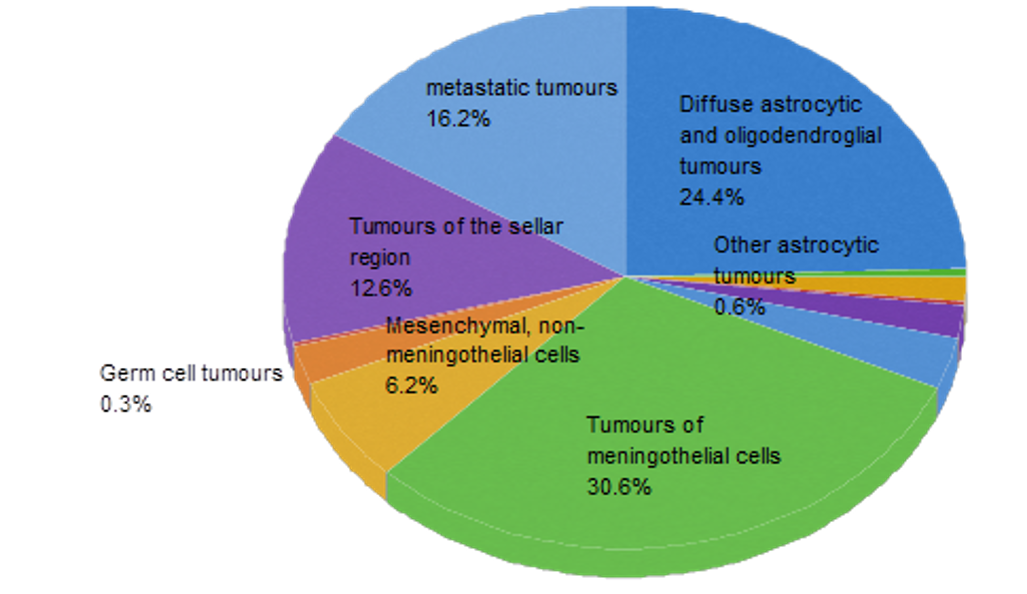
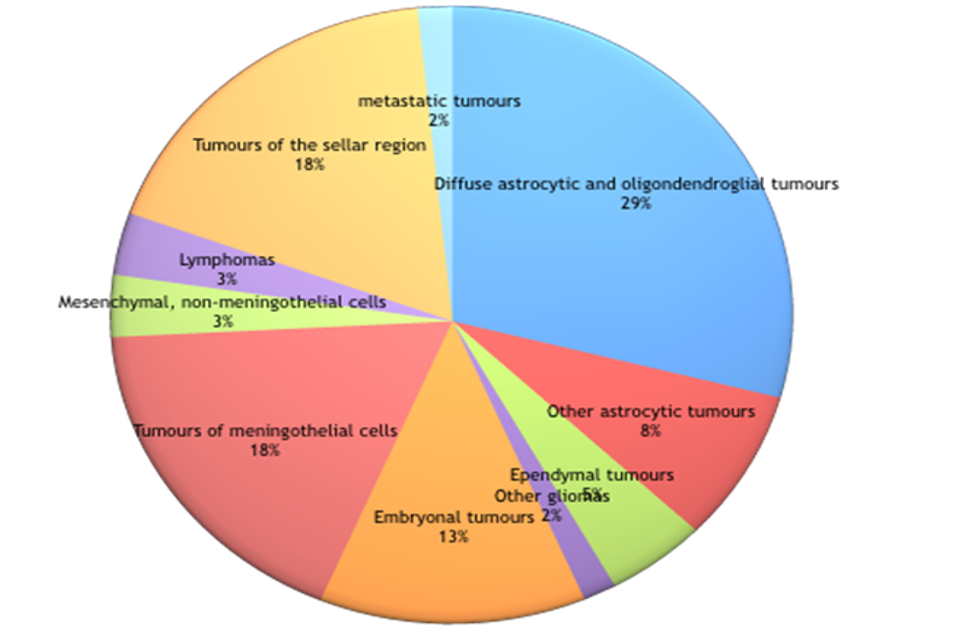
References
- Kleihues P, Burger PC, Scheithauer BW (1993)The new WHO classification of brain tumors. Brain Pathol 3: 255-268. [Crossref]
- David N Louis, Hiroko Ohgaki, Otmar D Wiestler,Webster K Cavenee (2007) WHO Classification of Tumors of the Central Nervous System. Lyon : International Agency for Research on Cancer.
- Jemal A, Murray T, Ward E, Samuels A, Tiwari RC et al. (2005) Cancer statistics. CA Cancer J Clin 55: 10-30. [Crossref]
- Donthineni R (2009) Diagnosis and staging of the spine tumors. Orthop Clin N Am 40: 1-7. [Crossref]
- Gasbarrini A, Cappuccio M, Mirabile L, Bandiera S, Terzi S et al. (2004) Spinal metastases: treatment evaluation algorithm. Eur Rev Med Pharmacol Sci 8: 265-274. [Crossref]
- Hatef J, Adamson C, Obiga O, Taremwa B, Ssenyojo H et al. (2014) Central nervous system tumour distribution at a tertiary Referral Center in Uganda. World Neurosurg 82: 258-265. [Crossref]
- Stagno V, Mugamba J, Ssenyonga P, Kaaya BN, Warf BC (2014) Presenttion, pathology, and treatment outcome in 172 cosnecutice Children at CURE Children,s hopsital of Uganda. The predominance of the visible diagnosis and the uncertainities of epidemiology in sub-saharan Africa. Childs Nerv Syst 30: 137-146. [Crossref]
- Mwang'Ombe NJ, Ombachi RB (2000) Brain tumors at the Kenyatta National Hospital, Nairobi. East Afr Med J 77: 444-447. [Crossref]
- Mwang'Ombe NJ, Ouma MB (2000) spinal cord compression due to tumors at Kenyatta National Hospital, Nairobi. East Afr Med J 77: 374-376. [Crossref]
- Pouchieu C, Baldi I, Gruber A, Berteaud E, Carles C et al. (2016) Descriptive epidemiology and risk factors of primary central nervous system tumors: Current knowledge. Rev Neurol (Paris) 172: 46-55. [Crossref]
- Baldi I, Gruber A, Alioum A, Berteaud E, Lebailly P et al. (2011) Descriptive epidemiology of CNS tumors in France: results from the Gironde Registry for the period 2000-2007. Neuro Oncol 13: 1370-1378. [Crossref]
- Victor-Claude Eyenga, Joseph Eloundou Ngah, Rene Atangana, Empime Etom, Marcellin Ngowe Ngowe et al. (2008) Les tumeurs du systeme nerveux central au Cameroun: histologie, demographie. Cahiers de Sante 18: 1.
- Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y et al. (2013) CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2006-2010. Neuro Oncol 15: 1-56. [Crossref]
- Lee CH, Jung KW, Yoo H, Park S, Lee SH (2013) Epidemiology of Primary Brain and Central Nervous System Tumors in Korea. J Korean Neurosurg Soc 48: 145-152. [Crossref]
- Registre des tumeurs du syste`me nerveux central de la Gironde (2015) General register of cancers of the Gironde. Institut of public health, epidemiology and development, University of Bordeaux Segalen.
- Zouaoui S, Darlix A, Rigau V, Mathieu-Daudé H, Bauchet F et al. (2015) Descriptive epidemiology of 13,038 newly diagnosed and histologically confirmed meningiomas in France: 2006-010. Neurochirurgie 64: 15-21. [Crossref]
- Jazayeri SB, Rahimi-Movaghar V, Shokraneh F, Saadat S, Ramezani R (2013) Epidemiology of Primary CNS Tumors in Iran: A Systematic Review. Asian Pacific J Cancer Prev 14: 3979-3985. [Crossref]
- Dolecek TA, Propp JM, Stroup NE, Kruchko C (2012) Cbtrus statistical report: Primary brain and central nervous system tumors diagnosed in the united states in 2005-2009. Neuro Oncol 14: v1-v49. [Crossref]
- Cheang CM, Hwang SL, Hwong SL (1997) An analysis of intraspinal tumors in south Taiwan. Kaohsiung J Med Sci 13: 229-236. [Crossref]
- Bhat AR, Kirmani AR, Wani MA, Bhat MH (2016) Incidence, histopathology, and surgical outcome of tumors of spinal cord, nerve roots, meninges, and vertebral column - Data based on single institutional (Sher-i-Kashmir Institute of Medical Sciences) experience. J Neurosci Rural Pract 7: 381-391. [Crossref]
- Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG (2015) Intramedullary Spinal Cord Tumors: Part I—Epidemiology, Pathophysiology, and Diagnosis. Global Spine J 5: 425-435. [Crossref]
- Eichler AF, Chung E, Kodack DP, Loeffler JS, Fukumura D et al. (2011) The biology of brain metastases-translation to new therapies. Nat Rev Clin Oncol 8: 344-356. [Crossref]
