Eagle Syndrome: An Unusual Cause of Stroke Successfully Treated by Angioplasty and Mechanical Thrombectomy
A B S T R A C T
We report a case of a 50-year-old male presenting with right arm weakness and mixed aphasia after motorcycle accident. Basal CT/MR imaging showed absence of acute brain lesions and left internal carotid artery (ICA) wall hematoma at C1-C2 level close to a prominent styloid process. Multiphase CT angiography confirmed ICA dissection and a hypertrophic styloid process compressing the ICA at the same level; ipsilateral intracranial blood flow delay and good collateral circulation were present in the latest CTA phases [1]. Due to Patient neurological status deterioration, with progressive global aphasia and right hemiplegia onset, digital subtraction angiography (DSA) was performed urgently. DSA confirmed the CTA findings together with slowing of cerebral blood flow above the dissection; after mechanical thrombectomy by aspiration followed by balloon angioplasty, good blood flow and vessel caliber restoration were obtained. Post-procedural control and follow-up findings are described together with revision of the recent literature on the possible association between cerebral ischemic stroke and Eagle syndrome.
Keywords
Eagle syndrome, endovascular treatment, post-traumatic acute stroke
Introduction
Temporal styloid process (TSP) is the attachment point of masticatory and swallowing muscles and ligament on the inferior part of temporal bone in the lateral neck space. Its normal length approximately ranged from 20 to 30 mm. Nearby there are many nerves and vessels, such as the carotid arteries. In case of elongation of TSP or calcification of styloid or stylo-mandibular ligament, the overall length of calcified parts is more than 30 mm. The radiographic prevalence of this feature in literature range from 2% to 30%. The clinical presentation caused by compression of elongated TSP on the nearest structures represents the Eagle Syndrome.
Case Description
This study was carried out according with Declaration of Helsinki principles. The patient gave informed consent to publish this work and to report individual data. A 50-year-old male presented to the ED of our institution, two hours after a motorcycle accident. Neurological examination showed fluctuating symptoms with right arm weakness and mixed aphasia (NIHSS 2). These symptoms were not constantly reproducible on examination and the patient was otherwise neurologically intact. His past clinical history was unremarkable, and he was free from any medications.
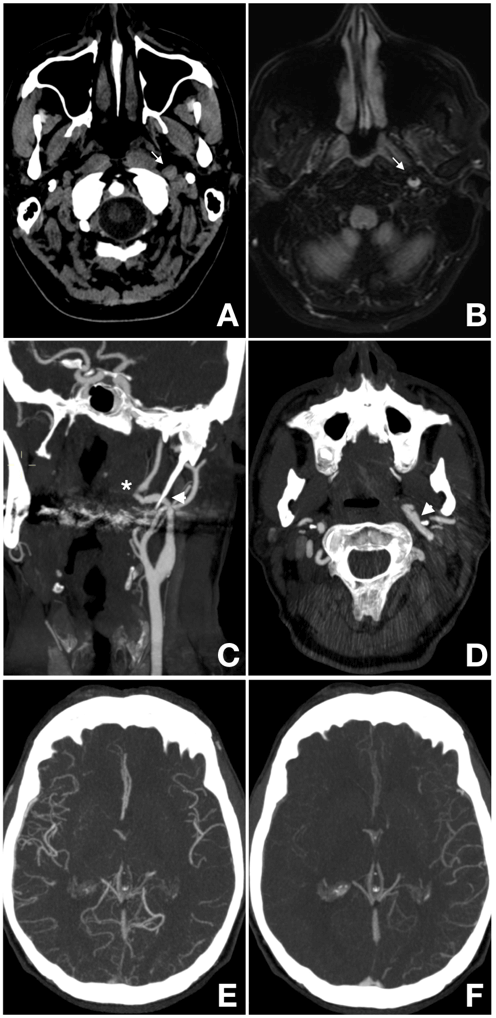
Basal CT and MRI demonstrated absence of acute brain lesions; a left internal carotid artery (ICA) wall hematoma was otherwise visible at cervical C1-C2 level (Figures 1A & 1B). Epiaortic and intracranial CT angiography (CTA), performed in a multiphase fashion, confirmed the left ICA irregularity with caliber reduction at C1-C2 level, consistent with focal vessel dissection (Figures 1C & 1D). At the same level MIP (maximum intensity projection), reconstruction images highlighted a hypertrophic styloid process partially compressing the ICA (Figures 1C & 1D). The left middle cerebral artery (MCA) was open, with circulation time delay and good retrograde collateral circulation demonstrated in the latest CTA phase (Figures 1E & 1F). The clinic and radiologic findings were interpreted as part of “Eagle Syndrome” picture.
Due to the low NIHSS, no indication to endovascular procedure was given, thus the patient was treated with intravenous rt-PA thrombolysis only. Unfortunately, during intravenous rt-PA thrombolysis administration the neurological status worsened, with stable global aphasia and right hemiplegia appearance. At that moment, DSA followed by a possible endovascular treatment was urgently planned.
Figures 1: Pre-operative diagnostic imaging. A-B: Wall hematoma in left C1-C2 tract of ICA (arrow) in Non-Enhanced CT (A) and FLAIR image (B); C-F: Multiphase CTA demonstrates irregular caliber reduction of the ICA (asterisk) near to the point of compression by elongated styloid process (arrowhead). (C: para-coronal MIP image; D: axial MIP image). Intracranial axial MIP images show good collateral leptomeningeal circulation in the left hemisphere (MCA territories), respectively in the first (E) and in the last (F) phase.
Endovascular Procedure
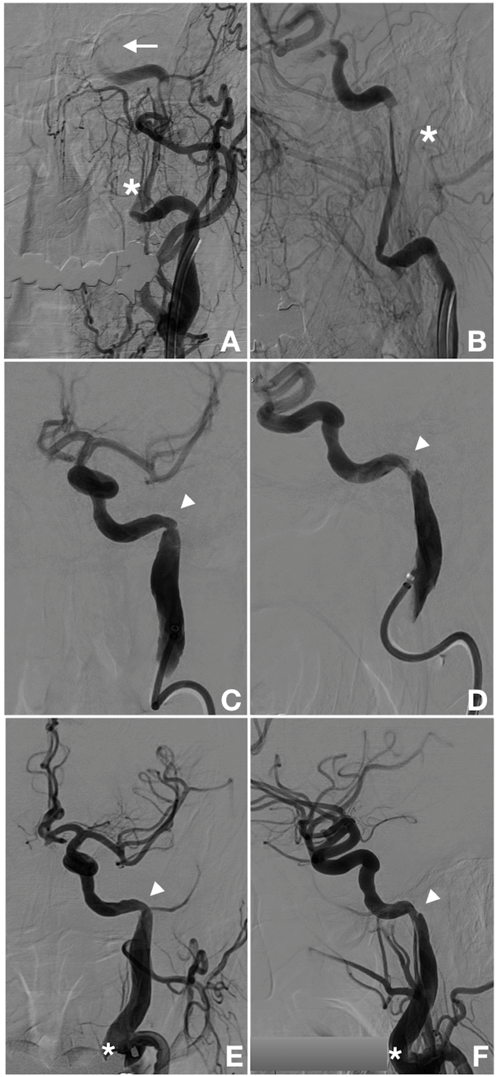
The Digital Subtraction Angiography (DSA) (Allura Philips, The Netherlands) performed immediately after, confirmed the cervical ICA vessel wall dissection, with progressive slowing of the cerebral blood flow in the left MCA (Figures 2A & 2B).
In general anesthesia and systemic heparinization monitored by ACT (activating clotting time), mechanical thrombectomy was performed utilizing a triaxial approach and a large bore aspiration catheter (6 French); through multiple thrombo-aspiration attempts at the dissection site, several red clots were removed. A residual anular stenosis of the proximal cervical ICA was afterwards treated by angioplasty using a compliant balloon (Eclipse 2L Dual Lumen Balloon Catheter, Balt USA), obtaining significant vessel caliber and good antegrade flow restoration (Figures 2C-2F).
Figures 2: Procedural DSA. A-B: Selective left ICA DSA confirms the vessel dissection at C1-C2 level (asterisk) and the slowing of the cerebral blood flow in the left hemisphere (arrow). C-D: Post-thrombectomy left ICA DSA demonstrate residual annular stenosis at the C1-C2 passage (arrowhead). E-F: Left ICA DSA controls after angioplasty with compliant balloon show vessel caliber and flow restoration (arrowhead) and a persistent proximal vessel dissection (asterisk). (A, C, E: Frontal view; B, D, F: Lateral view).
Post-Procedural Controls and Follow-Up
The patient was discharged from the angiosuite in a normalized neurological status (NIHSS 0); the 24-hrs CT scan showed absence of brain lesions. Low-molecular-weight heparin (LMWH) was started, and the patient was discharged few days later under oral anticoagulant regimen (Warfarin).
One month later, the patient experienced headache and vomiting associated with left eye pain and miosis. Brain CT excluded ischemic or hemorrhagic changes, while CTA demonstrated a pseudo-aneurysmal dilation of the cervical ICA (Figure 3). The patient remained under observation for few days, and he was discharged with a slight residual left miosis. Therapy remains unchanged.
Figures 3: One-month follow-up cervical CTA. Persistent left extra-cranial ICA pseudoaneurysm, with a dissection flap at the site of styloid process impingement demonstrated on para-coronal MIP reconstruction (A) and Volume Rendering reconstruction (B).
The neurological evaluation at 6 months follow-up, showed normal neurological status with persistent left eye miosis. No pseudoaneurysm modification was detected at CTA control. The oral anticoagulant therapy was finally replaced by mono-antiplatelet therapy (acetyl salicylic acid, ASA, 100mg/day).
Discussion
The symptomatology related to the ES is due to an elongated styloid process or an ossified stylohyoid or stylo-mandibular ligament that compress the surrounding anatomical structures [2-3]. Depending on the underlying pathogenetic mechanism and on the anatomical structures compressed, symptoms can vary, ranging from cervico-facial pain to cerebral ischemia. Diagnosis is confirmed by radiological findings.
Watt Eagle described the syndrome for the first time in 1937, dividing it into two major clinical subtypes:
i. Classic Syndrome: consisting of unilateral, persistent neck pain, ear pain, dysphasia and dysphonia, tinnitus, odynophagia, persistent sore throat, painful trismus and vertigo. All of these symptoms are attributed to the irritation of cranial nerves V, VII, IX or X, all of which are situated very close to the styloid process.
ii. Stylo-Carotid Syndrome: in which the elongated styloid process is in contact with the cervical ICA, causing compression or dissection of the carotid artery with possible transient ischemic attack or stroke, such as in our case.
Many cases of stylo-carotid variant are reported in literature, which were treated conservatively with anticoagulant or antiplatelets drug therapy only [4-9]. In case of recurrent symptoms, ICA stenting, eventually followed by surgical resection of the elongated styloid process, is reported [10-11]. Anyhow, very few cases were treated in the acute phase by endovascular approach. To our knowledge, our case is one of few reported cases successfully treated in the acute stage [12].
Conclusion
An elongated styloid process or a calcified stylo-hyoid or stylo-mandibular ligaments are not quite rare features in general population [13]. They can cause vessels injury and become the cause of brain ischemia, determining neurological symptoms such as transient ischemic attack or acute ischemic stroke. While it happens, an immediate thorough investigation of the cervical and intracranial circulation should be done in order to perform an endovascular revascularization procedure, if indicated.
Conflicts of Interest
None.
Funding
None.
Abbreviations
ACT: Activating clotting time
ASA: Acetyl salicylic acid
CTA: CT angiography
DSA: Digital Subctraction Angiography
ED: Emergency Department
ES: Eagle Syndrome
ICA: Internal Carotid Artery
LMWH: Low-molecular-weight heparin
MCA: Middle Cerebral Artery
MIP: Maximum Intensity Projection
NIHSS: National Institute of Health Stroke Scale
rt-PA: recombinant tissue Plasminogen Activator
TSP: Temporal Styloid Process
Article Info
Article Type
Case ReportPublication history
Received: Tue 14, Apr 2020Accepted: Tue 12, May 2020
Published: Mon 18, May 2020
Copyright
© 2023 Elisa Ciceri. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2020.02.09
Author Info
Elisa Ciceri Marco Conte Mauro Plebani Piergiuseppe Zampieri Raffaele Augelli
Corresponding Author
Elisa CiceriNeuroradiology Unit, University Hospital of Verona, Verona, Italy
Figures & Tables

References
- Yu AY, Zerna C, Assis Z, Holodinsky JK, Randhawa PA et al. (2016) Multiphase CT angiography increases detection of anterior circulation intracranial occlusion. Neurology 87: 609-616. [Crossref]
- Ayyildiz VA, Senel FA, Dursun A, Ozturk K (2019) Morphometric examination of the styloid process by 3D-CT in patients with Eagle syndrome. Eur Arch Otorhinolaryngol 276: 3453-3459. [Crossref]
- Pigkou M, Anagnostopoulou S, Kouladouros K, Piagkos G (2009) Eagle’s syndrome: a review of literature. Clin Anat 22: 545-558. [Crossref]
- Shindo T, Ito M, Matsumoto J, Miki K, Fujihara F et al. (2019) A Case of Juvenile Stroke due to Carotid Artery Dissection from an Elongated Styloid Process-Revisiting Conservative Management. J Stroke Cerebrovasc Dis 28: 104307. [Crossref]
- Razak A, Short JL, Hussain SI (2014) Carotid Artery Dissection due to Elongated Styloid Process: A Self-Stabbing Phenomenon. J Neuroimaging 24: 298-301. [Crossref]
- Zammit M, Chircop C, Attard V, D'Anastasi M (2018) Eagle’s syndrome: a piercing matter. BMJ Case Rep 11: e226611. [Crossref]
- Aldakkan A, Dunn M, Warsi NM, Mansouri A, Marotta TR (2017) Vascular Eagle's Syndrome: Two Cases Illustrating Distinct Mechanisms of Cerebral Ischemia. J Radiol Case Rep 11: 1-7. [Crossref]
- Qureshi S, Farooq MU, Gorelick PB (2019) Ischemic Stroke Secondary to Stylocarotid Variant of Eagle Syndrome. Neurohospitalist 9: 105-108. [Crossref]
- Sveinsson O, Kostulas N, Herrman L (2013) Internal carotid dissection caused by an elongated styloid process (Eagle syndrome). BMJ Case Rep 2013: bcr2013009878. [Cros sref]
- Torikoshi S, Yamao Y, Ogino E, Taki W, Sunohara T et al. (2019) A Staged Therapy for ICA Dissection Caused by Vascular Eagle Syndrome. World Neurosurg 129: 133-139. [Crossref]
- Smoot TW, Taha A, Tarlov N, Riebe B (2017) Eagle syndrome: a case report of stylocarotid syndrome with carotid artery dissection. Interv Neuroradiol 23: 433-436. [Crossref]
- Ogura T, Mineharu Y, Todo K, Kohara N, Sakai N (2015) Carotid Artery Dissection Caused by an Elongated Styloid Process: Three Case Reports and Review of the Literature. NMC Case Rep J 1: 21-25. [Crossref]
- Gokce C, Sisman Y, Sipahiuglu M (2008) Styloid process elongation or Eagle’s syndrome: is there any role for ectopic calcification? Eur J Dent 2: 224-228. [Crossref]
