Effects of Desflurane Versus Propofol Anesthesia on Regional Cerebral Oxygenation during Spinal Surgery in the Prone Position
A B S T R A C T
Context: Postural change during anaesthesia has a complex effect on systemic and cerebral circulations.
Aim: The goal of the study was to evaluate the effects of desflurane and propofol on cerebral oxygenation during spinal surgery in the prone position.
Settings and Design: A prospective randomized double-blinded trial.
Methods and Materials: Fifty-two patients scheduled for spinal surgery were randomly allocated to propofol (n=25) and desflurane (n=27) groups. Anaesthetic agents were maintained to obtain a bispectral index of 50-55. SAP, DAP, HR, SPO2, ETCO2 and right and left rSO2 were assessed at seven-time points: supine position without oxygen administration (T1), supine position with oxygen administration (T2-baseline), intubation in the supine position (T3), just after prone positioning (T4), 10 minutes after prone positioning (T5), at the end of surgery in the prone position (T6) and at the end of anaesthesia in the supine position (T7). PCO2, PO2 and Hb partial were also recorded at T3 and T7.
Results: Demographic data, pre-oxygenation hemodynamic variables and rSO2 were comparable between the groups. There was no significant difference between groups in SAP, DAP, HR, SPO2, and ETCO2 (p=0.095, p=0.061, p=0.357, p=0.088, p=0.328 respectively). PCO2, PO2 and Hb were not significant different between groups (p=0.542, p=0.394, p=0.768 respectively). rSO2 values were not significantly different between groups. In the propofol group, right rSO2 was significantly higher at T3 (p=0.017) and significantly lower at T5 (p=0,019) and at T6 (p=0,028) compared to baseline. Left rSO2 decreased significantly from baseline at T5 (p=0.026) in the propofol group. Left and right rSO2 in the desflurane group decreased significantly from baseline at T5 (p=0.0004 and p=0.0115).
Conclusion: In the prone position, desflurane and propofol were associated with a significant decrease in rSO2 without differences between these anaesthetics.
Keywords
Cerebral oxygenation, prone position, desflurane, propofol
Key Messages
Desflurane and propofol affect cerebral oxygenation in the same way during spinal surgery in the prone position.
Introduction
The prone position is commonly utilized for procedures requiring the posterior approach to the spine [1]. However, this position may cause significant hemodynamic instability and cerebral hypoperfusion. Several perioperative complications such as brain ischaemia, spinal cord injury and visual loss after the prone position have been reported [2]. Though most of these complications are rare, familiarity with strategies for prevention can limit morbidity in prone spine surgery. Desflurane or propofol-remifentanil-based anaesthetic regimens represent modern techniques for neurosurgical anaesthesia. Nevertheless, there are potential differences related to their activity on the cerebrovascular system. The magnitude of such difference is not completely known [3].
Studies in human subjects indicate that propofol affects reductions in the cerebral metabolic rate and secondarily decreases cerebral blood flow and intracranial pressure [4]. Autoregulation and CO2 responsiveness are preserved in humans during the administration of propofol and the magnitude of reduction in cerebral blood flow during hypocapnia is decreased during propofol administration [5]. On the other hand, desflurane can significantly reduce cerebral blood flow in humans when compared with cerebral blood flow in awake, non-anaesthetized patients. At 1 MAC concentrations, desflurane decreased cerebral blood flow by 22% and cerebral metabolic rate by 35% [6]. We hypothesized that both desflurane and propofol would decrease the rSO2 when patients turned to the prone position. Therefore, the aim of the present study was to investigate the differences between desflurane and propofol on reducing regional cerebral oxygenation (rSO2) in the prone position for spinal surgery.
Subjects and Methods
The study was approved by the Ethical Committee of General Hospital of Thessaloniki “G. Papanikolaou” (protocol number: 21/4-1-2017) (Trial registration: European Network of Centres for Pharmacoepidemiology and Pharmacovigilance identifier: EU PAS 16641). A thorough pre-anaesthetic evaluation was done and patients with morbid obesity, allergy to study drugs, severe cerebrovascular or cardiovascular disease were excluded from the study. We informed all the patients about the study and written informed consent was obtained before the procedure.
Fifty-two patients with the American Society of Anesthesiologists (ASA) physical status I/II, scheduled for spinal surgery, were enrolled in a prospective randomized double-blinded trial. The randomization was achieved by a random number table using a sealed envelope technique. Patients were divided into two groups: propofol group (n=25) and desflurane group (n=27). Oral diazepam (5mg) was administered an hour before surgery for premedication. All patients were monitored with electrocardiogram, invasive blood pressure and pulse oximetry. The basal crystalloid infusion was started at 4 ml/kg/h right after peripheral intravenous access. After cleansing the skin of the patient’s forehead with an alcohol pad, sensors of BIS monitoring (BISTM complete-2 channel monitor, Covidien, Medtronic) and INVOS monitoring (INVOSTM 5100C Cerebral/somatic oximeter, Medtronic) were attached.
Propofol (2mg/kg), fentanyl (2mcg/kg) and rocuronium 0.6 mg/kg were administrated for anaesthesia induction. After the tracheal intubation, the ventilator was set to a tidal volume of 8ml/kg and a respiratory rate of 8-12 breaths/min to adjust an end-tidal carbon dioxide concentration (ETCO2) of 32-38 mmHg at a 50% inspired oxygen with air. Anaesthetic agents were maintained and adjusted with the effect-site concentration of propofol 2-3.5 lg/ml in the propofol group and desflurane 4-7 vol% in the desflurane group to obtain the bispectral index of 50-55. The incidence of hypotension was recorded and corrected with ephedrine 5mg. SAP, DAP, HR, SPO2, ETCO2 and right and left rSO2 were assessed at seven-time points: supine position without oxygen administration (T1), supine position with oxygen administration (T2-baseline), intubation in the supine position (T3), just after prone positioning (T4), 10 minutes after prone positioning (T5), at the end of surgery in the prone position (T6) and at the end of anaesthesia in the supine position (T7). Partial pressure of carbon dioxide, partial pressure of oxygen and haemoglobin were also recorded at T3 and T7. Partial pressure of carbon dioxide, partial pressure of oxygen and haemoglobin were also recorded at T3 and T7 time points.
Statistical Analysis
A sample size of 52 patients in each group was estimated for a type 1 error of 0.05 (α= 0.05) and a power of 80%. The data were expressed as mean ± standard deviation. Age and BMI data were compared between the two groups by Student’s t-test (2-tailed). Weight, height and Aldrete score data were compared among the two groups using the Mann-Whitney-U-test (2-tailed). Sex and ASA physical status were compared using the Chi-Square test. SAP, DAP, HR, SPO2, ABGs, left and right rSO2 data were compared among the two groups using the Two-Way Mixed ANOVA test. Statistical Package for Social Sciences (SPSS, version 19.0; SPSS Inc., Chicago, IL, USA) was used for all calculations. P values less than 0.05 were considered significant.
Results
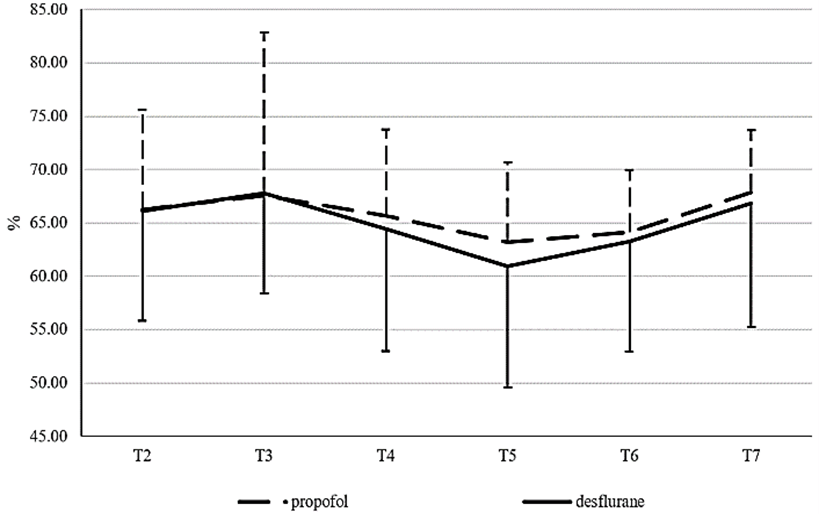
There were no significant differences between the two groups in demographic data and clinical characteristics. Pre-induction hemodynamic variables and left and right rSO2 were similar between groups (Table 1). There was not significantly difference between groups in SAP, DAP, HR, SPO2, and ETCO2 (p=0.095, p=0.061, p=0.357, p=0.088, p=0.328 respectively) (Table 2). PCO2, PO2 and Hb were no significant different between groups (p=0.542, p=0.394, p=0.768 respectively) (Table 3). Right (Figure 1) and left (Figure 2) rSO2 values were not significantly different between groups (right rSO2: p=0.357 (T2), p=0.275 (T3), p=0.657 (T4), p=0.611 (T5), p=0.536 (T6), p=0.853 (T7), left rSo2: p=0.958 (T2), p=0.954 (T3), p=0.646 (T4), p=0.397 (T5), p=0.709 (T6), p=0.689 (T7) (Table 4). In propofol group right rSO2 was significantly lower at T5 (62.22 ± 6.33 vs 66 ± 8.87, p=0,019) and at T6 (63.07 ± 5 vs 66 ± 8.87, p=0,028) compared to baseline. Moreover, in propofol group left rSO2 decreased significantly from baseline at T5 (63.19 ± 7.56 vs 66.22 ± 9.39, p=0.026) and at T6 (64,15 ± 5,84 vs 66.22 ± 9.39, p=0.041). In desflurane group right and left rSO2 decreased significant from baseline only at T5 (60.96 ± 11.02 vs 63.68 ± 9.14, p=0.0115 and 60.92 ± 11.32 vs 66.08 ± 10.21, p=0.0004) (Table 5).
Table 1: Demographic and clinical characteristics of study
patients.
|
Variable |
|
group propofol |
group desflurane |
P |
|
Age |
Years |
57 ± 11,13 |
55,8 ± 15,1 |
0,744a |
|
Height |
Cm |
74,48 ± 12,43 |
79,28 ± 12,31 |
0,601b |
|
Weight |
Kg |
166,15 ± 7,63 |
167,96 ± 8,2 |
0,502b |
|
BMI |
Kg/m2 |
27,19 ± 4,47 |
29,4 ± 3,01 |
0,063a |
|
Gender |
Male |
8 (29,63%) |
12 (48,00%) |
0,174c |
|
Female |
19 (70,37%) |
13 (52,00%) |
||
|
ASA |
1 |
3 (11,11%) |
3 (12,00%) |
0,980c |
|
2 |
18 (66,67%) |
16 (64,00%) |
||
|
3 |
6 (22,22%) |
6 (24,00%) |
||
|
Pre- induction hemodynamics SAP |
mmHg |
142,04 ± 19,79 |
148,92 ± 20,74 |
0,226a |
|
DAP |
mmHg |
82,48 ± 11,79 |
79,8 ± 11,1 |
0,403a |
|
HR |
beats/min |
75,63 ± 14,7 |
78,28 ± 13,56 |
0,503a |
|
SPO2 |
% |
95,3 ± 1,88 |
96,76 ± 2,74 |
0,056b |
|
Pre- induction rSO2 Right rSO2 |
% |
63,33 ± 7,42 |
61,36 ± 9,72 |
0,421a |
|
Left rSO2 |
% |
64,44 ± 7,7 |
62,84 ± 9,39 |
0,502a |
a:
Based on t-test, b: based on M-W test, c: based on Chi-Square test. Data are
presented as mean ± standard deviation or number (proportion, %)
BMI:
Body Mass Index; ASA: American Society of Anesthesiologist.
Table 2: Hemodynamic and end-tidal carbon dioxide tension
changes during prone position.
|
Index |
Group |
T2 |
T3 |
T4 |
T5 |
T6 |
T7 |
P |
|
SAP |
Propofol |
145,78 ± 22,38 |
112,3 ± 18,84 |
111,93 ± 20,66 |
114,63 ± 12,77 |
116,63 ± 15,18 |
121,48 ± 16,29 |
0,095 |
|
Desflurane |
148,2 ± 19,06 |
120,76 ± 21,65 |
104,84 ± 15,1 |
113,96 ± 17,87 |
109,28 ± 16,79 |
117,76 ± 17,57 |
||
|
DAP |
Propofol |
70,63 ± 11,82 |
64,07 ± 13,81 |
64,15 ± 9,93 |
68 ± 8,64 |
65,33 ± 8,35 |
64,74 ± 8,27 |
0,061 |
|
Desflurane |
70,28 ± 10,11 |
67,72 ± 11,96 |
58,6 ± 10,56 |
60,6 ± 7,42 |
58,84 ± 7,26 |
67,28 ± 9,07 |
||
|
HR |
Propofol |
73,52 ± 13,72 |
72,37 ± 12,53 |
66,48 ± 10,68 |
64,07 ± 11,23 |
62,15 ± 8,54 |
65,59 ± 13,1 |
0,357 |
|
Desflurane |
76,84 ± 13,76 |
79,4 ± 17,17 |
70,28 ± 13,95 |
65,16 ± 11,51 |
61,72 ± 7,13 |
68,44 ± 9,63 |
||
|
SPO2 |
Propofol |
98,37 ± 1,57 |
98,96 ± 1,02 |
98,52 ± 1,05 |
98,59 ± 1,22 |
98,96 ± 1,06 |
99,26 ± 0,86 |
0,088 |
|
Desflurane |
99,36 ± 0,64 |
99,08 ± 0,86 |
98,64 ± 0,76 |
98,76 ± 0,72 |
98,96 ± 0,73 |
99,16 ± 0,69 |
||
|
ETCO2 |
Propofol |
|
30,44 ± 3,25 |
30,78 ± 2,9 |
29,59 ± 2,26 |
31,22 ± 2,68 |
32,63 ± 2,99 |
0,328 |
|
Desflurane |
|
31,88 ± 4,72 |
31,24 ± 3,39 |
31,76 ± 2,59 |
32,44 ± 2,84 |
33,24 ± 2,77 |
Two-Way Mixed ANOVA.
Table 3: ABGs changes during prone positioning.
|
Index |
Group |
T3 |
T7 |
P |
|
PO2 |
Propofol |
272,96 ± 102,1 |
249,41 ± 74,89 |
0,542 |
|
Desflurane |
250,36 ± 98,99 |
246,48 ± 84,05 |
||
|
PCO2 |
Propofol |
36,3 ± 3,78 |
37,98 ± 3,56 |
0,394 |
|
Desflurane |
37,94 ± 3,83 |
38,52 ± 3,65 |
||
|
Hb |
Propofol |
12,36 ± 1,46 |
11,5 ± 1,51 |
0,768 |
|
Desflurane |
12,7 ± 1,49 |
11,94 ± 1,79 |
Two-Way Mixed ANOVA.
Table 4: INVOS data during the procedure between groups.
|
Index |
Group |
T2 |
P |
T3 |
P |
T4 |
P |
|
Right rSO2 |
Propofol |
66 ± 8,87 |
0,357 |
68,7 ± 9,41 |
0,275 |
64,33 ± 7,09 |
0,657 |
|
Desflurane |
63,68 ± 9,14 |
65,64 ± 10,59 |
63,16 ± 11,51 |
||||
|
Left rSO2 |
Propofol |
66,22 ± 9,39 |
0,958 |
67,59 ± 15,27 |
0,954 |
65,7 ± 8,03 |
0,646 |
|
Desflurane |
66,08 ± 10,21 |
67,8 ± 9,45 |
64,44 ± 11,48 |
||||
|
Index |
Group |
T5 |
P |
T6 |
P |
T7 |
P |
|
Right rSO2 |
Propofol |
62,22 ± 6,33 |
0,611 |
63,07 ± 5 |
0,536 |
65,85 ± 5,67 |
0,853 |
|
Desflurane |
60,96 ± 11,02 |
61,76 ± 9,65 |
65,44 ± 9,84 |
||||
|
Left rSO2 |
Propofol |
63,19 ± 7,56 |
0,397 |
64,15 ± 5,84 |
0,709 |
67,85 ± 5,88 |
0,689 |
|
Desflurane |
60,92 ± 11,32 |
63,28 ± 10,38 |
66,84 ± 11,58 |
Two-Way
Mixed ANOVA.
Table 5: INVOS data during the procedure for each group
separately.
|
Group |
Index |
P |
||||
|
|
|
T2 vs T3 |
T2 vs T4 |
T2 vs T5 |
T2 vs T6 |
T2 vs T7 |
|
Propofol |
Right rSO2 |
0,067 |
0,241 |
0,019 |
0,028 |
0,921 |
|
Left rSO2 |
0,489 |
0,664 |
0,026 |
0,041 |
0,268 |
|
|
Desflurane |
Right rSO2 |
0,069 |
0,653 |
0,0115 |
0,107 |
0,173 |
|
Left rSO2 |
0,145 |
0,294 |
0,0004 |
0,053 |
0,685 |
|
Two-Way Mixed ANOVA.
Figure 1: Right INVOS data for both groups.
Figure 2: Left INVOS data for both groups.
Discussion
Our study indicated that when patients were turned to the prone position for spine surgery, the right and left rSO2 values were not significantly different between propofol and desflurane at equipotent concentrations in terms of BIS. Moreover, both propofol and desflurane were associated with a significant decrease in the rSO2 in the prone position compared to the supine position. Desflurane and propofol have been widely used because both anaesthetics are characterized by a rapid onset and a short duration, along with a quick post-anaesthetic recovery. However, desflurane and propofol affect cerebral oxygenation differently. Desflurane causes dose-dependent decreases in cerebrovascular resistance and cerebral metabolic rate of oxygen consumption, while propofol is associated with dose-dependent reduction of cerebral blood flow and cerebral metabolic rate, which results in a decrease of intracranial pressure [7, 8]. Compared to volatile anaesthetics delivered at BIS-equivalent doses, propofol causes a significant reduction of cerebral blood flow and a similar decrease in cerebral metabolic rate of oxygen consumption [9].
Other studies have demonstrated that volatile anaesthetics can maintain higher cerebral oxygenation than propofol during anaesthesia. These studies include procedures performed in the supine position for tumorectomy for breast cancer or inguinal hernia repair, in sitting position for arthroscopy, in Trendelenburg’s position for gynaecologic laparoscopic surgery or laparoscopic cholecystectomy [10-13]. All four studies compared sevoflurane and propofol regarding their effect on regional cerebral oxygen saturation using near-infrared spectroscopy monitoring. The discrepancy between those results and our findings raises the question whether the prone position was a contributing factor for differences between sevoflurane or desflurane volatile agent. Changes in body position or head rotation during surgery and various surgical manipulations can cause significant respiratory and cardiovascular alterations that can negatively affect cerebral perfusion and hemodynamics. Regarding the prone position, Babakhani et al. have demonstrated significant decreases in rSO2 after 30 and 60 minutes of prone positioning compared with the values in the supine, which were not clinically important and reached supine values after 90 minutes of the prone position. They used propofol for induction and a combination of propofol and sevoflurane for maintenance of anaesthesia [14]. They also stated that the decrease in rSO2 caused by prone position could be more severe in older patients, which is also supported by other studies [15].
Other perioperative positioning challenges may have different effects. Studies have suggested that Trendelenburg positioning with the head tilted down over a substantial surgical period did not affect cerebral oxygen saturation [16, 17]. In contrast, in the beach chair position, by positioning the anaesthetized patient head up, the oxygen saturation of the brain decreased by about 10% from baseline levels. In the context of comparing desflurane and propofol effects on cerebral oxygenation, Kim et al. studied the effects of these two anaesthetic agents in the sitting position [18]. The authors showed that the rSO2 decreased significantly from the baseline in both groups. These findings are consistent with our research which shows a decline in rSO2 in both propofol and desflurane groups 10 minutes after prone positioning. However, comparing rSO2 values between the two groups, the authors have shown that the rSO2 in the desflurane group was higher compared to the propofol group concluding that desflurane preserved rSO2 better than propofol. This is inconsistent with our results which suggest that there were no significant differences between these anaesthetics throughout the prone position period.
Closhen et al. studied the changes in cerebral oxygen saturation following prone positioning using 2 different monitors, an INVOS cerebral oximeter for continuous rSO2 measurement and a FORE-SIGHT cerebral oximeter for absolute cerebral tissue oxygenation (StO2) measurement, while also comparing awake and anaesthetized patients [19]. Propofol 2mgkg-1 was used for induction and sevoflurane 0.7-1.0 MAC to maintain anaesthesia. They reported an initial decrease in rSO2 (from 75%±8% to 72%±8%) and StO2 (from 74%±5% to 72%±4%) in anaesthetized patients after prone positioning with a subsequent increase rate of 0.0324%/min. Awake volunteers did not show any significant change in cerebral oxygenation after prone positioning. The authors reported that the prone position did not induce any clinically significant change in cerebral oxygen saturation in both patient groups. Our results are comparable regarding the desflurane group, where a significant initial reduction in rSO2 was recorded from supine to prone position and was followed by an increase in rSO2 at the end of surgery in the prone position. Whereas, in the propofol group the initial rSO2 reduction remained significant throughout the prone position period. This comparison suggests that sevoflurane and desflurane may share more in common than propofol regarding their activity on the cerebrovascular system.
In conclusion, in the present prospective randomized double-blinded study conducted on patients undergoing spinal surgery in the prone position, desflurane and propofol were associated with a significant decrease in rSO2 without differences between these two anaesthetics.
Author Contributions
Concepts: Koraki, Kapsokalyvas; Design: Koraki, Stergiouda, Gkioulava, Kapsokalyvas, Chatzopoulos; Definition of intellectual content: Koraki, Stergiouda, Gkioulava, Kapsokalyvas; Literature search: Koraki, Stergiouda, Sifaki, Gkioulava, Kapsokalyvas; Clinical studies: Koraki, Stergiouda, Sifaki, Gkioulava, Kapsokalyvas; Experimental studies: NA; Data acquisition: Stachtari, Bagntasarian, Chatzopoulos; Data analysis: Stachtari, Bagntasarian, Chatzopoulos; Statistical analysis: Stachtari, Bagntasarian, Chatzopoulos; Manuscript preparation: Stachtari, Bagntasarian, Sifaki; Manuscript editing: Stachtari, Bagntasarian, Sifaki; Manuscript review: Koraki, Stachtari, Bagntasarian; Guarantor: Koraki.
Acknowledgement
None.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 14, Apr 2021Accepted: Thu 29, Apr 2021
Published: Tue 04, May 2021
Copyright
© 2023 Stachtari Chrysoula. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ACR.2021.01.02
Author Info
Koraki Eleni Stachtari Chrysoula Bagntasarian Stella Gkiouliava Anna Sifaki Freideriki Stergiouda Zoi Kapsokalyvas Ioannis Chatzopoulos Stavros
Corresponding Author
Stachtari ChrysoulaDepartment of Anesthesiology, General Hospital of Thessaloniki “G. Papanikolaou”, Thessaloniki, Greece
Figures & Tables
Table 1: Demographic and clinical characteristics of study
patients.
|
Variable |
|
group propofol |
group desflurane |
P |
|
Age |
Years |
57 ± 11,13 |
55,8 ± 15,1 |
0,744a |
|
Height |
Cm |
74,48 ± 12,43 |
79,28 ± 12,31 |
0,601b |
|
Weight |
Kg |
166,15 ± 7,63 |
167,96 ± 8,2 |
0,502b |
|
BMI |
Kg/m2 |
27,19 ± 4,47 |
29,4 ± 3,01 |
0,063a |
|
Gender |
Male |
8 (29,63%) |
12 (48,00%) |
0,174c |
|
Female |
19 (70,37%) |
13 (52,00%) |
||
|
ASA |
1 |
3 (11,11%) |
3 (12,00%) |
0,980c |
|
2 |
18 (66,67%) |
16 (64,00%) |
||
|
3 |
6 (22,22%) |
6 (24,00%) |
||
|
Pre- induction hemodynamics SAP |
mmHg |
142,04 ± 19,79 |
148,92 ± 20,74 |
0,226a |
|
DAP |
mmHg |
82,48 ± 11,79 |
79,8 ± 11,1 |
0,403a |
|
HR |
beats/min |
75,63 ± 14,7 |
78,28 ± 13,56 |
0,503a |
|
SPO2 |
% |
95,3 ± 1,88 |
96,76 ± 2,74 |
0,056b |
|
Pre- induction rSO2 Right rSO2 |
% |
63,33 ± 7,42 |
61,36 ± 9,72 |
0,421a |
|
Left rSO2 |
% |
64,44 ± 7,7 |
62,84 ± 9,39 |
0,502a |
a:
Based on t-test, b: based on M-W test, c: based on Chi-Square test. Data are
presented as mean ± standard deviation or number (proportion, %)
BMI:
Body Mass Index; ASA: American Society of Anesthesiologist.
Table 2: Hemodynamic and end-tidal carbon dioxide tension
changes during prone position.
|
Index |
Group |
T2 |
T3 |
T4 |
T5 |
T6 |
T7 |
P |
|
SAP |
Propofol |
145,78 ± 22,38 |
112,3 ± 18,84 |
111,93 ± 20,66 |
114,63 ± 12,77 |
116,63 ± 15,18 |
121,48 ± 16,29 |
0,095 |
|
Desflurane |
148,2 ± 19,06 |
120,76 ± 21,65 |
104,84 ± 15,1 |
113,96 ± 17,87 |
109,28 ± 16,79 |
117,76 ± 17,57 |
||
|
DAP |
Propofol |
70,63 ± 11,82 |
64,07 ± 13,81 |
64,15 ± 9,93 |
68 ± 8,64 |
65,33 ± 8,35 |
64,74 ± 8,27 |
0,061 |
|
Desflurane |
70,28 ± 10,11 |
67,72 ± 11,96 |
58,6 ± 10,56 |
60,6 ± 7,42 |
58,84 ± 7,26 |
67,28 ± 9,07 |
||
|
HR |
Propofol |
73,52 ± 13,72 |
72,37 ± 12,53 |
66,48 ± 10,68 |
64,07 ± 11,23 |
62,15 ± 8,54 |
65,59 ± 13,1 |
0,357 |
|
Desflurane |
76,84 ± 13,76 |
79,4 ± 17,17 |
70,28 ± 13,95 |
65,16 ± 11,51 |
61,72 ± 7,13 |
68,44 ± 9,63 |
||
|
SPO2 |
Propofol |
98,37 ± 1,57 |
98,96 ± 1,02 |
98,52 ± 1,05 |
98,59 ± 1,22 |
98,96 ± 1,06 |
99,26 ± 0,86 |
0,088 |
|
Desflurane |
99,36 ± 0,64 |
99,08 ± 0,86 |
98,64 ± 0,76 |
98,76 ± 0,72 |
98,96 ± 0,73 |
99,16 ± 0,69 |
||
|
ETCO2 |
Propofol |
|
30,44 ± 3,25 |
30,78 ± 2,9 |
29,59 ± 2,26 |
31,22 ± 2,68 |
32,63 ± 2,99 |
0,328 |
|
Desflurane |
|
31,88 ± 4,72 |
31,24 ± 3,39 |
31,76 ± 2,59 |
32,44 ± 2,84 |
33,24 ± 2,77 |
Two-Way Mixed ANOVA.
Table 3: ABGs changes during prone positioning.
|
Index |
Group |
T3 |
T7 |
P |
|
PO2 |
Propofol |
272,96 ± 102,1 |
249,41 ± 74,89 |
0,542 |
|
Desflurane |
250,36 ± 98,99 |
246,48 ± 84,05 |
||
|
PCO2 |
Propofol |
36,3 ± 3,78 |
37,98 ± 3,56 |
0,394 |
|
Desflurane |
37,94 ± 3,83 |
38,52 ± 3,65 |
||
|
Hb |
Propofol |
12,36 ± 1,46 |
11,5 ± 1,51 |
0,768 |
|
Desflurane |
12,7 ± 1,49 |
11,94 ± 1,79 |
Two-Way Mixed ANOVA.
Table 4: INVOS data during the procedure between groups.
|
Index |
Group |
T2 |
P |
T3 |
P |
T4 |
P |
|
Right rSO2 |
Propofol |
66 ± 8,87 |
0,357 |
68,7 ± 9,41 |
0,275 |
64,33 ± 7,09 |
0,657 |
|
Desflurane |
63,68 ± 9,14 |
65,64 ± 10,59 |
63,16 ± 11,51 |
||||
|
Left rSO2 |
Propofol |
66,22 ± 9,39 |
0,958 |
67,59 ± 15,27 |
0,954 |
65,7 ± 8,03 |
0,646 |
|
Desflurane |
66,08 ± 10,21 |
67,8 ± 9,45 |
64,44 ± 11,48 |
||||
|
Index |
Group |
T5 |
P |
T6 |
P |
T7 |
P |
|
Right rSO2 |
Propofol |
62,22 ± 6,33 |
0,611 |
63,07 ± 5 |
0,536 |
65,85 ± 5,67 |
0,853 |
|
Desflurane |
60,96 ± 11,02 |
61,76 ± 9,65 |
65,44 ± 9,84 |
||||
|
Left rSO2 |
Propofol |
63,19 ± 7,56 |
0,397 |
64,15 ± 5,84 |
0,709 |
67,85 ± 5,88 |
0,689 |
|
Desflurane |
60,92 ± 11,32 |
63,28 ± 10,38 |
66,84 ± 11,58 |
Two-Way
Mixed ANOVA.
Table 5: INVOS data during the procedure for each group
separately.
|
Group |
Index |
P |
||||
|
|
|
T2 vs T3 |
T2 vs T4 |
T2 vs T5 |
T2 vs T6 |
T2 vs T7 |
|
Propofol |
Right rSO2 |
0,067 |
0,241 |
0,019 |
0,028 |
0,921 |
|
Left rSO2 |
0,489 |
0,664 |
0,026 |
0,041 |
0,268 |
|
|
Desflurane |
Right rSO2 |
0,069 |
0,653 |
0,0115 |
0,107 |
0,173 |
|
Left rSO2 |
0,145 |
0,294 |
0,0004 |
0,053 |
0,685 |
|
Two-Way Mixed ANOVA.

References
1.
DePasse JM,
Palumbo MA, Haque M, Eberson CP, Daniels AH (2015) Complications associated
with prone positioning in elective spinal surgery. World J Orthop 6:
351-359. [Crossref]
2.
Kwee MM, Ho YH,
Rozen WM (2015) The prone position during surgery and its complications: a
systematic review and evidence-based guidelines. Int Surg 100: 292-303.
[Crossref]
3.
Conti A, Iacopino DG, Fodale V, Micalizzi S, Penna O et
al. (2006) Cerebral haemodynamic changes
during propofol-remifentanil or sevoflurane anaesthesia: transcranial Doppler
study under bispectral index monitoring. Br J Anaesth 97: 333-339. [Crossref]
4.
Vandesteene A,
Trempont V, Engelman E, Deloof T, Focroul M et al. (1988) Effect of propofol on
cerebral blood flow and metabolism in man. Anaesthesia 43: 42-43. [Crossref]
5.
Craen RA, Gelb AW,
Murkin JM, Chonq KY (1992) Human cerebral autoregulation is maintained during
propofol air/o2 anesthesia. J Neurosurg Anesthesiol 4.
6.
Mielck F, Stephan
H, Buhre W, Weyland A, Sonntag H (1998) Effects of 1 MAC desflurane on cerebral
metabolism, blood flow and carbon dioxide reactivity in humans. Br J Anaesth
81: 155-160. [Crossref]
7.
Young WL (1992)
Effects of desflurane on the central nervous system. Anesth Analg 75:
S32-S37. [Crossref]
8.
Bastola P, Bhagat
H, Wig J (2015) Comparative evaluation of propofol, sevoflurane and desflurane
for neuroanaesthesia: A prospective randomised study in patients undergoing
elective supratentorial craniotomy. Indian J Anaesth 59: 287-294. [Crossref]
9.
Slupe AM, Kirsch
JR (2018) Effects of anesthesia on cerebral blood flow, metabolism, and
neuroprotection. J Cereb Blood Flow Metab 38: 2192-2208. [Crossref]
10. Valencia L, Rodríguez Pérez A, Kühlmorgen B, Santana
RY (2014) Does sevoflurane preserve regional cerebral oxygen saturation
measured by near-infrared spectroscopy better than propofol? Ann Fr Anesth
Reanim 33: e59-e65. [Crossref]
11. Jeong H, Jeong S, Lim HJ, Lee J, Yoo KY (2012) Cerebral
oxygen saturation measured by near-infrared spectroscopy and jugular venous
bulb oxygen saturation during arthroscopic shoulder surgery in beach chair
position under sevoflurane-nitrous oxide or propofol-remifentanil anesthesia. Anesthesiology
116: 1047-1056. [Crossref]
12. Kim SJ, Kwon JY, Cho AR, Kim HK, Kim TK (2011) The
effects of sevoflurane and propofol anesthesia on cerebral oxygenation in
gynecological laparoscopic surgery. Korean J Anesthesiol 61: 225-232. [Crossref]
13. Ružman T, Šimurina T, Gulam D, Ružman N, Miškulin M
(2017) Sevoflurane preserves regional cerebral oxygen saturation better than
propofol: Randomized controlled trial. J Clin Anesth 36: 110-117. [Crossref]
14. Babakhani B, Heroabadi A, Hosseinitabatabaei N, Schott
M, Yekaninejad S et al. (2017) Cerebral oxygenation under general anesthesia
can be safely preserved in patients in prone position: A prospective
observational study. J Neurosurg Anesthesiol 29: 291-297. [Crossref]
15. Deiner S, Chu I, Mahanian M, Lin HM, Hecht AC et al.
(2014) Prone position is associated with mild cerebral oxygen desaturation in
elderly surgical patients. PLoS One 9: e106387. [Crossref]
16. Closhen D, Treiber AH, Berres M, Sebastiani A, Werner
C et al. (2014) Robotic assisted prostatic surgery in the Trendelenburg
position does not impair cerebral oxygenation measured using two different
monitors: A clinical observational study. Eur J Anaesthesiol 31:
104-109.
17. Kalmar AF, Dewaele F, Foubert L, Hendrickx JF,
Heeremans EH et al. (2012) Cerebral haemodynamic physiology during steep
Trendelenburg position and CO(2) pneumoperitoneum. Br J Anaesth 108:
478-484. [Crossref]
18. Kim JY, Lee JS, Lee KC, Kim HS, Kim SH et al. (2014)
The effect of desflurane versus propofol on regional cerebral oxygenation in
the sitting position for shoulder arthroscopy. J Clin Monit Comput 28:
371-376. [Crossref]
19. Closhen D, Engelhard K, Dette F, Werner C, Schramm P
(2015) Changes in cerebral oxygen saturation following prone positioning for
orthopaedic surgery under general anaesthesia: a prospective observational
study. Eur J Anaesthesiol 32: 381-386. [Crossref]
