Effectiveness of School Based Health Clinics on Utilization of Sexual and Reproductive Health Services Among School Girls Aged 15-19 Years in Uganda: Cluster Randomized Trial
A B S T R A C T
Background: Sexual and reproductive needs among adolescents remain largely unmet in Uganda, this coupled with poor access and utilization of adolescent sexual and reproductive health services among secondary school girls increases vulnerability to high risk sexual practices and adolescent pregnancy. This study aimed at evaluating the effect of providing school based sexual and reproductive health services on utilization of the services among school girls aged 15-19 years attending secondary schools in Uganda.
Methods: The study used Cluster Randomized Controlled Trial (CRCT) design. Twenty secondary schools (clusters) were selected using cluster sampling and allocated 1:1 into control or intervention group stratified by geographical location. 1,182 (average cluster size of 60) girls aged 15-19 years were selected using simple random sampling. The intervention group received tailored Sexual and Reproductive Health (SRH) services information, in-school SRH services delivery and referral for a period of ten months. The control group received no intervention from the research team but had access to the usual public health care. Data was collected at baseline and end of study; descriptive statistics and inferential analysis was done as well as structural equation modeling using SPSS.
Results: There was a significant variation in the proportion of school girls who reported receiving more than three services between the control group and intervention group (χ2 = 4.503, p = < 0.001). The findings indicate that the utilization of SRH services was higher (65.4%) among the girls who had access to School Based SRH services (intervention group) compared 34.6% among the girls who had access to services within the public/government health facilities (control group).
Conclusion: Provision of School Based SRH services is an effective intervention for improving utilization of sexual and reproductive health services among school going adolescents. This is key in addressing the SRH needs of adolescents and promoting safe sexual practices.
Keywords
Adolescents, utilization, sexual and reproductive health (SRH), services, school-based
Introduction
World Health Organization defines an adolescent as any person between ages 10 and 19 years and further recognizes adolescence as a transitional phase of growth and development between childhood and adulthood [1]. United Nations Children’s Fund defines an adolescent pregnancy as a young girl aged 13-19 years who becomes pregnant or has had a live birth [2]. Half of the world’s population is under 25 years and the population of young people aged between 10-25 years is estimated to be 1.8 billion with about 85% living in the developing world [2]. In many cases adolescents consider themselves grown up and mature enough to have sex, have an intense drive which makes a man and woman desire to be in company of each other and yet they have inadequate knowledge about the consequences of unprotected sex including unwanted pregnancy, complications of unsafe abortion, early marriage and sexually transmitted infections [3-9]. Adolescent sexuality and its consequences are further aggravated by the prevailing customs, religious belief, substance use, lack of education and information about reproductive sexual health, lack of access to tools that prevent pregnancies, peer pressure to engage in sexual activity, incorrect use of contraception, sexual abuse that leads to rape, poverty, exposure to abuse, violence, family strife at home and low self-esteem [10-12].
As a result, 49% of girls in Least Developed Countries (LDCs) marry before they turn 18 while 10% – 40% of young unmarried girls have had an unintended pregnancy giving rise to about 14 million children worldwide who are born every year to young married and unmarried women aged 15 to 19 years [2, 11]. When a girl becomes pregnant, her education may end, her job prospects diminish, she becomes more vulnerable to poverty, her health often suffers and the complications from pregnancy and childbirth are the leading cause of death among adolescent girls [11]. Adolescent pregnancy is not always as a result of a deliberate choice, often unintended pregnancy among the adolescent girls is a consequence of little or no access to Adolescent Sexual and Reproductive Health (ASRH) information and services [11, 13].
Uganda has had an adolescent pregnancy rate of 25% among girls 15 to 19 years for the last ten years and yet the level of SRH service utilization remains low at 30% [14, 15]. In a study conducted among school girls and boys in Mityana, Uganda, the level of SRH service utilization was found to be at 73.3% which is higher than 30% for the general population, this was further justified by the fact that over 41% of the participants reported abstinence drive education as the most utilized service which is contrary to 68% sexuality rate reported by the ministry of education in Uganda [16]. This clearly shows that there is an unmet need for SRH services among school adolescents especially the vulnerable girls.
According to Uganda Bureau of Statistics, the communities within Bunyoro region where Hoima District is found have one of the lowest ASRH access rates for adolescents with only 8% having access to youth counseling services, 4% to peer education, 3.4% SRH education, 0.3% pregnancy information and checkups and 0.1% post abortion care in the community [14]. No data found on ASRH services for school going adolescents because majority of the adolescent programs focus on youth out of school. The main gap in the provision of SRH services is the location which consequently may influence access and utilization of services by adolescents in school. The girls’ in-schools have been disadvantaged in such a way that they spend most of their time at school where ASRH services are unavailable; this increases their vulnerability to unhealthy and early sexual practices which increases their risk to unintended pregnancy. It is therefore paramount that schoolgirls are provided with information and services to enable them to meet their sexuality needs safely.
The WHO recommended ASRH package includes: 1) comprehensive sexuality education (CSE) provision; 2) contraception counselling and provision; 3) antenatal, intrapartum and postnatal care; 4) safe abortion care; 5) sexually transmitted infections (STIs) prevention and care; 6) human immunodeficiency virus (HIV) prevention and care; 7) violence against women and girls prevention, support and care; and 8) harmful traditional practices prevention [17]. In line with the global standards, Uganda launched the national sexuality framework and also promotes the Uganda Adolescent Health Policy Guidelines and Services Standards which clearly highlight 1) Clinical Care for Sexual gender-based violence; 2) Prenatal care and maternity care for pregnant adolescents; 3) HPV immunization; 4) HIV counseling and testing; 5) Breast examination and information on cancer cervix; 6) Information and counselling on health especially growth and development; 7) Information on their rights and responsibilities; 8) Referral and follow up [18, 19].
However, the Ugandan policy guideline excludes provision of key reproductive health services which are vital for prevention of adolescent pregnancy and mortality due to pregnancy related complications such as family planning and post abortion care. The clinic and community based SRH services have not addressed the needs of the adolescents in school because both take place during the same working hours hence inaccessible for adolescents in school [20]. This study therefore aimed at removing barrier of access to services by providing SRH services within the school premises and the effect of the school-based services on improving utilization was evaluated [21, 22].
Methods and Materials
The Cluster Randomized Controlled Trial (CRCT) design was used to conduct this evaluation research and took on the epistemological lens of positivism so as to determine the effect of the school-based intervention on service utilization objectively [23, 24]. The study was guided by the Consolidated Standards of Reporting Trials (CONSORT) guidelines and Clinical trial guidelines [25, 26].
The study was conducted in Hoima District located in western Uganda, sample size was determined using Campbell and Walters method for comparing differences in rates and or proportions between two groups and determining the number of subjects per group for a two-sided significance level [26]. A total of 1,182 adolescent girls aged 15-19 years who were attending the 20 randomly selected secondary schools in Hoima District were enrolled in the study randomly. The unit of randomization was at cluster level. The 20 cluster (eligible schools) were randomly allocated to either the intervention (10 schools) or the control (10 schools) arms of the study at a ratio of 1:1. Formally consent was sought from girls aged 18 years and above while parent consent and assent was sought from the girls who were below 18 years.
The intervention package was provided for ten months in the 10 intervention clusters and included adolescent SRH education and information; SRH medical care and referral. The intervention was based on the Uganda national sexuality framework and SRH guidelines.
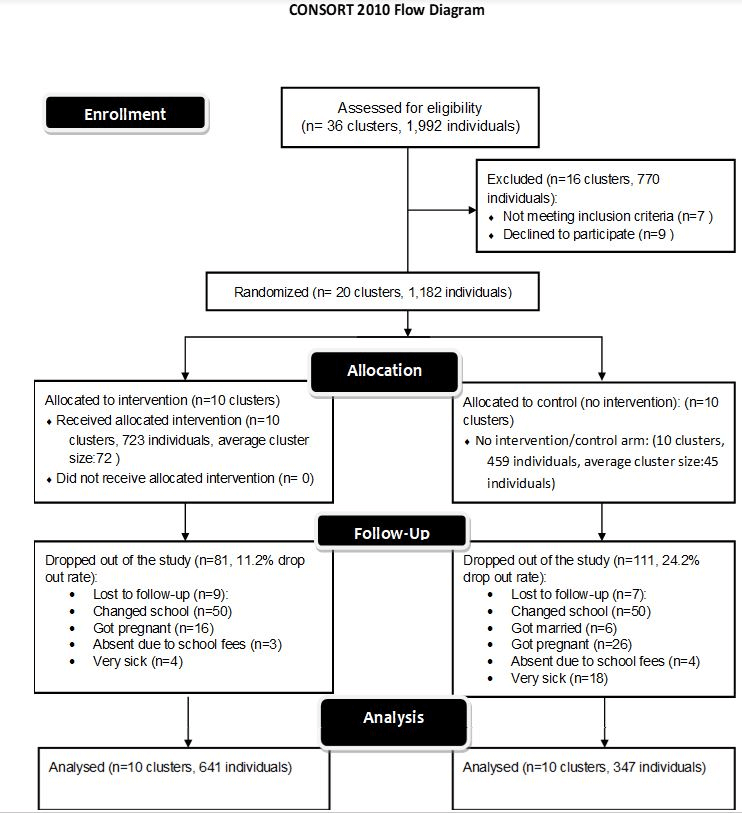
Data was collected using structured questionnaire which had an item rated Content Validity Index of 86% and was also underwent face validity by two experts [27, 28]. In addition, the questionnaire had a Cronbach alpha of 0.807 which was considered to be good [26, 29]. Double blinding was done by concealing the type of SRH package from participants and data collectors were not aware which intervention arm each cluster belonged to. Participant flow is shown in (Figure 1) and data was analyzed using SPSS Version 20 to generate descriptive and inferential statistics.
Figure 1: CONSORT 2010 Participant flow diagram.
Results
The entire study had a total of 1,182 participants, of these, 57.2% (676) were aged 15-16 years, 39.5% (466) aged 17-18 years and 3.4% (40) were aged 19 years and above. Majority 91.4% (1,080) of the participants were Christians, 98.7% (1,167) of the participants were Ugandans while 71.1% (840) were in the boarding section of the school. Most of the participants were in senior three (55.7%) and senior two (32.3%) classes. 93.2% (1,101) of the participants were in schools which had both day and boarding sections as shown in (Table 1).
The study results in (Table 1) show that there was no statistical difference in the demographic characteristics of the participants in the intervention group compared to the participants in the control group. The results there indicate that the demographics of all participants were generally the same in both study groups which means that the randomization of the clusters was properly conducted. There was no observed imbalance in the baseline variables in both the intervention group and the control group, it is assumed that the outcome of the study was due to the intervention [25, 30].
Utilization of SRH services was measured by the reported receipt of the various services by the individual schoolgirls and this was considered as follows:
i. Receipt of few services: School girls who did not receive any service or received three services or less were considered to have received few or inadequate SRH services.
ii. Receipt of comprehensive services: School girls who received more than three SRH services were considered to have received comprehensive SRH services.
Table 1: Summary statistics of key socio demographic characteristics of the participants at baseline.
|
Demographics |
Intervention N (%) |
Control N (%) |
χ2 |
P-Valuea |
|
|
Age in years |
|
|
|
|
|
|
|
15-16 |
425(58.7) |
251(54.8) |
2.047 |
0.359 |
|
|
17-18 |
277(38.3) |
189(41.3) |
|
|
|
|
19+ |
22(3.0) |
18(3.9) |
|
|
|
Religion |
|
|
|
|
|
|
|
Christian |
669(92.4) |
411(89.7) |
2.528 |
0.112 |
|
|
Non-Christian |
55(7.6) |
47(10.3) |
|
|
|
Father Occupation |
|
|
|
|
|
|
|
Employed |
162(22.4) |
92(20.1) |
4.850 |
0.303 |
|
|
Business |
239(33.0) |
137(29.9) |
|
|
|
|
Farmer |
204(28.2) |
148(32.3) |
|
|
|
|
Not Employed |
16(2.2) |
16(3.5) |
|
|
|
|
Not Applicable |
103(14.2) |
65(14.2) |
|
|
|
Mother Occupation |
|
|
|
|
|
|
|
Employed |
86(11.9) |
50(10.9) |
1.256 |
0.869 |
|
|
Business |
294(40.6) |
199(43.4) |
|
|
|
|
Farmer |
249(34.4) |
154(33.6) |
|
|
|
|
Not Employed |
36(5.0) |
19(4.1) |
|
|
|
|
Not Applicable |
59(8.1) |
36(7.9) |
|
|
|
Class |
|
|
|
|
|
|
|
S.1 |
75(10.4) |
57(12.4) |
6.494 |
0.090 |
|
|
S.2 |
221(30.5) |
160(34.9) |
|
|
|
|
S.3 |
423(58.4) |
235(51.3) |
|
|
|
|
S.5 |
5(0.7) |
6(1.3) |
|
|
|
School Type |
|
|
|
|
|
|
|
Day Only |
42(5.8) |
36(7.9) |
3.341 |
0.164 |
|
|
Boarding Only |
3(0.4) |
0(0.0) |
|
|
|
|
Day and Boarding |
679(93.8) |
422(92.1) |
|
|
|
Participant-Day Scholar Vs Boarding |
|
|
|
||
|
|
Day Scholar |
214(29.6) |
128(27.9) |
0.354 |
0.552 |
|
|
Boarding |
510(70.4) |
330(72.1) |
|
|
|
Parent Marital Status |
|
|
|
|
|
|
|
Married |
389(53.7) |
232(50.7) |
4.160 |
0.245 |
|
|
cohabiting |
106(14.6) |
87(19.0) |
|
|
|
|
Separated |
175(24.2) |
103 (22.5) |
|
|
|
|
widowed |
54(7.5) |
36(7.9) |
|
|
|
a Comparison between Intervention and comparison groups |
|||||
**Significant at 5% level. Data source: Primary data, 2019.
I Baseline
Findings in (Table 2) show that 61.4% (726/1,182) of the schoolgirls reported to have received more than three SRH services during the six-month period prior to the study. Most study participants received more than three services in both the intervention and the control groups (59.6% vs 40.4%). The proportion of schoolgirls that reported receiving more than three services did not however statistically vary at baseline (χ2 = 2.056, p = 0.159). This means that there was no variation in the type of services provided and access by the schoolgirls hence resulting in similar levels of utilization of SRH services for the girls in both the intervention and control groups. Therefore, the variations observed among the schoolgirls in the intervention group at the end of the intervention are strongly attributed to the intervention (school based SRH services) provided during the study.
II End of Intervention
At the end of the intervention, 97% (958/988) reported to have received more than three services within the period of the study. However, the proportion of schoolgirls in the intervention arm who reported receiving more than three services had increased from 59.6% at baseline to 65.4% by the end of the intervention but respectively lowered from 40.4% to 34.6% in the control group. There was significant variation in the proportion of schoolgirls who reported receiving more than three services between the two groups (χ2 = 4.503, p < 0.001).
Table 2: Utilization of School Based SRH services among schoolgirls aged 15-19 years.
|
School Based SRH services |
Intervention N (%) |
Control N (%) |
χ2(df) |
P-Valuea |
|
|
Baseline |
|
|
|
|
|
|
SRH services utilized 6 months prior to the study |
|
|
|
|
|
|
|
0-3 services |
291(63.8) |
165(36.2) |
2.056 |
0.159 |
|
|
More than 3 services |
433(59.6) |
293(40.4) |
|
|
|
End-line |
|
|
|
|
|
|
SRH services utilized during the study |
|
|
|
|
|
|
|
0-3 services |
14(46.7) |
16(53.3) |
4.503 |
0.039** |
|
|
More than 3 services |
627(65.4) |
331(34.6) |
|
|
|
a Comparison between Intervention and comparison groups |
|||||
**Significant at 5% level. Data source: Primary data, 2019.
Discussion
The findings indicate that the utilization of SRH services was higher (65.4%) among the girls who had access to School Based SRH services compared 34.6% among the girls who had access to services within the public/government health facilities. Findings differ slightly with a study by Ntulume which indicated that the overall access and utilization of SRH services among school adolescents was 73.3% with abstinence drive (41%) as the most utilized services [16]. However, it is important to note that in Ntulume’s study, abstinence education was the most utilized service, yet utilization of services in this study is mainly focused on individuals who received more than 3 services hence being considered as having received comprehensive SRH services.
The findings of this study do not agree with two cross sectional studies conducted in Nigeria and Ethiopia among school adolescents, the level of utilization was found to be only 33.8% and 21.2% respectively among adolescents who reported to have utilized at least one of reproductive health services [31, 32]. The results of the Nigeria and Ethiopian studies are lower than the findings in this study that show that the schoolgirls who received only three or less services were 46.7% and 53.3% among the girls within the intervention group and control group respectively. This study did not focus on just receipt of one service but rather on how comprehensive the services were for the participant and indeed found that the proportion of girls who received three or less services was higher (46.7% in intervention group and 53.3% in control group) than the proportion (33.8% in Nigeria and 21.2% in Ethiopia) [31, 32]. This may be attributed to methodology used in conducting the research as well as the geographical access and availability of services within the free public health facilities in Uganda.
Conclusion
Provision of school based SRH services greatly improves utilization among schoolgirls aged 15-19 years. Further research in the actual SRH services highly demanded for by the adolescent boys and girls would enhance program design and implementation in a bid to address the SRH needs of the adolescent.
Acknowledgements
Special thanks to Brenda Katusiime, the research assistant who significantly participated in the data collection and entry process. The District and school leadership in Hoima District for the enormous support as well as the study participants for the valuable information provided.
Funding
None.
Conflicts of Interest
None.
Trial Registration
This study was nested out of the larger cluster randomized trial registered by the Pan African Clinical Trial Registry (PACTR201810882140200).
Article Info
Article Type
Research ArticlePublication history
Received: Thu 14, May 2020Accepted: Mon 25, May 2020
Published: Sat 30, May 2020
Copyright
© 2023 Gloria Kasozi Kirungi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JCMCR.2020.02.02
Author Info
Frank Pio Kiyingi Gloria Kasozi Kirungi Julius Kasozi Miph Musoke
Corresponding Author
Gloria Kasozi KirungiSchool of Post Graduate Studies and Research, Nkumba University, Entebbe, Uganda
Figures & Tables
Table 1: Summary statistics of key socio demographic characteristics of the participants at baseline.
|
Demographics |
Intervention N (%) |
Control N (%) |
χ2 |
P-Valuea |
|
|
Age in years |
|
|
|
|
|
|
|
15-16 |
425(58.7) |
251(54.8) |
2.047 |
0.359 |
|
|
17-18 |
277(38.3) |
189(41.3) |
|
|
|
|
19+ |
22(3.0) |
18(3.9) |
|
|
|
Religion |
|
|
|
|
|
|
|
Christian |
669(92.4) |
411(89.7) |
2.528 |
0.112 |
|
|
Non-Christian |
55(7.6) |
47(10.3) |
|
|
|
Father Occupation |
|
|
|
|
|
|
|
Employed |
162(22.4) |
92(20.1) |
4.850 |
0.303 |
|
|
Business |
239(33.0) |
137(29.9) |
|
|
|
|
Farmer |
204(28.2) |
148(32.3) |
|
|
|
|
Not Employed |
16(2.2) |
16(3.5) |
|
|
|
|
Not Applicable |
103(14.2) |
65(14.2) |
|
|
|
Mother Occupation |
|
|
|
|
|
|
|
Employed |
86(11.9) |
50(10.9) |
1.256 |
0.869 |
|
|
Business |
294(40.6) |
199(43.4) |
|
|
|
|
Farmer |
249(34.4) |
154(33.6) |
|
|
|
|
Not Employed |
36(5.0) |
19(4.1) |
|
|
|
|
Not Applicable |
59(8.1) |
36(7.9) |
|
|
|
Class |
|
|
|
|
|
|
|
S.1 |
75(10.4) |
57(12.4) |
6.494 |
0.090 |
|
|
S.2 |
221(30.5) |
160(34.9) |
|
|
|
|
S.3 |
423(58.4) |
235(51.3) |
|
|
|
|
S.5 |
5(0.7) |
6(1.3) |
|
|
|
School Type |
|
|
|
|
|
|
|
Day Only |
42(5.8) |
36(7.9) |
3.341 |
0.164 |
|
|
Boarding Only |
3(0.4) |
0(0.0) |
|
|
|
|
Day and Boarding |
679(93.8) |
422(92.1) |
|
|
|
Participant-Day Scholar Vs Boarding |
|
|
|
||
|
|
Day Scholar |
214(29.6) |
128(27.9) |
0.354 |
0.552 |
|
|
Boarding |
510(70.4) |
330(72.1) |
|
|
|
Parent Marital Status |
|
|
|
|
|
|
|
Married |
389(53.7) |
232(50.7) |
4.160 |
0.245 |
|
|
cohabiting |
106(14.6) |
87(19.0) |
|
|
|
|
Separated |
175(24.2) |
103 (22.5) |
|
|
|
|
widowed |
54(7.5) |
36(7.9) |
|
|
|
a Comparison between Intervention and comparison groups |
|||||
**Significant at 5% level. Data source: Primary data, 2019.
Table 2: Utilization of School Based SRH services among schoolgirls aged 15-19 years.
|
School Based SRH services |
Intervention N (%) |
Control N (%) |
χ2(df) |
P-Valuea |
|
|
Baseline |
|
|
|
|
|
|
SRH services utilized 6 months prior to the study |
|
|
|
|
|
|
|
0-3 services |
291(63.8) |
165(36.2) |
2.056 |
0.159 |
|
|
More than 3 services |
433(59.6) |
293(40.4) |
|
|
|
End-line |
|
|
|
|
|
|
SRH services utilized during the study |
|
|
|
|
|
|
|
0-3 services |
14(46.7) |
16(53.3) |
4.503 |
0.039** |
|
|
More than 3 services |
627(65.4) |
331(34.6) |
|
|
|
a Comparison between Intervention and comparison groups |
|||||
**Significant at 5% level. Data source: Primary data, 2019.
References
- World Health Organization (2014) Adolescent health and development. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland.
- United Nations Children’s Fund (UNICEF, 2008). The state of the world's children 2009. Maternal and newborn health, UNICEF. 978-92-806-4318-3. United Nations Children’s Fund, 3 United Nations Plaza, New York, NY 10017, USA.
- Green G, Pool R, Harrison S, Hart GJ, Wilkinson J et al. (2001) Female Control of Sexuality: Illusion or Reality? Use of Vaginal Products in South West Uganda. Soc Sci Med 52: 585-598. [Crossref]
- Nyanzi S, Pool R, Kinsman J (2001) The Negotiation of Sexual Relationships Among School Pupils in South-Western Uganda. AIDS Care 13: 83-98. [Crossref]
- Nzioka C (2001) Perspectives of Adolescent Boys on the Risks of Unwanted Pregnancy and Sexually Transmitted Infections: Kenya. Reprod Health Matters 9: 108-117. [Crossref]
- Ankwasiize EG, Kiyingi FP (2015) Marvels of managing Human sexuality; the theory and practice. Smmart stationers limited, Kampala, Uganda.
- Lema VM, Mpanga V, Makanani BS (2002) Socio-demographic Characteristics of Adolescent Post-Abortion Patients in Blantyre, Malawi. East Afr Med J 79: 306-310. [Crossref]
- Soderberg H, Andersson C, Janzon L, Sjoberg NO (1997) Continued Pregnancy Among Abortion Applications. A Study of Women Having a Change of Mind. Acta Obstet Gynecol Scand 76: 942-947. [Crossref]
- Felice ME, Feinstein RA, Fisher MM, Kaplan DW, Olmedo LF et al. (1999) Adolescent Pregnancy--Current Trends and Issues: 1998 American Academy of Pediatrics Committee on Adolescence, 1998-1999. Pediatrics 103: 516-520. [Crossref]
- World Health Organization (2012) Early marriages, adolescent and young pregnancies. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland.
- United Nation Population Fund (2017) Technical guidance on prioritizing adolescent health and Adolescent pregnancy.
- Birdthistle I, Whitman CV (1997) Reproductive Health Programs for Young Adults: School-Based Programs. Education Development Center Inc Focus on Young Adults. Res Series 7: 71.
- Kemigisha E, Bruce K, Nyakato VN, Ruzaaza GN, Ninsiima AB et al. (2018) Sexual Health of Very Young Adolescents in South Western Uganda: A Cross-Sectional Assessment of Sexual Knowledge and Behavior. Reprod Health 15: 148. [Crossref]
- Uganda Bureau of Statistics (UBOS), ICF (2017) Uganda Demographic and Health Survey 2016: Key Indicators Report Kampala, Uganda: UBOS, and Rockville, Maryland, USA: UBOS and ICF.
- Ivanova O, Rai M, Mlahagwa W, Tumuhairwe J, Bakuli A et al. (2019) A Cross-Sectional Mixed-Methods Study of Sexual and Reproductive Health Knowledge, Experiences and Access to Services Among Refugee Adolescent Girls in the Nakivale Refugee Settlement, Uganda. Reprod Health 16: 35. [Crossref]
- Ntulume CK (2018) Access to and Utilization of Adolescent Sexual and Reproductive Health Services among Secondary School Students in Mityana district, Uganda. J Biomed Res Stud 1: 102.
- World Health Organisation (2018) WHO recommendations on adolescent sexual and reproductive health and rights. ISBN 978-92-4-151460-6. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland.
- Ministry of Education and Sports (2018) National Sexuality Education Framework 2018. Kampala, Uganda.
- Ministry of Health (2012) Adolescent Health Policy Guidelines and Services Standards. In: Kampala Uganda: The Reproductive Health Division. 3rd ed. Uganda: Department of Community Health, Ministry of Health.
- Atun R, de Jongh T, Secci F, Ohiri K, Adeyi O (2010) Integration of Targeted Health Interventions Into Health Systems: A Conceptual Framework for Analysis. Health Policy Plan 25: 104-111. [Crossref]
- Keeton V, Soleimanpour S, Brindis CD (2012) chool-based Health Centers in an Era of Health Care Reform: Building on History. Curr Probl Pediatr Adolesc Health Care 42: 132-156. [Crossref]
- Arenson M, Hudson PJ, Lee N, Lai B (2019) The Evidence on School-Based Health Centers: A Review. Global Pediatr Health 6: 2333794X19828745. [Crossref]
- Hayes RJ, Bennett S (1999) Simple Sample Size Calculation for Cluster-Randomized Trials. Int J Epidemiol 28: 319-326. [Crossref]
- Moon K, Blackman D (2014) A Guide to Understanding Social Science Research for Natural Scientists. Conserv Biol 28: 1167-1177. [Crossref]
- Campbell MK, Piaggio G, Elbourne DR, Altman DG, CONSORT Group (2012) Consort 2010 Statement: Extension to Cluster Randomised Trials. BMJ 345: e5661. [Crossref]
- Campbell MJ, Walters SJ (2014) How to design, analyze and report cluster randomized trials in medicine and health related research. John Wiley & Sons Ltd, the Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, United Kingdom.
- Yusoff MSB (2019) ABC of content validation and content validity index calculation. Educ Med J 11: 49-54.
- Larsson H, Tegern M, Monnier A, Skoglund J, Helander C et al. (2015) Content Validity Index and Intra- and Inter-Rater Reliability of a New Muscle Strength/Endurance Test Battery for Swedish Soldiers. PLoS One 10: e0132185. [Crossref]
- Aparasu R (2011) Research methods for pharmaceutical practices and policy. Pharmaceutical Press, United States of America.
- Roberts C, Torgerson DJ (1999) Understanding Controlled Trials: Baseline Imbalance in Randomised Controlled Trials. BMJ 319: 185. [Crossref]
- Tlaye KG, Belete MA, Demelew TM, Getu MA, Astawesegn FH (2018) Reproductive Health Services Utilization and Its Associated Factors Among Adolescents in Debre Berhan Town, Central Ethiopia: A Community-Based Cross-Sectional Study. Reprod Health 15: 217. [Crossref]
- Binu W, Marama T, Gerbaba M, Sinaga M (2018) Sexual and reproductive health services utilization and associated factors among secondary school students in Nekemte town, Ethiopia. Reprod Health 15: 64. [Crossref]
