Early Perceval Valve Thrombosis
A B S T R A C T
We report a case of early thrombosis of a sutureless Perceval valve after aortic valve replacement (AVR). Previous reports described Perceval AV thrombosis between 1-12 months [1, 2]. However, the patient was diagnosed with valve dysfunction 3 days later.
Keywords
Valve thrombosis, aortic valve, perceval
Case Presentation
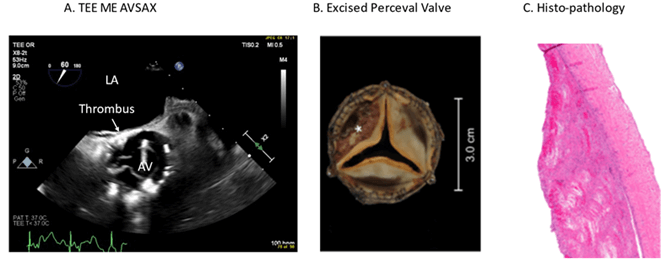
A 67-year-old male with severe, symptomatic bicuspid AV stenosis (Peak velocity: 449 cm/sec, peak gradient: 81 mmHg, mean gradient: 52 mmHg, AV area: 0.86 cm2) underwent AVR using an XL Perceval valve (LivaNova PLC. London, UK). Intra-operative trans-esophageal echocardiographic examination (TEE) showed well sedated tissue valve with no intra or para valvular leaks. He had a history of hypertension, Type-2 Diabetes Mellitus, chronic kidney dysfunction and stroke. The post-operative period was complicated by prolonged ventilation. TEE 3 days post-operatively, showed restriction in the non-coronary (NCC) and right coronary cusps (RCC), an echogenic mass in the NCC and increased AV gradients (Vmax 343 cm/s, Max PG 47 mmHg, Mean PG 16 mmHg) (Figure 1A). The patient underwent urgent redo sternotomy and valve replacement where we found the Perceval valve well seated and without paravalvular leaks. A fresh thrombus compromised the NCC and RCC (Figure 1B & 1C). The Perceval valve was replaced by a 25 mm Magna Ease bioprosthetic valve (Edwards Lifesciences Corp. Irvine, CA, USA). Post-operative course was complicated by prolonged intubation, atrial fibrillation, and neurological dysfunction. Patient was discharged home in stable cardiovascular condition and almost complete neurological recovery. Warfarin 3 mg per day for 3 months was prescribed.
Discussion
Our case of Perceval valve thrombosis, diagnosed on the 3rd day, seems to be an extremely rare occurrence. The largest study (n=47) of Perceval valve thrombosis reported diagnosis of 36-1247 days [1]. This case highlights the importance of echocardiographic investigation after AVR in patients with abnormal post-operative course. There was a good correlation between TEE and surgical findings. Contrary to previous reports, we did not find risk factors for thrombus in our case (use of steroids). This early thrombus supports the debate around the use of anticoagulation after AVR with Perceval valve.
Figure 1: A) 3D mid-esophageal aortic valve view of a thrombus at the non-coronary cusp. B) Photomicrograph of excised Perceval valve cusp with recent laminated thrombus (*) C) Photomicrograph of pericardial bioprosthetic cusp with recent laminated thrombus (H&E original magnification 40x).
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
None.
Ethical Approval
Ethics approval was obtained from Nova Scotia Health Authority Research Ethics Board.
Consent
Patient consent was waived for this study.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 01, Jun 2022Accepted: Thu 16, Jun 2022
Published: Wed 29, Jun 2022
Copyright
© 2023 Hashem Aliter. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2022.01.04
Author Info
Hashem Aliter Daniel Neira Claudio Diquinzio Mathieu Castonguay Keir Stewart
Corresponding Author
Hashem AliterDivision of Cardiac Surgery, Dalhousie University, Halifax, Canada
Figures & Tables
References
1. Dalén M, Sartipy U, Cederlund K, Franco Cereceda A, Svensson A et al. (2017) Hypo-Attenuated Leaflet Thickening and Reduced Leaflet Motion in Sutureless Bioprosthetic Aortic Valves. J Am Heart Assoc 6: e005251. [Crossref]
2. Makkar RR, Fontana G, Jilaihawi H, Chakravarty T, Kofoed KF et al. (2015) Possible Subclinical Leaflet Thrombosis in Bioprosthetic Aortic Valves. N Engl J Med 373: 2015-2024. [Crossref]
