Cystic Cervicitis and Infertility, A New Treatment Modality: A Case Report and Review of the Literature
A B S T R A C T
We present a rare case of cystic cervicitis in a 42-year-old woman who came to our unit suffering from primary infertility for one year. Her only complaint was infertility. She was not suffering from chronic pelvic pain or increased vaginal discharge neither before nor after marriage. Diagnosis of cystic cervicitis was made by both transvaginal ultrasound examination and MRI. As her main problem was infertility, she refrained from doing cone biopsy and opted for an ICSI trial and aspiration of the cervical cysts at the same time of ovum pick up (OPU). Ovum pick up resulted in the recovery of two oocytes. On the same setting and using the same needle, aspiration of all of the cervical cysts was performed successfully. Aspirated fluid was sent for cytology as well as culture and sensitivity. To our knowledge, this is the first case, in the english literature, to provide complete diagnosis of, and describe treatment of cystic cervicitis by transvaginal aspiration of the cysts.
Keywords
Cystic cervicitis, nabothian cysts, cervical cystic lesions, ICSI, infertility
Synopsis
ICSI and transvaginal aspiration of cervical cysts in a woman suffering from infertility and cystic cervicitis.
Introduction
Cystic lesions of the cervix, diagnosed by transvaginal ultrasound and/or MRI, are not common. Differential diagnosis includes benign conditions like nabothian cysts, cystic cervicitis, tunnel cluster and endocervical hyperplasia [1]. On the other hand, malignant cystic lesions of the cervix include adenocarcinoma and adenoma malignum (minimal deviation tumor of the cervix) [1]. MRI may help in the differentiation of such conditions [2]. Malignancy is suggested if the cystic lesion invades deep cervical stroma and contains a solid component [2]. On the other hand, benign conditions, usually, do not invade deeply into the cervical stroma, are usually small size, have well-defined margins and do not contain solid components [3]. The term cystic cervicitis was first given by Masson and Parsons back in 1982 [4]. Here, we describe a rare case of cystic cervicitis in an asymptomatic infertile patient and a new mode of management.
Case Presentation
I Facts and Assumptions
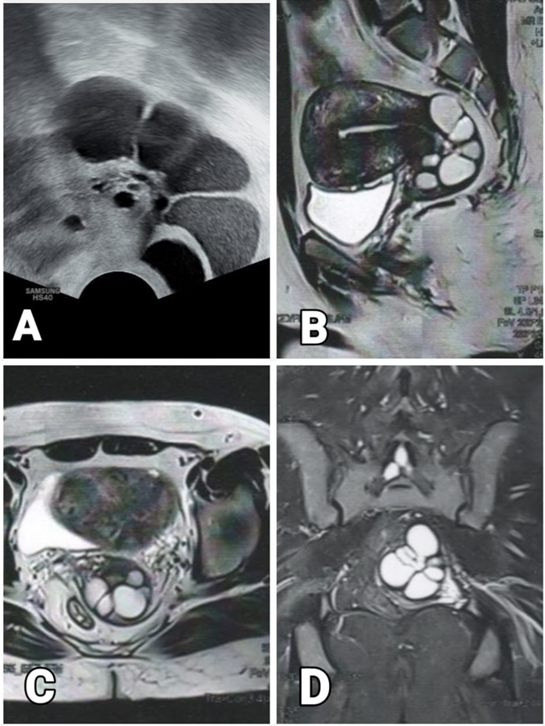
A 42-year-old woman presented to our unit with primary infertility of one year after her recent marriage. This is her first marriage. Her husband was previously married and has two living children. In addition to fertility issue, her cycles started to be irregular coming every 45-50 days in the last six months. She was quite anxious because of her age. Her abdominal examination was unremarkable. Cusco-speculum showed a normal healthy cervix. Pap smear was taken, and colposcopy was performed. Both came back to normal. On bimanual examination, there was ballooning of the posterior cervix. Transvaginal ultrasound examination showed a normal corpus and multiple large ~ 8 cervical retention cysts (12-25 mm in diameter) occupying the substance of the posterior cervix. Most of these cysts showed hyper-echogenic fluid inside (Figure 1A). Antral follicle count (AFC) was 2.
Figure 1: Cystic cervicitis. A) Trans-vaginal US: Sagittal view showing the cysts showing echogenic fluid content. B) MRI: Sagittal T2W showing the multilocular hyperintense cysts. C) MRI: Axial T2W showing the multilocular hyperintense cysts. D) MRI: Coronal STIR showing the multilocular hyperintense cysts.
Hormonal profile, semen analysis and MRI were requested. Patient FSH was 14.4 miu/ml, AMH = 0.01 ng/ml with normal LH, prolactin and TSH levels. Semen analysis came back normal. MRI showed multilocular cystic lesions in the posterior cervical wall extending/protruding into the vagina with no internal soft tissue components. Those cystic lesions exhibit hyperintense signal in T1, T2 and STIR suggesting either blood or chronically retained fluid. The final diagnosis of MRI was benign featuring cystic cervicitis (Figures 1B-1D).
Detailed counseling of the patient and her husband was given for both management of cystic cervicitis and the dismal prognosis of ICSI. Patient and her husband refrained from doing cone biopsy which will result in further delay in her fertility treatment in particular, in the presence of poor ovarian reserve (POSEIDON group = 4). The decision was to start controlled ovarian stimulation, egg collection and a trial of aspiration of these cysts at the time of OPU. An ethical approval was obtained and both partners gave their written informed consent for such management.
For her ICSI trial, short agonist protocol was chosen. She received highly purified FSH (Fostimon, IBSA, Institut Biochimique - Lugano - Switzerland) in a dose of 300 IU for 5 days followed by highly purified HMG, menotropin (Meriofert, IBSA, Institut Biochimique - Lugano - Switzerland) in a dose of 300 IU for seven more days. Two follicles grew up and triggering of ovulation was performed using 10000 IU HCG (Choriomon, IBSA, Lugano, Switzerland). OPU was performed 36 hours later using a wide bore (16G), double lumen OPU needle (Allwin, Allwin Medical devices, Anaheim, USA). Egg collection resulted in the recovery of two oocytes, one MI and the other was MII. Following OPU and with the use of the same needle, all cervical cysts were aspirated. The fluid within these cysts was very thick and we had to flush and aspirate the fluid using ringer`s lactate solution. All cysts were aspirated the same way as OPU and the aspirated fluid was sent for cytology and culture sensitivity (Figure 2).
Figure 2: A) Before the procedure. B) During the procedure: Aspiration needle inside one of the cysts. C) After the procedure.
The procedure took 15 minutes to complete and was uneventful. Three days later, she had an embryo transfer of one grade 2, six cell-stage embryo. Culture showed peptostreptococci (anaerobic Gram-positive cocci) for which she received an antibiotics course. On the other hand, cytology showed inflammatory cells (neutrophils, macrophages, plasma cells and lymphocytes) with no evidence of atypical or malignant cells. Both culture and cytology confirmed further the diagnosis of cystic cervicitis.
Discussion
This is a rare case of cystic cervicitis and infertility. Multilocular cystic lesions in the uterine cervix can vary widely from benign lesions to malignant lesions. The most common of them are nabothian cysts. Most of case reports of such lesions had treatment by either cone biopsy or hysterectomy. In our case, the patient was quite eager to preserve her uterus and to get pregnant. Depending on the benign featuring MRI characteristics in our patient (absence of solid components, well defined margins) a new treatment plan was suggested. The role of the radiologist is to ensure the identification of a broad spectrum of multilocular cystic lesions in the uterine cervix and possibly to differentiate malignant from benign lesions using either imaging or clinical features (or both). In our case, both clinical features and imaging were suggestive of the benign featuring cystic cervicitis. Okamoto and his colleagues tried to differentiate between benign and malignant lesions of the cervix by MRI [5]. They used three parameters: percentage of solid components in the lesion, the cyst diameter, and the signal intensity of the cyst fluid on a T1W1. Lesions were divided into 4 types (A-D) according to the percentages of solid and cystic components [5]. Type A: Entirely solid up to type D entirely cystic [5].
They reported an increased incidence of malignancy as the percentage of solid components increase. On the other hand, both cyst size and signal intensity of cyst fluid were not correlated with the malignancy potential [5]. However, it is not always possible to differentiate between malignant and benign cystic lesions of the cervix even with MRI. Combination of clinical presentation, imaging (US and MRI) and cervical biopsy may be needed in difficult cases. In our case, the absence of watery discharge (a chief clinical symptom observed in adenoma malignum), Type D (entirely cystic lesion with absence of solid components) on MRI, and well-defined margins were all reassuring of the benign nature of the condition and allowed us to adopt a more conservative approach. Differentiation between benign and malignant cystic lesions of the cervix is crucial and not always easy and may require cone biopsy or even hysterectomy.
According to our knowledge, this is first case (in the english literature) of cystic cervicitis to be treated by transvaginal aspiration of the cysts. Being familiar with the clinical setting and with the imaging features suggestive of multilocular cystic lesions in the uterine cervix, in particular MRI, can save patients unnecessary radical surgery before malignancy being diagnosed histopathologically. In addition, it can help in prompt and accurate diagnosis and possible conservative treatment as shown in our case.
Author Contributions
Tarek K. Al-Hussaini, he managed, counseled patient from A-Z. He diagnosed the case by transvaginal ultrasound and sent her for MRI. He did and monitored the ICSI trial and aspirated the cysts using the same needle of OPU. He did the embryo transfer. In, addition he wrote the manuscript. Moustafa T. Al-Hussaini, he was responsible for the MRI imaging of the patient. He helped in the diagnosis and reported upon the unusual presentation. He revised the manuscript before submission.
Conflicts of Interest
None.
Funding
None.
Data Availability
Data are available for this manuscript.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 12, Jun 2023Accepted: Tue 04, Jul 2023
Published: Tue 18, Jul 2023
Copyright
© 2023 Tarek Al-Hussaini. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CROGR.2023.01.01
Author Info
Tarek Al-Hussaini Moustafa T. Al-Hussaini
Corresponding Author
Tarek Al-HussainiDepartment of Obstetrics and Gynecology, Faculty of Medicine, Assiut University, Assiut, Egypt
Figures & Tables

References
1. Oliveto JM, Muinov
L (2016) Cystic Cervicitis: A Case Report and Literature Review of Cystic
Cervical Lesions. J Comput Assist Tomogr 40: 564-566. [Crossref]
2. Park SB, Lee JH,
Lee YH, Song MJ, Choi JH (2010) Multilocular cystic lesions in the uterine
cervix: broad spectrum of imaging features and pathologic correlation. AJR
Am J Roentgenol 2010:195: 517-523. [Crossref]
3. Doi T, Yamashita Y,
Yasunaga T, Fujiyoshi K, Tsunawaki A et al. (1997) Adenoma malignum: MR imaging
and pathologic study. Radiology 204: 39-42. [Crossref]
4. Masson JC, Parsons L (1928) Cystic cervicitis, with special reference to treatment by cauterization: A clinical study of 1031 cases. Am J Obstet Gynecol 16: 348-358.
5. Okamoto Y, Tanaka YO, Nishida M, Tsunoda H, Yoshikawa H (2004) Pelvic imaging: Multicystic uterine cervical lesions. Can magnetic resonance imaging differentiate benignancy from malignancy? Acta Radiol 45: 102-108. [Crossref]
