Diabetic Retinopathy: Complications Associated with Treatment and the Way Out
A B S T R A C T
Objective: Elevation in blood sugar level damages the blood vessels of retina leading to a condition called diabetic retinopathy (DR). The treatment of DR is a critical factor as the condition is very difficult to target at early stage.
Key Findings: Advancements in the field of drug delivery and introduction of nanotechnology have made way out to treat DR and to solve the problem associated with its treatment. The researchers have recommended that there is need of new treatments which are based on the proper understanding of the mechanism of the disease and its pathophysiology.
Summary: The condition of diabetic retinopathy leads to blurred vision and ultimately loss of vision. The treatment involves control of blood sugar levels, surgery and medications like anti-VEGF. The Nano technological systems are so tiny and can cross the barriers of eye thus improving the bioavailability and permeability of drugs. Researches have been done in the field of nanotechnology and the advancements have suggested that it can be used in the treatment of DR.
Keywords
Diabetic retinopathy, treatment, nanotechnology
Graphical Abstract
Introduction
Eyes are one of sense organs which are responsible for vision. They detect the light and then convert it in electrochemical signals. These signals are then transmitted to the brain through optic nerve. The signals are then converted into the images at the retina [1].
I Components of Eyes
Human eye is very complex organ which contains many subparts [2]. The parts and its functions are discussed in the (Table 1).
Table 1: Parts of human eye and functions.
|
Parts of eyes |
Description |
Function |
|
Cornea |
Front part Transparent and convex |
Refraction of light |
|
Iris |
Pigmented |
Controls the quantity of light |
|
Lens |
Transparent Bi-convex |
Focuses light on the retina |
|
Retina |
Lining in the back of eye |
Contains photoreceptors |
|
Optic nerve |
Bundle of sensory neurons |
Transport signals to the brain |
II Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes in which the retinal blood vessels are affected leading to blurred vision. Retina is a light sensitive tissue at back lining of eye which detects light, converts it to signals and sends the signal to the brain through optic nerve [3]. DR is the most common cause of vision loss in people suffering from diabetes. Elevation in the blood sugar level damages the small blood vessels of retina which ends up leaking or swelling of vessels. This leakage and swelling in blood vessels lead to increased release of cytokines and growth factors. The growth factors increase the formation of blood vessels in that area causing angiogenesis and ultimately vision loss [4].
III Stages of DR
There are 4 stages in DR:
i. Mild nonproliferative retinopathy: Earliest stage in which small swellings in the blood vessels occurs leading to leakage.
ii. Moderate nonproliferative retinopathy: Second stage of DR in which blood vessels swell and gets damaged due to which the blood supply to retina is affected.
iii. Severe nonproliferative retinopathy: Third stage in which the blood vessels are blocked and leading secretion of growth factor which signals to generate new blood vessels.
iv. Proliferative diabetic retinopathy: This is the last stage where DR has taken over the retina. New blood vessels are generated which are very fragile and prone to leakage and bleeding [5].
Mechanism of Diabetic Retinopathy
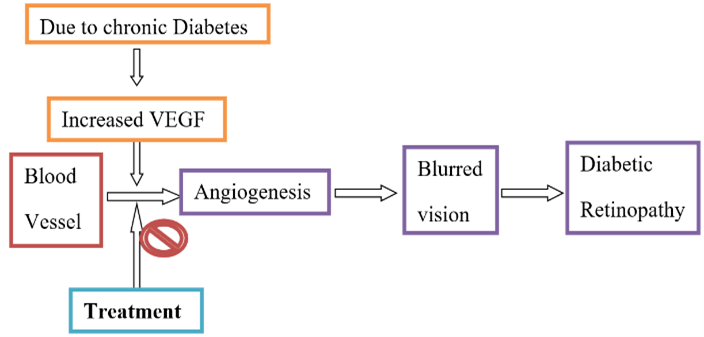
Elevation in high sugar glucose levels weakens and damages the small blood vessels of retina [6]. This may cause haemorrhages, exudates and even swelling of the retina leading to decreased supply of oxygen leading to activation of other pathways which increases the level of cytokines and VEGF in that area [7]. Increased level of VEGF causes neural dysfunction and increased vascular permeability leading to DR and ultimately vision loss. The whole process is briefly shown in (Figure 1) [8].
Figure 1: Mechanism of diabetic retinopathy.
Symptoms
There are no visual symptoms until the disease advances. Edema and leakage results in blurred vision, pain and other complications [9]. Figure 2 depicts some symptoms of DR.
Figure 2: Symptoms of DR.
Risk Factors for Diabetic Retinopathy Include
The diabetic retinopathy is very crucial in cases of elevation of diabetes. There are also other factors which can lead to DR [10]. Some of the risk factors of DR are discussed in (Table 2).
Table 2: Risk factors.
|
Factors |
Effect on DR |
|
Diabetes |
Increased level of diabetes → increased risk of DR. |
|
Race |
Hispanics and African Americans |
|
Medical conditions |
Elevation in cholesterol |
|
Pregnancy |
Gestational diabetes is also prone to retinopathy. |
Statistics of DR
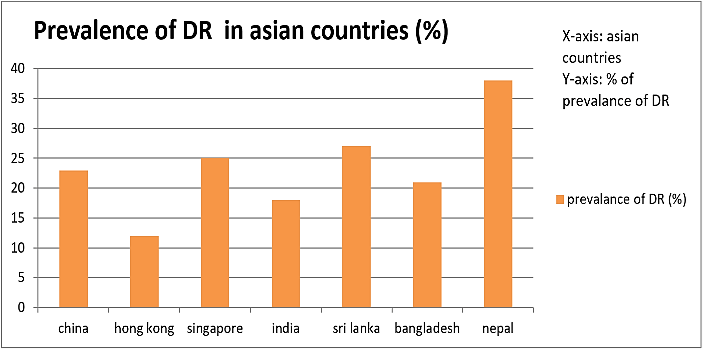
Diabetic retinopathy (DR) is a leading cause of vision-loss globally. Of an estimated 285 million people with diabetes mellitus worldwide, approximately one third have signs of DR and of these, a further one third of DR is vision-threatening DR, including diabetic macular edema (DME). These estimates are expected to rise further due to the increasing prevalence of diabetes, ageing of the population and increasing of life expectancy of those with diabetes [11]. Figure 3 depicts the prevalence of DR in Asian countries in past few years.
Figure 3: Prevalence of DR in Asian countries, china shows 23% in 2012, Hong Kong shows 12.1% in 2014, Singapore shows 30.4 in 2012, India shows 18% in 2009, Sri Lanka shows 27.4% in 2014, Bangladesh shows 21% in 2013, Nepal shows 38% in 2014.
The statistical data shows that the prevalence of DR in Asian countries in past few years has shown that there is need for proper treatment in DR treatment.
Current Medications for DR
The treatment of DR involves vitrectomy, laser surgery, medical control and medication [4]. The treatments of DR are discussed in (Table 3).
Table 3: Treatment of DR.
|
Treatment |
Details |
|
Vitrectomy |
Removal of the vitreous gel |
|
Laser surgery |
Use of laser heat to seal leaking blood vessels in the retina |
|
Medical control |
Proper diet and regular checkups |
|
Medicines |
anti-VEGF medication |
The available treatments are not so affective for complete cure of DR [3]. Some of the reasons are discussed in the (Table 4).
Table 4: Limitations of the treatments available for DR.
|
Treatment |
Limitations |
|
Vitrectomy |
It becomes too late for vitrectomy in many cases and also the vision may decline even after the procedure |
|
Laser surgery |
Costly and uncomfortable for patient as a very bright light is flashed in the patient’s eye |
|
Medical control |
Not effective specially in case where the DR is already residing |
|
Medicines |
Painful and patient incompliance occur as injections and shots have to be taken |
The detection of DR is possible only at the third stage because till now the symptoms are latent and cannot be diagnosed [12]. The limitations in the treatment of conventional dosage form are a matter of concern and have made researchers to advance the treatment [13]. The major problem in the treatment of DR is that the disease can be diagnosed only in the advanced stage. If the problem is detected in the early stage then most of the problems can be solved. The advancements in the DR treatment are mainly focused on decreasing the dose and increasing the efficacy and targeting [14]. The treatment of diabetic retinopathy is mainly focused on decreasing the growth factor thus inhibiting the further steps of blurred vision [15]. Figure 4 depicts the site of action for the treatment.
Figure 4: Site of action for the treatment of DR.
The anti-VEGF drugs are used to decrease the level of VEGF in the region. These agents are injected intravitreally in form of shots. The treatment of DR requires repeated and long-term therapy leading to ocular and systemic complications [16]. Inflammation and haemorrhage may occur in the ocular region which results in patient discomfort. So, there is a need of advancements in the field of treatment of diabetic retinopathy [17].
Advancements in Ocular Delivery
Several advancements have been made in the field of ocular delivery of drug. Some of them are discussed below [18].
I Gel Technologies
Gel formulation increases the concentration of drug on the surface and thus enhances the therapeutically efficacy of drug. As compared to the other drug delivery system in form of solution, the gel provides prolonged delivery to the site improving dosing compliance.
II Nanotechnologies
These provide many advantages over conventional suspensions like increased absorption due to increased surface area and tissue exposure. This system also facilitates the targeting of drug by using proper material to formulate it.
III Iontophoresis
It is an invasive method that propels the charged compounds into ocular tissues by using a small electrical current similar charge to the drug and creates repulsive electromotive forces. This system is beneficial for diseases like fungal keratitis, uveitis, retinitis, retinoblastoma, proliferative vitreoretinopathy and various retinal degenerations. Pre-clinical and clinical studies have demonstrated that there is 100-fold increase in drug bioavailability when compared with topical drops.
IV Microneedles
Microneedles inserted into the cornea resulted in 60-fold increase in drug concentration in the anterior chamber when applied topically. Larger microneedles have been also tested for delivery of drugs to the anterior suprachoroidal space.
V Contact Lenses
Contact lenses have been used for years as a type of sustained release drug delivery system. The drug is allowed to release to the ocular surface once the contact had been placed on the eye. Although delivery of a drug via a contact lens does improve the contact time of the drug compared with topical eye drops, drugs released by a contact lens results in a burst of drug at therapeutic levels only for a few hours.
VI Eye Misters and Microdroplets
Eye misters and microdroplet improved compliance and possibly ocular drug penetration. In one study, an ultrasonic nebulizer was used to create a mist of vitamin B12 that was delivered to the ocular surface in humans and compared with a control group that received a topical eye drop of vitamin B12. Twelve hours later, aqueous humor was collected and analysed for B12 concentrations. None of those receiving eye drops had detectable vitamin B12 in the aqueous humor; however, 29% in the nebulizer group had detectable vitamin B12 concentrations. This suggests that the small particle size, increased surface area of the eye treated, and possibly increased contact time obtained from an eye mist may provide better ocular drug delivery than eye drops.
Pictorial Representation of the Site of Action of Different Drug Delivery Systems
Summary of site of action of different delivery systems is picturized in (Figure 5).
Figure 5: The noninvasive methods for drug delivery to ocular sites are droplets, gel and nanotechnology and deliver the drug to the surface of eye. The iontophoresis and microneedles are invasive methods which causes patient incompliance and interference in vision. The contact lenses and the implants are methods which can provide sustained drug delivery and are suitable for long term therapies. There is a need for a drug delivery system in treatment of diabetic retinopathy which is noninvasive as well as can provide sustained drug delivery.
Nanotechnology is modification and advancements in matter at the atomic level. These carrier systems can deliver the drug more efficiently and potentially providing patient compliance [19]. These carrier systems can be modified and engineered to target the cell and increase the efficacy protecting the healthy cell. Researches are focusing on the effectiveness of nanocarriers in the delivery of anti-VEGF to the ocular site [20]. Researchers have demonstrated that nanocarriers can be used to increase the targeting and efficacy as well as to decrease the side effects and dose [21]. The nanotechnology is a method which is noninvasive and can provide sustained delivery when they are inserted in the right form.
In-Situ Implants
Ocular implants delivers constant drug directly to the site of disease and minimizes systemic side effects. These are classified as biodegradable (i.e., eroding) and nonbiodegradable (i.e., noneroding). Biodegradable implants have the advantage of being able to be fashioned into various shapes and they do not require removal. Nonbiodegradable implants have the advantage of steady, controlled release of a drug for potentially long periods of time (i.e., years) and the disadvantage of removal and/or replacement when the drug is depleted. The targeted disease process dictates the site and placement of the implant. In general, episcleral implantation is used for the treatment of anterior segment disease, whereas intrascleral, suprachoroidal and intravitreal placement of implants target posterior segment disease.
Figure 6: Advantages of In-situ implant.
Clinical Data
Some clinical works regarding to the treatment and advancements in the diabetic retinopathy have been discussed below in (Table 5).
Table 5: Summary of clinical trials in field of Diabetic retinopathy treatment.
|
Clinical trials |
Results |
References |
|
Sustained delivery Bevacizumab vitreous implants: long-term benefit in patients with chronic diabetic macular edema [22]. |
In patients with chronic DME, implants releasing FAc 0.2 μg/day provides substantial visual benefit for up to 3 years and would provide an option for patients who do not respond to other therapy. |
Cunha-Vaz et al. |
|
Sustained ocular delivery of Bevacizumab by an intravitreal insert |
The FA intravitreal inserts provide excellent sustained intraocular release of FA for > or = 1 year. Although the number of patients in this trial was small, the data suggest that the inserts provide reduction of edema and improvement in BCVA in patients with DME with mild effects on intraocular pressure over the span of 1 year [23]. |
Campochiaro et al. |
|
Safety and efficacy of intraoperative intravitreal injection of triamcinolone acetonide injection after phacoemulsification in cases of uveitic cataract |
A single intraoperative intravitreal injection of triamcinolone acetonide seemed to be a safe and efficacious route of steroid delivery during phacoemulsification in patients with chronic idiopathic anterior uveitis or intermediate uveitis and is recommended as a substitute for postoperative oral steroid administration. |
Dada et al. |
|
State of the art clinical efficacy and safety evaluation of N-acetylcarnosine dipeptide ophthalmic prodrug. Principles for the delivery, self-bioactivation, molecular targets and interaction with a highly evolved histidyl-hydrazide structure in the treatment and therapeutic management of a group of sight-threatening eye diseases [24]. |
The results of this study provide a substantial basis for further evaluation of N-acetylcarnosine eye drops patented by IVP in the treatment and prevention of visual impairment in the temporal cross-sections of an older population several years apart [25]. In the number of promotion studies this ophthalmic drug showed experimental and clinical potential for the non-surgical treatment of age-related cataracts [26]. |
Babizhayev et al. |
|
N-acetylcarnosine lubricant eyedrops possess all-in-one universal antioxidant protective effects of L-carnosine in aqueous and lipid membrane environments, aldehyde scavenging, and transglycation activities inherent to cataracts: a clinical study of the new vision-saving drug N-acetylcarnosine eyedrop therapy in a database population of over 50,500 patients [27]. |
accumulated study data demonstrate that the IVP-designed new vision-saving drugs, including N-acetylcarnosine eyedrops, promote health vision and prevent vision disability from senile cataracts, primary open-angle glaucoma, age-related macular degeneration, diabetic retinopathy, and aging [28, 29]. N-acetylcarnosine eyedrop therapy is the crown jewel of the anti-aging medical movement and revolutionizes early detection, treatment, and rejuvenation of aging-related eye-disabling disorders. |
Babizhayev et al. |
Conclusion
The diabetic retinopathy is at very crucial stage and requires attention for the treatment and advancements. The treatments available for DR are very problematic and lead to patient incompliance. There is a need of proper treatment for the DR to avoid the case of surgery and vitrectomy. The advancements in nanotechnology have opened ways for treatment of drug without causing much discomfort to patient. The In-situ implants can be used to provide long term therapy and to decrease the frequency of dosing. The advantages of In-situ implants in drug delivery have made it a potential target for research and development.
Article Info
Article Type
Review ArticlePublication history
Received: Fri 09, Oct 2020Accepted: Mon 19, Oct 2020
Published: Thu 31, Dec 2020
Copyright
© 2023 Saurabh Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDMC.2020.02.04
Author Info
Corresponding Author
Saurabh SharmaProfessor and Head of School, School of Pharmaceutical Sciences, CT University, Ludhiana, Punjab, India
Figures & Tables
Table 1: Parts of human eye and functions.
|
Parts of eyes |
Description |
Function |
|
Cornea |
Front part Transparent and convex |
Refraction of light |
|
Iris |
Pigmented |
Controls the quantity of light |
|
Lens |
Transparent Bi-convex |
Focuses light on the retina |
|
Retina |
Lining in the back of eye |
Contains photoreceptors |
|
Optic nerve |
Bundle of sensory neurons |
Transport signals to the brain |
Table 2: Risk factors.
|
Factors |
Effect on DR |
|
Diabetes |
Increased level of diabetes → increased risk of DR. |
|
Race |
Hispanics and African Americans |
|
Medical conditions |
Elevation in cholesterol |
|
Pregnancy |
Gestational diabetes is also prone to retinopathy. |
Table 3: Treatment of DR.
|
Treatment |
Details |
|
Vitrectomy |
Removal of the vitreous gel |
|
Laser surgery |
Use of laser heat to seal leaking blood vessels in the retina |
|
Medical control |
Proper diet and regular checkups |
|
Medicines |
anti-VEGF medication |
Table 4: Limitations of the treatments available for DR.
|
Treatment |
Limitations |
|
Vitrectomy |
It becomes too late for vitrectomy in many cases and also the vision may decline even after the procedure |
|
Laser surgery |
Costly and uncomfortable for patient as a very bright light is flashed in the patient’s eye |
|
Medical control |
Not effective specially in case where the DR is already residing |
|
Medicines |
Painful and patient incompliance occur as injections and shots have to be taken |
Table 5: Summary of clinical trials in field of Diabetic retinopathy treatment.
|
Clinical trials |
Results |
References |
|
Sustained delivery Bevacizumab vitreous implants: long-term benefit in patients with chronic diabetic macular edema [22]. |
In patients with chronic DME, implants releasing FAc 0.2 μg/day provides substantial visual benefit for up to 3 years and would provide an option for patients who do not respond to other therapy. |
Cunha-Vaz et al. |
|
Sustained ocular delivery of Bevacizumab by an intravitreal insert |
The FA intravitreal inserts provide excellent sustained intraocular release of FA for > or = 1 year. Although the number of patients in this trial was small, the data suggest that the inserts provide reduction of edema and improvement in BCVA in patients with DME with mild effects on intraocular pressure over the span of 1 year [23]. |
Campochiaro et al. |
|
Safety and efficacy of intraoperative intravitreal injection of triamcinolone acetonide injection after phacoemulsification in cases of uveitic cataract |
A single intraoperative intravitreal injection of triamcinolone acetonide seemed to be a safe and efficacious route of steroid delivery during phacoemulsification in patients with chronic idiopathic anterior uveitis or intermediate uveitis and is recommended as a substitute for postoperative oral steroid administration. |
Dada et al. |
|
State of the art clinical efficacy and safety evaluation of N-acetylcarnosine dipeptide ophthalmic prodrug. Principles for the delivery, self-bioactivation, molecular targets and interaction with a highly evolved histidyl-hydrazide structure in the treatment and therapeutic management of a group of sight-threatening eye diseases [24]. |
The results of this study provide a substantial basis for further evaluation of N-acetylcarnosine eye drops patented by IVP in the treatment and prevention of visual impairment in the temporal cross-sections of an older population several years apart [25]. In the number of promotion studies this ophthalmic drug showed experimental and clinical potential for the non-surgical treatment of age-related cataracts [26]. |
Babizhayev et al. |
|
N-acetylcarnosine lubricant eyedrops possess all-in-one universal antioxidant protective effects of L-carnosine in aqueous and lipid membrane environments, aldehyde scavenging, and transglycation activities inherent to cataracts: a clinical study of the new vision-saving drug N-acetylcarnosine eyedrop therapy in a database population of over 50,500 patients [27]. |
accumulated study data demonstrate that the IVP-designed new vision-saving drugs, including N-acetylcarnosine eyedrops, promote health vision and prevent vision disability from senile cataracts, primary open-angle glaucoma, age-related macular degeneration, diabetic retinopathy, and aging [28, 29]. N-acetylcarnosine eyedrop therapy is the crown jewel of the anti-aging medical movement and revolutionizes early detection, treatment, and rejuvenation of aging-related eye-disabling disorders. |
Babizhayev et al. |




References
- Sussman EJ, Tsiaras WG, Soper KA (1982) Diagnosis of diabetic eye disease. JAMA 247: 3231-3234. [Crossref]
- André Deshays C, Berthoz A, Revel M (1988) Eye-head coupling in humans. Exp Brain Res 69: 399-406. [Crossref]
- Early Treatment Diabetic Retinopathy Study Research Group (1991) Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology 98: 766-785. [Crossref]
- Diabetic Retinopathy Study Research Group (1981) Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. Ophthalmology 88: 583-600. [Crossref]
- Yun WL, Acharya UR, Venkatesh YV, Chee C, Min LC (2008) Identification of different stages of diabetic retinopathy using retinal optical images. Info Sci 178: 106-121.
- Tarr JM, Kaul K, Chopra M, Kohner EM, Chibber R (2013) Pathophysiology of diabetic retinopathy. ISRN Ophthalmol 2013: 343560. [Crossref]
- Funatsu H, Yamashita H (2002) Pathophysiology of diabetic retinopathy. Drug News Perspect 15: 633-639. [Crossref]
- Ciulla TA, Amador AG, Zinman B (2003) Diabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapies. Diabetes Care 26: 2653-2664. [Crossref]
- Ferris FL, Davis MD, Aiello LM (1999) Treatment of diabetic retinopathy. N Engl J Med 341: 667-678. [Crossref]
- Early Treatment Diabetic Retinopathy Study Research Group (1987) Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema: Early Treatment Diabetic Retinopathy Study report number 2. Ophthalmology 94: 761-774. [Crossref]
- Lee R, Wong TY, Sabanayagam C (2015) Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond) 2: 17. [Crossref]
- Fong DS, Aiello L, Gardner TW, King GL, Blankenship G et al. (2004) Retinopathy in diabetes. Diabetes Care 27: S84-S87. [Crossref]
- Keech AC, Mitchell P, Summanen PA, O'day J, Davis TM et al. (2007) Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 370: 1687-1697. [Crossref]
- Liang JC, Goldberg MF (1980) Treatment of diabetic retinopathy. Diabetes 29: 841-851. [Crossref]
- Early Treatment Diabetic Retinopathy Study Research Group (1987) Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. Int Ophthalmol Clinics 27: 254-264. [Crossref]
- Trautmann JC, Kearns TP (1969) Treatment of Diabetic Retinopathy. Postgraduate Med 45: 123-125.
- Nicholson BP, Schachat AP (2010) A review of clinical trials of anti-VEGF agents for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 248: 915-930. [Crossref]
- Mnyusiwalla A, Daar AS, Singer PA (2003) ‘Mind the gap’: science and ethics in nanotechnology. Nanotechnol 14: R9.
- Ritala M, Leskelä M (1999) Atomic layer epitaxy-a valuable tool for nanotechnology? Nanotechnol 19.
- Hughes MP (2000) AC electrokinetics: applications for nanotechnology. Nanotechnol 11: 124.
- Huang ZM, Zhang YZ, Kotaki M, Ramakrishna S (2003) A review on polymer In-situ implant by electrospinning and their applications in nanocomposites. Composites Sci Technol 63: 2223-2253.
- Ramakrishna S (2005) An introduction to electrospinning and In-situ implant. World Scientific.
- Fong H, Chun I, Reneker DH (1999) Beaded In-situ implant formed during electrospinning. Polymer 40: 4585-4592.
- Doshi J, Reneker DH (1995) Electrospinning process and applications of electrospun fibers. J Electrostatics 35: 151-160.
- Cunha Vaz J, Ashton P, Iezzi R, Campochiaro P, Dugel PU et al. (2014) Sustained delivery fluocinolone acetonide vitreous implants: long-term benefit in patients with chronic diabetic macular edema. Ophthalmol 121: 1892-1903. [Crossref]
- Campochiaro PA, Hafiz G, Shah SM, Bloom S, Brown DM et al. (2010) Sustained ocular delivery of Bevacizumab by an intravitreal insert. Ophthalmol 117: 1393.e3-1399.e3. [Crossref]
- Dada T, Dhawan M, Garg S, Nair S, Mandal S (2007) Safety and efficacy of intraoperative intravitreal injection of triamcinolone acetonide injection after phacoemulsification in cases of uveitic cataract. J Cataract Refractive Surg 33: 1613-1618. [Crossref]
- Babizhayev MA, Kasus Jacobi A (2009) State of the art clinical efficacy and safety evaluation of N-acetylcarnosine dipeptide ophthalmic prodrug. Principles for the delivery, self-bioactivation, molecular targets and interaction with a highly evolved histidyl-hydrazide structure in the treatment and therapeutic management of a group of sight-threatening eye diseases. Curr Clin Pharmacol 4: 4-37. [Crossref]
- Babizhayev MA, Micans P, Guiotto A Kasus Jacobi A (2009) N-acetylcarnosine lubricant eyedrops possess all-in-one universal antioxidant protective effects of L-carnosine in aqueous and lipid membrane environments, aldehyde scavenging, and transglycation activities inherent to cataracts: a clinical study of the new vision-saving drug N-acetylcarnosine eyedrop therapy in a database population of over 50,500 patients. Am J Ther 16: 517-533. [Crossref]

