Disappearance of Internal Jugular Vein Thrombosis After Use of Edoxaban Following Head and Neck Reconstruction: A Case Report
A B S T R A C T
Internal jugular vein thrombosis (IJVT) is a complication of neck dissection. After head and neck reconstruction, flap congestion due to IJVT may lead to flap necrosis, and early diagnosis and treatment should be considered. We experienced a case of disappearance of IJVT in which edoxaban was administered after free-flap reconstruction, and the entire flap survived. Edoxaban has few bleeding complications and was useful as a single drug approach for IJVT after head and neck reconstruction.
Keywords
Internal jugular vein thrombosis, Head and Neck reconstruction, Edoxaban
Introduction
Internal jugular vein thrombosis (IJVT) is a complication of neck dissection. Its incidence is reported to be 20% to 24.7% 1 day after surgery and 6% to 7.4% between 54 days and 3 months after surgery [1, 2]. Problems associated with IJVT, such as congestion of the free-flap transfer, are extremely rare, occurring in 0.6% to 2.8% of cases [3, 4]. However, if such flap congestion does occur, it may lead to flap necrosis, and early diagnosis and treatment should be considered [5]. We here report a case of IJVT after head and neck reconstruction in which edoxaban administration led to regression of the thrombosis and survival of the flap.
Patient Report
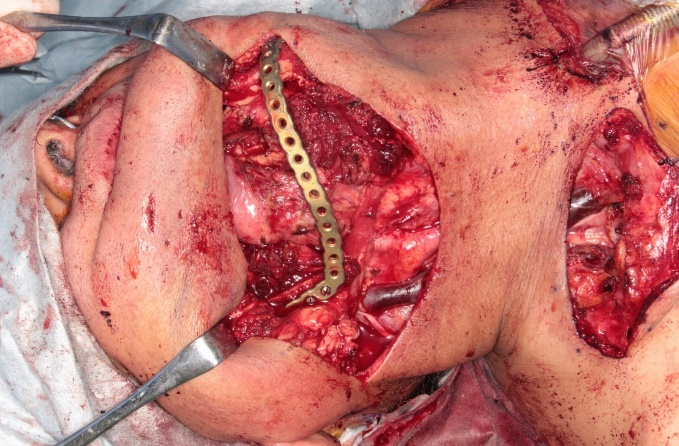
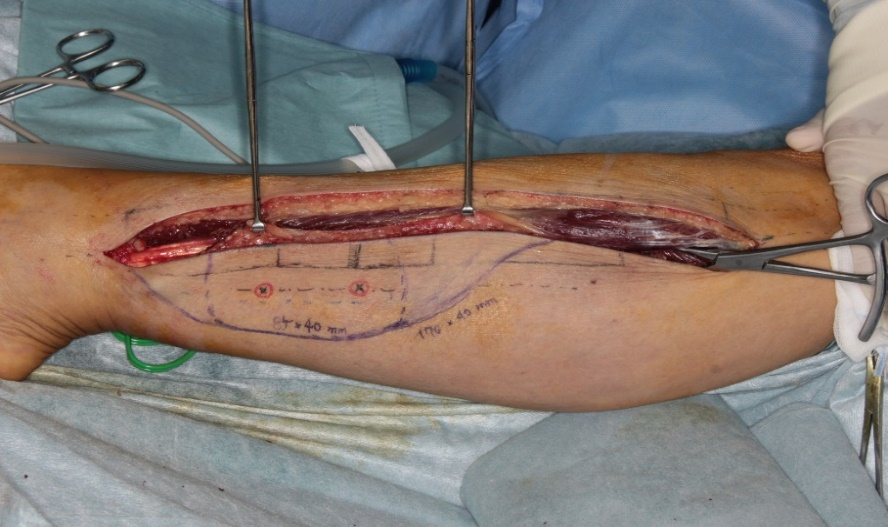
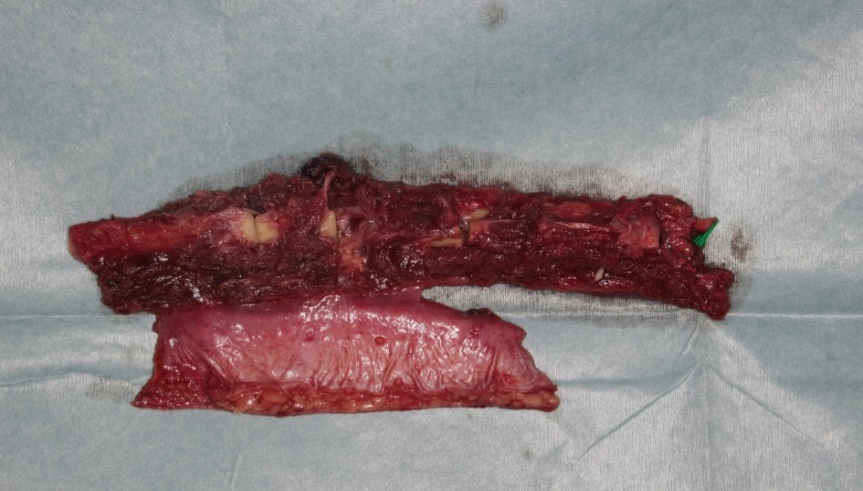
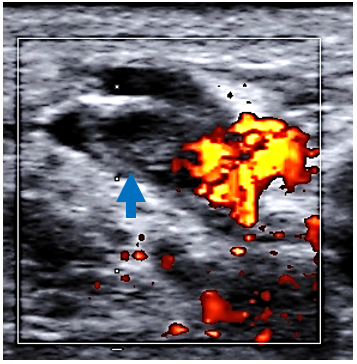
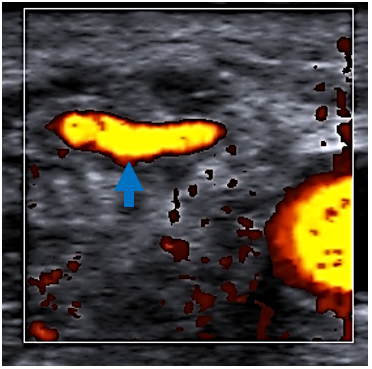
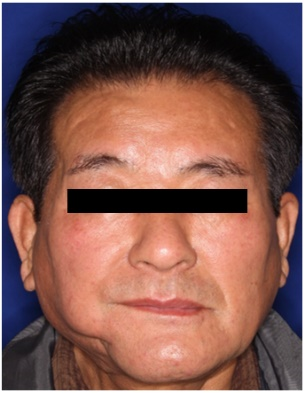
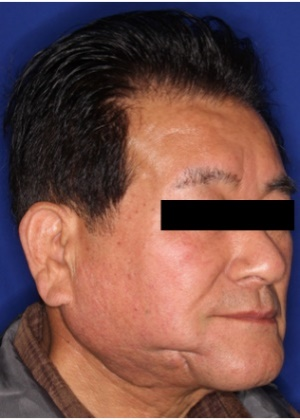
The patient was a 62-year-old man with right lower gingival cancer (T4aN1M0). Right mandibular segmentectomy, total neck dissection, and tracheostomy were performed (Figures 1 & 2), and primary reconstruction was performed with a left fibula osteocutaneous flap. The flap was 17 cm long and 4 cm wide, and the bone, 22.5 cm long (Figures 3 & 4). After bone processing, the bone was fixed as a double barrel (Figure 5). Under the microscope, the right facial artery and fibular artery, and the fibular vein 2 and right external jugular vein were all anastomosed in an end-to-end manner, and the fibular vein 1 and right internal jugular vein were anastomosed in an end-to-side manner (Figure 6). Intraoperative thrombosis of the anastomosis side did not appear, and the flap blood flow was normal (Figure 7). IJVT was confirmed by ultrasonography 12 hours after the surgery (Figure 8). At this time, no congestion of the flap was observed. Edoxaban 30 mg was started, and on the tenth day after surgery, the thrombus in the internal jugular vein was reduced in size (Figure 9). After that, no congestion of the flap was observed, and it survived in its entirety. Contrast-enhanced CT 4 months after the operation revealed no thrombosis in the two fibular veins or the external and internal jugular veins (Figure 10). Therefore, we stopped the use of edoxaban. Despite a slight depression of the mandibular part 8 months postoperatively, the flap was fully engrafted (Figures 11, 12 & 13), and bone resorption was not observed by orthopantomography 1 year postoperatively (Figure 14).
Figure 1: Defect in the right lower gingiva.
Figure 2: Defect in the right lower mandible.
Figure 3: Design of the left fibula osteocutaneous flap.
Figure 4: Elevated fibula osteocutaneous flap.
Figure 5: After bone fixation.
Figure 6: Anastomosis side.
Figure 7: Oral cavity flap.
Figure 8: Color Doppler ultrasound image of the case. Thrombosis of the right internal jugular vein 12 hours postoperatively (blue arrow).
Figure 9: Color Doppler ultrasound image of the case. Most of the right internal jugular vein thrombosis had disappeared 10 days postoperatively (blue arrow).
Figure 10: CT image of the case 4 months postoperatively. The right internal (white arrow) and external (yellow arrow) jugular veins and fibular veins (blue arrow) were patent.
Figure 11: Front view of the patient 8 months postoperatively.
Figure 12: Oblique view of the patient 8 months postoperatively.
Figure 13: Oral cavity flap 8 months postoperatively (white arrow).
Figure 14: Orthopantomography image of the case. The transplanted bone (yellow arrow) was not resorbed 1 year postoperatively.
Discussion
IJVT is one of the complications of cervical dissection, with a reported incidence of 20% to 24.7% 1 day after surgery and 6% to 7.4% between 54 days and 3 months after surgery [1, 2]. Problems associated with IJVT, such as congestion of the free flap, are very rare, the incidence being 0.6% to 2.8% [4]. However, once congestion due to IJVT does occur, relief may not be successful, and flap necrosis may occur. Reports of progression to congestion and necrosis of the flap due to IJVT are seen occasionally. Kubo et al. reported IJVT in 4 of 58 cases of free-flap head and neck reconstruction, two of which resulted in flap necrosis [3]. Miyasaka et al., Fukuiwa et al., and Yang et al. reported that flap congestion caused by IJVT led to flap necrosis in 3 cases, 4 cases, and 3 cases, respectively [4-6]. If the cause of flap congestion is IJVT, there are many reports of flap necrosis, and the rescue of the flap is considered difficult.
Edoxaban is a direct oral anticoagulant (DOAC) first approved in Japan in September 2014 as a treatment for venous thromboembolism (VTE). It is an Ⅹa inhibitor and is a DOAC that has a rapid effect with a maximum blood concentration time (Tmax) of 1 to 3 hours and can be used as a single drug. The use of a DOAC in the initial and maintenance treatment for VTE is also recommended in major overseas guidelines because the administration method is simple, and there are few bleeding complications [7, 8].
Few reports of using edoxaban for IJVT have been published. Toratani et al. started edoxaban after 7 days’ administration of heparin 10,000 units/day for the idiopathic left internal jugular vein, left subclavian vein, and left brachial vein thrombosis [9]. They reported relief of the swelling and no bleeding complications. Shimizu et al. started edoxaban for a right internal jugular vein thrombosis due to an aneurysm in the right aortic arch and confirmed the disappearance of the thrombosis by contrast-enhanced CT 3 months after it was started [10]. However, the use of edoxaban for IJVT after head and neck reconstruction has not been reported. Even if IJVT is recognized early after cervical dissection, improvement in the long term has been reported [1, 2]. However, after head and neck reconstruction, IJVT is not likely to cause flap congestion and necrosis, and treatment is necessary. Many reports recommend anastomosing the flap vein into two systems, such as the internal jugular vein and the external jugular vein, to avoid flap congestion due to IJVT [11-13]. Although we usually try to anastomose two veins in the internal jugular vein and external jugular vein if possible, we experienced a thrombosis in both the internal jugular vein and the external jugular vein in a case in which the flap was congested. As for the second anastomosis to the external jugular vein, it is performed in cases in which the external jugular vein is in good condition.
In cases of IJVT occurring in the early postoperative period, as in our case, edoxaban was selected as the first choice to prevent the development of flap congestion if it had not already occurred. After starting edoxaban, we continue to use it until the disappearance of the thrombosis is shown on ultrasonography, contrast-enhanced CT, and D-dimer values. On the other hand, if IJVT is detected and congestion of the flap is observed, surgery is performed to rescue the flap. At surgery, we try to remove the thrombosis in the internal jugular vein to secure the recipient vein, but if this is difficult, we secure another recipient vein. Thrombosis-occluded internal jugular veins are likely to resume in the long term, and ligation and separation of the internal jugular veins is not essential, considering the risk of pulmonary embolism due to the surgical operation. However, some anticoagulant therapy, such as heparin or edoxaban therapy, should be performed during the operation from the viewpoint of pulmonary embolism prevention and venous anastomosis thrombosis.
In this way, edoxaban alone was administered for IJVT after head and neck reconstruction, and the thrombosis disappeared, and the flap was engrafted. Edoxaban has low bleeding complications and was useful as a single drug approach for IJVT after head and neck reconstruction.
Acknowledgements
We are grateful to Ms. Miyamasu for helpful English proofreading.
Conflicts of Interest
None.
Ethical Approval
I am following the ethical rules of the University of Tsukuba.
Consent
The patient has given permission to publish the paper.
Article Info
Article Type
Case ReportPublication history
Received: Fri 31, Jan 2020Accepted: Mon 17, Feb 2020
Published: Mon 09, Mar 2020
Copyright
© 2023 Masahiro Sasaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2020.01.08
Author Info
Yoichiro Shibuya Akio Nishijima Junya Oshima Kaoru Sasaki Masahiro Sasaki Mitsuru Sekido Yukiko Aihara
Corresponding Author
Masahiro SasakiDepartment of Plastic and Reconstructive Surgery, Faculty of Medicine, University of Tsukuba, Japan
Figures & Tables







References
- Quraishi HA, Wax MK, Granke K, Rodman SM (1997) Internal Jugular Vein Thrombosis After Functional and Selective Neck Dissection. Arch Otolaryngol Head Neck Surg 123: 969-973. [Crossref]
- Wax MK, Quraishi H, Rodman S, Granke K (1997) Internal Jugular Vein Patency in Patients Undergoing Macrovascular Reconstruction. Laryngoscope 107: 1245-1248. [Crossref]
- Kubo T, Haramoto U, Yano K, Kakibuchi M, Takagi S et al. (2002) Internal Jugular Vein Occlusion in Head and Neck Microsurgical Reconstruction. Ann Plast Surg 49: 490-494. [Crossref]
- Fukuiwa T, Nishimoto K, Hayashi T, Kurono Y (2008) Venous thrombosis after microvascular free-tissue transfer in head and neck cancer reconstruction. Auris Nasus Larynx 35: 390-396. [Crossref]
- Miyasaka M, Ichikawa K, Nishmura M, Yamazaki A, Taira H et al. (2005) Salvage operations of free tissue transfer following internal jugular venous thrombosis: a review of 4 cases. Microsurgery 25: 191-195. [Crossref]
- Yang B, Qu Y, Su M, Li J, Li H et al. (2017) Characteristics and surgical management of flap compromise caused by thrombosis of the internal jugular vein. J Craniomaxillofac Surg 45: 347-351. [Crossref]
- Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D et al. (2014) 2014 ESC guidelines on thediagnosis and management of acute pulmonary embolism. Eur Heart J 35: 3033-3069, 3069a-3069k. [Crossref]
- Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D et al. (2016) Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 149: 315-352. [Crossref]
- Toratani M, Hayashi A, Nishiyama N, Nakamura H, Chida R et al. (2017) Thrombosis in an Internal Jugular Vein and an Upper Limb Deep Vein Treated with Edoxaban. Intern Med 56: 1053-1055. [Crossref]
- Shimizu R, Yasu T, Uema A, Hiki T, Matsushita Y et al. (2018) Right internal jugular vein thrombosis caused by aneurysm of right-sided aortic arch. J Cardiol Cases 17: 220-222. [Crossref]
- Kiya K, Kubo T, Seike S, Hosokawa K (2018) Free Flap Survival Despite Internal Jugular Vein Thrombosis in Head and Neck Reconstruction. Plast Reconstr Surg Glob Open 6: e1647. [Crossref]
- de Bree R, van den Berg FG, van Schaik C, Beerens AJ, Manoliu RA et al. (2002) Assessment of patency of the internal jugular vein following neck dissection and microvascular flap reconstruction by power Doppler ultrasound. J Laryngol Otol 116: 622-626. [Crossref]
- Brown DH, Mulholland S, Yoo JH, Gullane PJ, Irish JC et al. (1998) Internal jugular vein thrombosis following modified neck dissection: implications for head and neck flap reconstruction. Head Neck 20: 169-174. [Crossref]
