Differential Diagnosis of a Glenoid Cyst in Omarthrosis: Hemangioma of the Glenoid – Resection and Reconstruction Using Autologous Bone-Graft and Special Implant
A B S T R A C T
Hemangiomas belong to the benign tumors, that can occur in any bone of the human body. The typical localization are the vertebral spine and the skull. There is no reported case of an intraarticular glenoidal hemangioma so far. The current paper presents a case of a 48-year-old female with joint pain that started 2 years before. The clinical manifestations included limited range of motion (ROM) and load dependent, non-load dependent and night pain. Roentgenogram and magnetic resonance imaging (MRI) of the left shoulder showed degenerative changes of the glenohumeral cartilage and a big (11.8mm x 10.3 mm) intraglenoidal mass affecting the joint line. The postoperative pathological diagnosis was that of a cavernous hemangioma. The aim of the present study was to present the imaging presentation of glenoidal hemangioma and to show therapeutic options in case of glenohumeral osteoarthritis (OA) with glenoidal bone loss due to hemangioma. In the present case no recurrence of the hemangioma and no complications of the implant in terms of loosening, infection or consisting were observed.
Keywords
Hemangioma, tumor, glenoid, arthroplasty, shoulder
Introduction
Bone hemangioma is a rare tumor as it accounts to only 1% of the musculoskeletal tumors. It can occur at any part of the body and mostly affect the vertebral column and the skull. At first, they appear as an asymptomatic mass, but can cause pain when growing. Commonly it affects patients between 40 and 60 years of age. Gender affection is M: F 1:2 and it is often diagnosed as an incidental finding during imaging. Treatment options for bone hemangioma are supervised neglect or complete resection of the tumor with subsequent treatment of the remaining bone lesion. Treatment of choice for advanced omarthrosis is arthroplasty. Depending on the condition of the rotator cuff and the bone loss this is either an anatomic or a reverse total shoulder arthroplasty. In order to achieve a good functional result and long-term survival of the implant the restoration of the joint line and correction of glenoid bone loss is mandatory. The classification of glenoid morphology as first described by Walch et al. is the gold standard in terms of treatment decisions.
Case Presentation
In October 2018 a 48-year-old female presented at our clinic who had been complaining about load dependent left shoulder pain for two years. The patient already received surgical intervention such as subacromial decompression elsewhere 14 months before without improvement after long rehabilitation. The patient was very active in sports, such as horse riding and fitness training. At the time of presentation, the patient complained about pain during activities of daily living, night pain and pain at rest. The main clinical findings were a limited active ROM and a painful arc of motion. Active flexion was 120°, abduction 120°, external rotation 0° and internal rotation to the gluteal region. Passive flexion was 140°, abduction 140°, external rotation 20° and internal rotation to the lower lumbar spine at the level of L5. Glenohumeral abduction was 70°. There were no clinical signs of impingement or rotator cuff tear. Force measurement was 4-5/5 for all muscle groups.
Figure 1A: Preoperative roentgenogram ap. White arrow illustrating the hemangioma.
Figure 1B: Preoperative roentgenogram axial. White arrow illustrating the hemangioma.
The left shoulder was investigated using radiography (Figures 1A & 1B), which revealed OA (grade I according to Samilson) with an acromio-humeral distance of 12 mm [1]. Note the intraglenoidal cyst in the lower third of the glenoid in relation to the glenoidal articular surface (white arrow).
Figure 2A: Preoperative MRI ap. White arrow illustrating the hemangioma.
Figure 2B: Preoperative MRI parasagittal. White arrow illustrating the hemangioma.
Figure 2C: Preoperative MRI transversal. White arrow illustrating the hemangioma.
The MRI (Figures 2A-2C) revealed advanced degenerative changes of the hyaline cartilage at the humeral head and at the glenoid. Posterior decentering of the humeral head was noted. A large glenoid cyst of 11.8 mm x 10.3 mm in the transverse plane was detected with breaches to the cortex. No signs of a rotator cuff tear or advanced muscular atrophy or fatty degeneration were observed. Glenoid bone loss was classified to be low without consideration of the glenoid cyst and the glenoid deformity was classified to be Walch type A2 [2]. Considering the classifications of glenoid bone loss for revision arthroplasty according to Williams and Antuna the prevailing defect was categorized as S-R+V+ and as a central severe contained defect [3, 4].
Preoperatve planning led to the decision to perform a one stage procedur with excision of the cyst, glenoid bone grafting with autologous bone and implantation of an anatomical shoulder endoprosthesis with a special glenoid implant. The latter consists of a modular peg made of trabecular titanium and a glenoid base plate of titanium both adaptable in size. With this implant optimal form fitting and bone ingrowth was expected to be provided for secure fixation and good primary stability. The operation was performed in beach chair position using a deltoideo-pectoral approach. After resection of the humeral head the glenoid cavity was exposed. The gleonid cyst was situated in the centre of the glenoid cavity and resected under direct vision (R1). The bone was curetted into healthy trabecular bone. The remaining defect was filled with autologous bone from the humeral head.
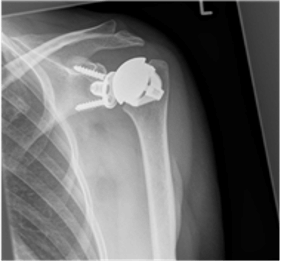
The implant was sized in line with the preoperative planning and the baseplate with the modular trabecular titanium peg was press-fit inserted and secured with two 6.5 mm cancellous screws. The pathological examination of the 1.5 cm measuring excidate revealed a fibrosated connective tissue with aspects of lamellar bone, focal haemorrhage, cavernous cavities and intraluminar extravasation of erythrocytes. The final diagnosis was that of a benign cavernous hemangioma of the glenoid. The patient followed a patient-specific rehabilitation program which included passive mobilisation for the first 2 weeks with a maximum of 90° flexion, 60° abduction, 45 internal rotation and 10° external rotation. The following 4 weeks consist of passive mobilisation with a maximum of 90° flexion, 70° abduction, 70° internal rotation and 20° external rotation. A careful assisted active mobilisation is allowed during this phase. From week 7 the amount and difficulty of motion was increased gradually. The imaging findings after one year follow up (Figures 3A & 3B) showed a good alignment of the implant without signs of loosening or fracture. After one-year follow-up the patient showed an active ROM of 120° flexion, 110° abduction, 45° external rotation and internal rotation to L5 without significant reduction in activities of daily living.
Figure 3A: Postoperative roentgenogram ap.
Figure 3B: Postoperative roentgenogram axial.
Discussion
Hemangioma of the glenoid is an uncommon benign tumor and to the best of our knowledge, no cases have been reported so far. The prognosis of hemangioma is good without high rates of recurrence [5]. This case shows that it should be considered as a differential diagnosis of osteoarthritic cysts in the setting of advanced omarthrosis. In this case the treatment included surgical resection and implantation of a special implant due to bone loss after glenoidal excision of the hemangioma. The decision for a one-stage procedure was based on the MRI findings without any sign of malignancy. The lesion could have easily been overlooked and taken for an arthritic cyst or ganglion, which would have been the differential diagnosis of choice. It needs to be noted, that in cases of malignancy a much more aggressive approach must have been undertaken. In that case the aim would have been a wide resection and a two-stage final procedure after establishing the final diagnosis, the prognosis and a treatment plan that could have included adjuvant chemotherapy or radiation.
The goal of therapy in this special case is not only the adequate resection of the benign tumor mass but also the correct and good fixation of the implant. The reduced impairment after reverse shoulder arthroplasty in humeral tumorous lesion has been shown already [6]. The special modular glenoid implant made of trabecular titanium (SMR Axioma, Lima SPO, Italy) was used to provide secure glenoidal fixation despite of the glenoid defect after the resection of the hemangioma. The advantage of the used system is the strong fixation guaranteed by the trabecular titanium design and the screws as well as the central peg which go past the central defect and therefore provide firm seating. Good primary stability is therefore provided which allows early rehabilitation. This case shows, that the implantation of a glenoid component can technically be performed even in cases of a bigger bone loss due to a benign tumor mass. We suggest this procedure only in case of being absolutely sure about the dignity of the tumor and if the intraoperative finding of the incidental mass appears benign. Any reasonable doubt in imaging or intraoperative presentation should cause a switch to a procedure in a tumor-like manner.
Malhas et al. showed the efficiency of the glenoidal reconstruction using the same implant (Axioma, Lima SPA, Italy) in gross defects. According to the authors the use of a metal baseplate with a trabecular titanium surface in conjunction with autologous bone can be seen as a reliable technique of addressing glenoid bone defects with an observed success in over 90%. They showed an integration rate of the implant in 93% with CT scan analysis 3-6 months postoperatively [7]. In spite of the higher complication rate of anatomical shoulder arthroplasty (ASA) the authors describe the performed method as a reliable technique especially in central glenoid defects as found in this case. It is reported that the restoration of the joint line and correction of retroversion play an important role for the success of ASA [7].
Conclusion
Intraarticular hemangioma is a very rare tumor that can occur in conjunction with an arthrotically changed glenohumeral joint. The reconstruction with autologous bone-graft and a special implant with porous titanium after tumor resection leads to good clinical results even in a glenohumeral joint with OA and gross bone defect after hemangioma resection. The performed technique provides sufficient intraosseous fixation and integration.
Funding
None.
Author Contributions
MJ wrote the manuscript. MFF kept patient records. JK operated on the patient and reviewed the manuscript.
Article Info
Article Type
Case ReportPublication history
Received: Thu 30, Jan 2020Accepted: Wed 19, Feb 2020
Published: Wed 26, Feb 2020
Copyright
© 2023 Marius Junker. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.01.04
Author Info
Jörn Kircher Marius Junker Milad Farkhondeh-Fal
Corresponding Author
Marius JunkerOrthopedic University Hospital Friedrichsheim, Frankfurt am Main, Germany
Figures & Tables






References
- Samilson RL, Prieto V (1983) Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 65: 456-460. [Crossref]
- Walch G, Badet R, Boulahia A, Khoury A (1999) Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty 14: 756-760. [Crossref]
- Antuna SA, Sperling JW, Cofield RH, Rowland CM (2001) Glenoid revision surgery after total arthroplasty. Journal Shoulder Elbow Surg 10: 217-224. [Crossref]
- Williams GR Jr, Ianotti JP (2007) Options for glenoid bone loss: composites of prosthetics and biologics. J Shoulder Elbow Surg 16: S267-S272. [Crossref]
- Verbeke SL, Bovée JV (2011) Primary vascular tumors of bone: a spectrum of entities? Int J Clin Exp Pathol 4: 541-551. [Crossref]
- De Wilde L, Boileau P, Van der Bracht H (2011) Does reverse shoulder arthroplasty for tumors of the proximal humerus reduce impairment? Clin Orthop Relat Res 469: 2489- 2495. [Crossref]
- Malhas AM, Granville Chapman J, Robinson PM, Brookes Fazakerley S, Walton M et al. (2018) Reconstruction of the glenoid using autologous bone-graft and the SMR Axioma TT metal-backed prosthesis: the first 45 sequential cases at a minimum of two years follow up. Bone Joint J 100-B: 1609-1617. [Crossref]
