A B S T R A C T
Objectives: Extra Levator Abdominoperineal Excision (ELAPE) is an emerging technique for the management of locally advanced distal rectal cancers. Current evidence suggests that this technique is associated with better oncological outcomes and hence survival. Extra levator abdominoperineal excision is associated with significant perineal complications both in short and long term. The objective of the current study is to emphasize on the early wound complications of the above-mentioned procedure.
Study Design: It was a retrospective observational study with continent sampling.
Place and Duration of Study: The study was conducted at department of Surgical Oncology Shaukat Khanum Memorial Cancer Hospital & Research Center Lahore, Pakistan. The study period was from 1st January 2014 to 31st December, 2019.
Patients and Methods: A total of 84 patients were included in the study who underwent extra levator abdominoperineal excision (ELAPE). All patients undergoing extra levator abdominoperineal excision during the said period were included.
Results: A total of 84 patients underwent Extra Levator Abdominoperineal Excision between January 2014 and December 2019. Wound infection was observed in 32 (38.09%) of the patients. Wound dehiscence was seen is five patients. Median day of detection of infection was day 10 (5-22). Median hospital stay was 7 (4-22) days.
Conclusion: Extra Levator Abdominoperineal Excision is a procedure with significant perineal wound complication rate. The occurrence of perineal wound complications is multifactorial. Judicial use of the procedure is warranted.
Keywords
Distal rectal cancer, extra levator, extra levator abdominoperineal excision, abdominoperineal excision, perineal wound, dehiscence
Introduction
Extralevator Abdominoperineal Excision (ELAPE) is an emerging technique for the management of locally advanced distal rectal tumors in which sphincter preservation cannot be performed. The technique has not yet been adopted globally, however now as evidence is emerging more and more centers are adopting this technique. There is an ongoing debated whether ELAPE has oncological and survival benefits. Many studies have shown improved oncological outcomes and hence survival in patients undergoing ELAPE as compared to conventional abdominoperineal excision (CAPE) for the management of locally advanced distal rectal cancers [1].
Management of rectal cancers is complex as various factors like local disease burden, co morbidities, distance from anal verge and sphincter involvement influence the decision of operative strategy [2]. The preferred operation in the management of rectal cancers is anterior resection (AR) or low anterior resection (LAR) with preservation of the sphincter and colorectal anastomosis [3]. However, in certain circumstances the sphincters must be sacrificed and abdominoperineal resection with end colostomy has to be carried out to obtain oncological clearance. The overall prognosis of patients of distal rectal cancer is worse as compared to proximal rectal and rectosigmoid cancers because the distal few cm of rectum is devoid of mesorectum and the nearby structures such as prostate in males and vagina in females anteriorly and the levator muscles laterally are closely present without any significant barriers to prevent local invasion [4]. Thus, it is common for these cancers to present at an advanced stage. Likewise, abdominoperineal excision (APE) carries a poorer prognosis as compared to anterior resection (AR) and low anterior resection (LAR), which are mostly done for upper and mid rectal cancers.
The concept of total mesorectal excision (TME) has improved patient outcomes in the rectal cancer [5]. Since its introduction by Heald et al. in 1982 it has revolutionized the management of rectal cancer. However, as the distal few cm of rectum are devoid of mesorectum the prognosis of distal rectal cancer remains poor. Positive circumferential margins (CRM) and intra-operative tumor perforations are one of the major factors that lead to local disease relapse and overall poor patient outcomes [6]. To overcome the poor outcomes the concept of ELAPE was introduced by Holm et al. in 2007 [7]. ELAPE involves TME up to the coccyx posteriorly and Denonviller’s fascia anteriorly. At this point further dissection southwards is stopped to prevent conning and wasting of the specimen. Further perineal part is being performed in prone Jack- Knife position. ELAPE leaves a pelvic defect that can be reconstructed with either mesh or flaps, or it can be closed primarily [8].
ELAPE is also associated with more early and late perineal wound complications. The Early perineal complications range from wound infection to dehiscence [9]. Various studies have stated that the wound complications are more pronounced in ELAPE as compared to CAPE due to more extensive dissection. Most of the cases that undergo ELAPE have already been previously radiated as part of neoadjuvant approach that further decreases the ability of the tissue to heal post-operatively [10]. Perineal wound infection has been reported in up to 44% of cases undergoing ELAPE [11]. Infection and sepsis increase patient morbidity, duration of hospital stay, cost of treatment and delayed return to adjuvant treatment [9]. The aim of our study is to focus on perineal wound complications following ELAPE at our institute.
Materials and Methods
This was a retrospective analysis of patients undergoing ELAPE at Department of Surgical Oncology, Shaukat Khanum Memorial Cancer Hospital & Research Center (SKMCH&RC) between 1st January 2014 and 31st December 2019 and all patients who underwent ELAPE during the said time were included. A total of 84 patients met the criteria. The data was retrospectively retrieved from hospital information system (HIS) that is a fully electronic data system that is prospectively maintained. We retrieved the demographic, pathological, radiological and treatment data. Patient’s follow-ups and examinations were retrospectively reviewed in the HIS.
After initial diagnostic and staging workup, all patients were being discussed in the multidisciplinary team (MDT) meeting of the hospital before their treatments were initiated. All patients that were being treated with ELAPE were locally advanced distal rectal tumors that were threatening the CRM or abutting the levators, thus majority of these patients underwent neo-adjuvant chemoradiotherapy with 50.4Gy and oral capecitabine. After neo-adjuvant treatment, patients were restaged with MRI Pelvis and CT scan Chest and Abdomen followed by clinical examination. Decision for surgery was then made. Patients were normally operated 6-8 weeks post neo-adjuvant treatment. Post-operatively the patients were daily screened for signs of infection at the perineal wound during their stay at the hospital, at the time of discharge and on the subsequent visits in the outpatient department. The subsequent visits in the outpatient department were scheduled on the 10th day post-surgery and at 4th week post-surgery. However, more frequent visits were arranged if needed according to the clinical condition of the patient. Afterwards patients were followed up three monthly for year one post-surgery, six monthly for year two and three and yearly for year four and five. On each visit the patients were evaluated by a consultant surgeon.
I Technique
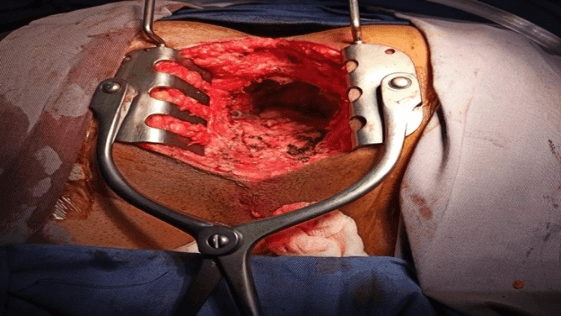
Almost all patients underwent Laparoscopic abdominal part of the operation followed by perineal part performed in prone jack knife position (Figure 1A). The abdominal dissection was completed till coccyx posteriorly and Denonvilliers' fascia anteriorly, further dissection was stopped to prevent specimen wasting and conning. Abdominal drain was placed, omentum brought in the pelvis and a 4 x 12cm raytec gauze was packed in the pelvis. Stoma matured in the left iliac fossa and patient moved to prone jack knife position for perineal part of the operation (Figure 1A).
Figure 1A: Prone jackknife position for perineal part of ELAPE.
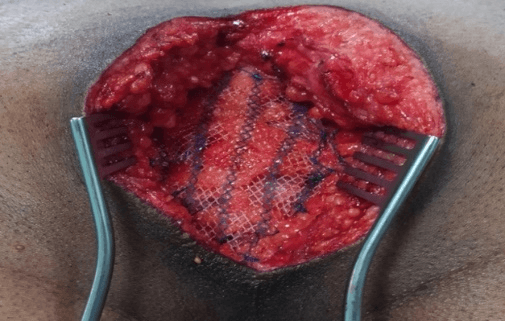
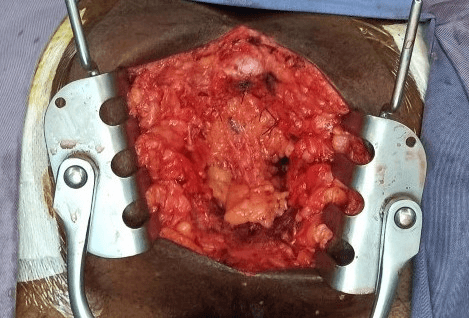
Tear drop incision was made around the anus and first entry was made into the presacral fascia posteriorly, just anterior to the coccyx. The coccyx may or may not be removed at this point. Levator muscles were divided widely on the both sides. Specimen was flipped and anterior dissection was completed under vision and a cylindrical specimen was delivered. During the anterior dissection posterior wall of vagina in females, if involved was removed and defect was closed primarily. Likewise, the prostatic capsule in males was removed if was involved. We routinely use a silicone Foley’s catheter that could always be palpated during anterior dissection to prevent urethral injury. Resection left a considerable perineal defect (Figure 1B). The defect was either re-constructed with a mesh (Figure 1C) or a flap reconstruction was used. Primary closure with Omentoplasty (Figure 1D) was also be performed in some patients. Our early cases were reconstructed with Ultra-pro mesh. However, afterwards we gave up the practice of routine mesh placement and adopted Omentoplasty as the mode of closure. Flap reconstruction was used only selectively.
Figure 1B: Specimen resected and perineal defect.
Figure 1C: Mesh reconstruction of perineal defect.
Figure 1D: Omentoplasty of perineal defect.
II Operative Definitions
i Early Post-Operative Period
Early post-operative period was defined as 30 days post-surgery.
ii Perineal Wound Infection
Perineal wound infection was defined as presence of pus discharge, pain, erythema, tenderness, swelling or deep space infection in the perineal wound.
iii Perineal Wound Dehiscence
Perineal wound dehiscence was defined as partial or complete separation of wound skin with or without infection.
III Analysis
The data was analysed using SPSS for MAC version 26. Descriptive statistics were run, and data was expressed as median along with inter quartile range (IQR). Multivariate analysis using the regression model was done. Chi-square test was performed for categorical, Mann-Whitney U test for non-parametric and student's t-test for parametric variables A p-value of <0.05 was considered significant.
Results
A total of 84 patients underwent ELAPE between January 2014 and December 2019. Various characteristics of the patients are being described in detail in (Table 1A). Median age of the patients was 39 (18-70) years. The study population had a male predominance. The median BMI of the patients was 23 (15-38). Most of the patients belonged to American Society of Anesthesiologists (ASA) group II.
Table 1A: Patient characteristics.
|
Characteristics |
|
|
Age: median (range) |
39 (18 – 70) |
|
Gender n (%) Male Female |
64 (76.2%) 20 (23.8%) |
|
BMI: median (range) |
23 (15 – 38) |
|
ASA classification n (%) I II III IV |
0 (0%) 77 (91.7%) 7 (8.3) 0 (0%) |
|
Duration of symptoms (months): median (range) |
5 (1 – 24) |
|
Distance from anal verge (cm): median (range) |
2 (0 - 6) |
|
CEA: median (range) |
4.05 (0.60 – 192.00) |
|
Albumin (g/dl): median (range) |
4.23 (3.05 – 5.17) |
|
Hemoglobin (g/dl): median (range) |
13.45 (6.80 – 17.80) |
|
Clinical Staging TNM n (%) T1 T2 T3 T4 N0 N1 N2 N3 M0 M1 |
0 (0%) 3 (3.6%) 65 (77.4%) 15 (17.9%) 11 (13.1%) 35 (41.7%) 37 (44.0%) 1 (1.2%) 81 (96.4%) 3 (3.6%) |
|
Neoadjuvant Chemoradiation Given Not Given |
80 (95.2%) 4 (4.8%) |
|
Histopathology Adenocarcinoma Melanoma |
82 (97.61%) 2 (2.38%) |
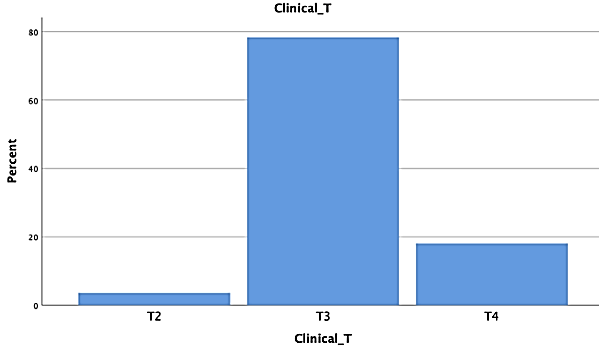
The median duration of symptoms before presentation was 5 (1-24) months. The median distance from anal verge was 2 (0-6) cm. Most of the tumors were T3 and T4 according to American Joint Committee on Cancer (AJCC) TNM classification. The T stage is further being elaborated in the (Figure 2A) with the aid of a bar chart. Neoadjuvant chemoradiation was done in 80 (95.23%) of the patients.
Figure 2A: Clinical T stage of tumors.
Table 1B: Operative variables.
|
Operative Variables |
|
|
Mode of Surgery n (%) Laparoscopic Laparoscopic converted to open Open |
83 (98.8%) 1 (1.2%) 0 (0%) |
|
Positioning in perineal part n (%) Supine Prone Jack Knife |
0 (0%) 84 (100%) |
|
Operative time (minutes) median (range) |
320 (250 – 490) |
|
Blood loss (ml) median (range) |
70 (25 – 600) |
|
Reconstruction n (%) Mesh Flap Omentoplasty |
17 (20.2%) 1 (1.2%) 66 (78.57%) |
|
Drain n (%) Jaxon Pratt Redon Corrugated drain |
4 (4.8%) 77 (91.70) 3 (3.60%) |
|
TME (complete) n (%) |
78 (92.85%) |
|
Intra-operative tumor perforation n (%) |
5(6%) |
|
Extended pelvic resections Prostate capsule resection Partial vaginectomy |
5 (5.92%) 13 (15.5%) |
|
Positive circumferential resection margins (CRM) n (%) |
17 (20.2%) |
In (Table 1B) the operative variables are being discussed. Amongst the studied cohort, 83 (98.8%) of the patients had laparoscopic resection of the abdominal part and all patients had perineal part performed in prone jackknife position. Mesorectum was complete in 78 (92.8%) of the cases. There were five intra-operative tumor perforations. Positive circumferential margins (CRM) was observed in 17 (20.2%) patients. Table 1C describes different variables in pertinence to wound infection. Wound infection was observed in 32(38.09%) of the patients. 5 (5.95%) of the patients developed wound dehiscence. Median day of wound infection detection was day 10. Of those requiring intervention majority were being managed by dressings and antibiotics only. However, six patients needed surgical drainage and debridement. Those managed by surgical debridement underwent secondary suturing. Radiological drain was placed in two, one patient needed gracilis flap and another patient was managed by vacuum assisted closure (VAC). Median hospital stay was 7 (4-22) days.
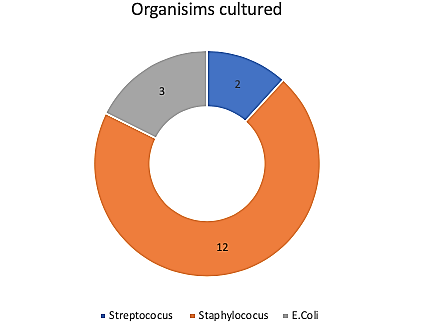
Figure 2B: Pie chart of organisms cultured from infected wounds.
Table 1C: Perineal wound complication data.
|
Perineal wound complication data |
|
|
Perineal wound complication n (%) Wound infection n (%) Dehiscence n (%) |
37 (44.04%) 32 (38.09%) 5 (5.95%) |
|
Post-operative day wound infection detected: median (range) |
10 (5 – 22) |
|
Culture growth n (%) of total infected Positive Negative |
32 + 5 = 37 17 (45.94%) 20 (54.06%) |
|
Intervention n (%) Dressings and antibiotics only Surgical Debridement Radiological drain placement Vacuum assisted closure (VAC) Flap |
32 (100 %) 22 (68.75%) 6 (18.75 %) 2 (6.25%) 1 (3.125 %) 1 (3.125%) |
|
Perineal Hernia |
1 (1.19%) |
|
Hospital stay (days): median (range) |
7 (4-22) |
|
Time to return to adjuvant chemotherapy (if needed) Weeks: median (range) |
5 (4-7) |
The donut chart (Figure 2B) describes the percentages of organisms that were being cultured from the infected wounds. Tables 1D & 1E shows the univariate analysis. On multivariate analysis (Table 1F) Body mass index (BMI) was identified as a significant independent risk factor for infection: BMI (mean ± standard deviation) (adjusted odds ratio [AOR] 1.10; 95% confidence interval [CI] (1.00 – 1.20), p-value (0.045). Hemoglobin (Hb) was marginally statistically significant in logistic regression model: Hb (mean ± standard deviation) adjusted odds ratio [AOR] 0.85; 95% confidence interval [CI] (0.71 – 1.02), p-value (0.09). The correlation of resection margins, albumin and operative time were not statistically significant as independent factors for perineal wound infection. The correlation with intra operative perforations was clinically significant on our clinical observation however, the number of intra-operative perforations were only five. Thus, it was not feasible to run the regression model as the numbers were too low to calculate statistical significance.
Table 1D: Pre-operative characteristics, univariate analysis and p-value.
|
Character |
P value |
|
Age in years |
0.846 |
|
Gender |
0.258 |
|
Demographics |
0.472 |
|
Location of tumor |
0.191 |
|
ASA grade |
0.458 |
|
BMI |
0.002 |
|
Addiction |
0.539 |
|
Comorbids |
0.243 |
|
Clinical T stage |
0.909 |
|
Albumin |
0.846 |
|
Hemoglobin |
0.312 |
|
Neoadjuvant finish date |
0.596 |
Table 1E: Per-operative characteristics, univariate analysis and p-value.
|
Per operative characteristics |
P value |
|
Operative time |
1.00 |
|
Blood loss |
0.093 |
|
Perforation |
0.761 |
|
Mode of surgery |
0.404 |
|
Vaginal resection |
0.515 |
|
Type of drain used |
0.614 |
|
Mode of defect repair |
0.095 |
|
Type of mesh used |
0.141 |
Table 1F: Multivariate logistic regression model.
|
Variables Categories |
Adjusted OR (CI), p value |
|
Body mass index (Mean ± Standard deviation) |
1.10 (1.00 1.20), 0.045 |
|
Hemoglobin (Mean ± Standard deviation) |
0.85 (0.71 1.02), 0.09 |
|
Resection margins |
|
|
R0 |
Ref |
|
R1 |
1.54 (0.60 4.10), 0.40 |
|
Albumin (Mean ± Standard deviation) |
0.74 (0.26 2.11), 0.60 |
|
Operation time (Mean ± Standard deviation) |
1.10 (1.00 1.03), 0.08 |
Discussion
Since its introduction ELAPE is believed to offer better oncological outcomes as a more radical resection can be performed and negative margins can be obtained [1]. However, the extensive resection in the presence of previously radiated perineum paves path for further complications. As majority of the patients undergoing ELAPE are given neo-adjuvant chemoradiotherapy the healing capacity of radiated area is decreased [12]. The wide resection of the levators leave a big defect in the perineum (Figure 1B).
Perineal wound complications after ELAPE have been reported in range of 20-46% of the patients. On literature review (Table 2) three previously done studies have also reported wound complication rates in range of 20-44% [13-15]. The perineal wound complication rate of 44.04% in our reported series falls between the previously reported figures. The uniform use of neoadjuvant chemoradiation might have contributed to our reported higher wound infection rate. A nationwide study that was conducted at Denmark concluded that ELAPE and neoadjuvant chemoradiotherapy were independent risk factors for the development of perineal complications [14]. Following resection there are various methods for dealing with the perineal defect. Either mesh or flaps can be used for the re construction. The perineal wound can be primarily closed as well. However, there are more chances of hernia formation if the defect is primarily closed [16].
Table 2: Literature review of different studies on perineal wound complication rate.
|
Authors |
Type of study |
Sample size |
Perineal wound complication rate |
|
Prytz et al. [13] |
Registry data |
519 |
20% |
|
Asplund et al. [14] |
Registry data |
222 |
21% |
|
Niharka et al. [15] |
Retrospective data |
71 |
42% |
|
Current study |
Retrospective data |
84 |
44% |
In our series 66 (78.57%) were being primarily closed with aid of omentoplasty, the rest were being managed by either mesh or flap. Perineal hernia was reported in one patient. In published data the incidence of perineal hernia has been reported in up to 2% of the patients [11]. The incidence of perineal hernia in our studied cohort was thus less as compared to the published data. However, many patients can have asymptomatic perineal hernia that can be detected on imaging. We plan to upraise this association in detail in a study later on. The time of adjuvant chemotherapy can get adversely effected in cases of perineal wound complications. A recent study concluded that the average time from day of surgery to resumption of adjuvant chemotherapy was between 9 and 11 weeks. In our series the average time of resumption of adjuvant chemotherapy was 5 (4-7) weeks. Resumption of adjuvant chemotherapy in our studied cohort was early as compared to the published data. However, in cases where there was a delayed wound healing or wound complication the time to adjuvant chemotherapy was significantly delayed.
The circumferential resection margins were positive (R1) in 17 (22%) of the patients. The positivity was likely due to bad patient selection. More cases with positive circumferential margins were reported towards the end of the series. It is likely due to more experience with ELAPE and we started attempting more cases that were locally advanced to start with and R0 resection could not have been possible. However, it was attempted, and the results were more R1 resections. This issue has been upraised at our department and we have improved patient selection criteria now. The median hospital stay following ELAPE at our institution was 7 (4-22) days. That was significantly less as compared to the published data [17]. Being a high-volume rectal cancer center and implementation of enhanced recovery programs, we have managed to improve patient outcomes and decrease hospital stay and costs of treatment.
Conclusion
ELAPE is a procedure with significant perineal wound complication rate. Multiple factors contribute to the development of perineal complications. Patients for ELAPE shall be carefully selected and the recognized factors that are shown to cause perineal wound complication shall be corrected if possible. However, if these factors cannot be altered then these patients shall be carefully observed for development of perineal wound complications and prompt detection and intervention shall be done.
Study Limitations
The limitations of the study include a small sample size and retrospective nature.
Conflicts of Interest
None.
Funding
None.
Disclosure
None.
Institutional Review Board Approval
IRB exemption was obtained from IRB cell of Shaukat Khanam Memorial Cancer Hospital & Research center.
Article Info
Article Type
Publication history
Received: Thu 01, Jan 1970Accepted: Thu 01, Jan 1970
Published: Thu 01, Jan 1970
Copyright
© 2023 . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI:
Author Info
Corresponding Author
Figures & Tables
Table 1A: Patient characteristics.
|
Characteristics |
|
|
Age: median (range) |
39 (18 – 70) |
|
Gender n (%) Male Female |
64 (76.2%) 20 (23.8%) |
|
BMI: median (range) |
23 (15 – 38) |
|
ASA classification n (%) I II III IV |
0 (0%) 77 (91.7%) 7 (8.3) 0 (0%) |
|
Duration of symptoms (months): median (range) |
5 (1 – 24) |
|
Distance from anal verge (cm): median (range) |
2 (0 - 6) |
|
CEA: median (range) |
4.05 (0.60 – 192.00) |
|
Albumin (g/dl): median (range) |
4.23 (3.05 – 5.17) |
|
Hemoglobin (g/dl): median (range) |
13.45 (6.80 – 17.80) |
|
Clinical Staging TNM n (%) T1 T2 T3 T4 N0 N1 N2 N3 M0 M1 |
0 (0%) 3 (3.6%) 65 (77.4%) 15 (17.9%) 11 (13.1%) 35 (41.7%) 37 (44.0%) 1 (1.2%) 81 (96.4%) 3 (3.6%) |
|
Neoadjuvant Chemoradiation Given Not Given |
80 (95.2%) 4 (4.8%) |
|
Histopathology Adenocarcinoma Melanoma |
82 (97.61%) 2 (2.38%) |
Table 1B: Operative variables.
|
Operative Variables |
|
|
Mode of Surgery n (%) Laparoscopic Laparoscopic converted to open Open |
83 (98.8%) 1 (1.2%) 0 (0%) |
|
Positioning in perineal part n (%) Supine Prone Jack Knife |
0 (0%) 84 (100%) |
|
Operative time (minutes) median (range) |
320 (250 – 490) |
|
Blood loss (ml) median (range) |
70 (25 – 600) |
|
Reconstruction n (%) Mesh Flap Omentoplasty |
17 (20.2%) 1 (1.2%) 66 (78.57%) |
|
Drain n (%) Jaxon Pratt Redon Corrugated drain |
4 (4.8%) 77 (91.70) 3 (3.60%) |
|
TME (complete) n (%) |
78 (92.85%) |
|
Intra-operative tumor perforation n (%) |
5(6%) |
|
Extended pelvic resections Prostate capsule resection Partial vaginectomy |
5 (5.92%) 13 (15.5%) |
|
Positive circumferential resection margins (CRM) n (%) |
17 (20.2%) |
Table 1C: Perineal wound complication data.
|
Perineal wound complication data |
|
|
Perineal wound complication n (%) Wound infection n (%) Dehiscence n (%) |
37 (44.04%) 32 (38.09%) 5 (5.95%) |
|
Post-operative day wound infection detected: median (range) |
10 (5 – 22) |
|
Culture growth n (%) of total infected Positive Negative |
32 + 5 = 37 17 (45.94%) 20 (54.06%) |
|
Intervention n (%) Dressings and antibiotics only Surgical Debridement Radiological drain placement Vacuum assisted closure (VAC) Flap |
32 (100 %) 22 (68.75%) 6 (18.75 %) 2 (6.25%) 1 (3.125 %) 1 (3.125%) |
|
Perineal Hernia |
1 (1.19%) |
|
Hospital stay (days): median (range) |
7 (4-22) |
|
Time to return to adjuvant chemotherapy (if needed) Weeks: median (range) |
5 (4-7) |
Table 1D: Pre-operative characteristics, univariate analysis and p-value.
|
Character |
P value |
|
Age in years |
0.846 |
|
Gender |
0.258 |
|
Demographics |
0.472 |
|
Location of tumor |
0.191 |
|
ASA grade |
0.458 |
|
BMI |
0.002 |
|
Addiction |
0.539 |
|
Comorbids |
0.243 |
|
Clinical T stage |
0.909 |
|
Albumin |
0.846 |
|
Hemoglobin |
0.312 |
|
Neoadjuvant finish date |
0.596 |
Table 1E: Per-operative characteristics, univariate analysis and p-value.
|
Per operative characteristics |
P value |
|
Operative time |
1.00 |
|
Blood loss |
0.093 |
|
Perforation |
0.761 |
|
Mode of surgery |
0.404 |
|
Vaginal resection |
0.515 |
|
Type of drain used |
0.614 |
|
Mode of defect repair |
0.095 |
|
Type of mesh used |
0.141 |
Table 1F: Multivariate logistic regression model.
|
Variables Categories |
Adjusted OR (CI), p value |
|
Body mass index (Mean ± Standard deviation) |
1.10 (1.00 1.20), 0.045 |
|
Hemoglobin (Mean ± Standard deviation) |
0.85 (0.71 1.02), 0.09 |
|
Resection margins |
|
|
R0 |
Ref |
|
R1 |
1.54 (0.60 4.10), 0.40 |
|
Albumin (Mean ± Standard deviation) |
0.74 (0.26 2.11), 0.60 |
|
Operation time (Mean ± Standard deviation) |
1.10 (1.00 1.03), 0.08 |
Table 2: Literature review of different studies on perineal wound complication rate.
|
Authors |
Type of study |
Sample size |
Perineal wound complication rate |
|
Prytz et al. [13] |
Registry data |
519 |
20% |
|
Asplund et al. [14] |
Registry data |
222 |
21% |
|
Niharka et al. [15] |
Retrospective data |
71 |
42% |
|
Current study |
Retrospective data |
84 |
44% |

References
- Mulsow J, Winter DC (2010) Extralevator abdominoperineal resection for low rectal cancer: new direction or miles behind? Arch Surg 145: 811-813. [Crossref]
- Sun Z, Yu X, Wang H, Ma M, Zhao Z et al. (2015) Factors affecting sphincter‑preserving resection treatment for patients with low rectal cancer. Exp Ther Med 10: 484-490. [Crossref]
- Paty PB, Enker WE, Cohen AM, Lauwers GY (1994) Treatment of rectal cancer by low anterior resection with coloanal anastomosis. Ann Surg 219: 365-373. [Crossref]
- Jung M, Shin US, Ki YJ, Kim Y, Moon S et al. (2017) Is the location of the tumor another prognostic factor for patients with colon cancer? Ann Coloproctol 33: 210-218. [Crossref]
- Delibegovic S (2017) Introduction to Total Mesorectal Excision. Med Arch 71: 434-438. [Crossref]
- Eriksen MT, Wibe A, Syse A, Haffner J, Wiig JN (2004) Inadvertent perforation during rectal cancer resection in Norway. Br J Surg 91: 210-216. [Crossref]
- Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94: 232-238. [Crossref]
- Peirce C, Martin S (2016) Management of the perineal defect after abdominoperineal excision. Clin Colon Rectal Surg 29: 160-167. [Crossref]
- Wiatrek RL, Thomas JS, Papaconstantinou HT (2008) Perineal wound complications after abdominoperineal resection. Clin Colon Rectal Surg 21: 76-85. [Crossref]
- Hoare D, Maw A, Gollins S (2013) Does pre-operative chemoradiotherapy cause wound complications after abdominoperineal excision for rectal cancer? An observational study. Int J Surg 11: 395-399. [Crossref]
- Colov EP, Klein M, Gögenur I (2016) Wound complications and perineal pain after extralevator versus standard abdominoperineal excision. Dis Colon Rectum 59: 813-821. [Crossref]
- Chang CC, Lan Y, Jiang J, Chang S, Yang S et al. (2019) Risk factors for delayed perineal wound healing and its impact on prolonged hospital stay after abdominoperineal resection. World J Surg Oncol 17: 226. [Crossref]
- Prytz M, Angenete E, Ekelund J, Haglind E (2014) Extralevator abdominoperineal excision (ELAPE) for rectal cancer--short-term results from the Swedish Colorectal Cancer Registry. Selective use of ELAPE warranted. Int J Colorectal Dis 29: 981-987. [Crossref]
- Asplund D, Prytz M, Bock D, Haglind E, Angenete E (2015) Persistent perineal morbidity is common following abdominoperineal excision for rectal cancer. Int J Colorectal Dis 30: 1563-1570. [Crossref]
- Aggarwal N, Seshadri RA, Arvind A, Jayanand SB (2018) Perineal Wound Complications Following Extralevator Abdominoperineal Excision: Experience of a Regional Cancer Center. Indian J Surg Oncol 9: 211-214. [Crossref]
- Mjoli M, Sloothaak DA, Buskens CJ, Bemelman WA, Tanis PJ (2012) Perineal hernia repair after abdominoperineal resection: a pooled analysis. Colorectal Dis 14: e400- e406. [Crossref]
- Perry WB, Connaughton JC (2007) Abdominoperineal resection: how is it done and what are the results? Clin Colon Rectal Surg 20: 213-220. [Crossref]
