Current CT and MRI Applications in the Diagnosis of Bladder Cancer: A Review
A B S T R A C T
Most common urinary system cancer is the Bladder cancer(BC), more common in men (M/F: 3), is associated with both genetic and environmental factors.,two most well-known environmental factors are smoking and occupational exposures.Smoking is associated with 25-65% of BC cases, %50 average. Urothelial cancers are common in occupations that use paint, textiles, rubber and petroleum products. Among the chemical substances; O-toluidine, 2-naphthylamine, benzidine, 4-amino-biphenyl and nitrosamines are particularly related with the BC. Our objective in this systematic review is to indicate the value and aid of CT and MRI in the diagnosis of bladder cancer.
Keywords
Bladder, cancer, CT, MRI, diagnosis
Introduction
Most common urinary system cancer is the Bladder cancer (BC), more common in men (M/F:3), most common 7th cancer in men and 17th in women according to worldwide datas [1]. BC is associated with both genetic and environmental factors, two most well-known environmental factors are smoking and occupational exposures, etiology also differs according to the pathological subtypes of BC [1-3]. Smoking is associated with 25-65% of BC cases, %50 average. Risk of developing urothelial cancer is 2 to 4 times higher in smokers, current risk of developing cancer may regress to the level of non-smokers 12 to 15 years later after giving up smoking (risk continued up to 40 years) [2, 3].
Urothelial cancers are common in occupations that use paint, textiles, rubber and petroleum products. Among the chemical substances; O-toluidine, 2-naphthylamine, benzidine, 4-amino-biphenyl and nitrosamines are particularly related with the BC, it has also been reported that there is a relationship between some human papilloma virus (HPV) (especially type 16) and BCs [4]. Our objective in this systematic review is to indicate the value and aid of Computed tomography (CT) and Magnetic resonance imaging(MRI) in the diagnosis of BC.
Methods
I Data Sources
Most common type of BC is the transitional epithelial cell carcinoma and about 90% of BC develop in the epithelial cells lining the bladder [1-4]. Chronic irritation, schistosomiasis, bladder stones, and prolonged catheterization are associated with squamous cell BC. Other causes are phenacetin and cyclophosphamide use, pelvic radiation and tuberculosis [1, 2, 5]. Extrophy vesicale, urachal anomalies, neurogenic bladder, endometriosis or other adenocancer metastases can be counted in the etiology of bladder adenocancer [3, 5, 6]. Chief complaint is the haematuria, possibility of carcinoma in situ (CIS) should not be forgotten in the patients with lower urinary tract symptoms,mainly haematuria and also possibility of urothelial cancer in the upper urinary system increases in the presence of cancer in the trigone and high-risk cancers, none of the radiological imaging method is effective for the diagnosis of CIS [1, 5, 6]. Approximately 75% of BCs are diagnosed before muscle invasion so cystoscopy is an indispensable method in the diagnosis of papillary bladder cancers, tissue resection is required for definitive diagnosis and it is applied together with cytology and/or biopsies to prove the presence of CIS [5-7].
Photo-Dynamic Diagnosis (PDT) and Narrow-Band Imaging (NBI), which are macroscopic assistive imaging methods, are often used in daily practice as new cancer imaging methods. In vivo effective diagnosis is aimed with more experimental microscopic imaging methods such as confocal laser endomicroscopy (CLE), optical compatibility tomography (OCT), and ultraviolet microscopic fluorescent cystoscopy [1, 6]. The histological features of BC were first made by the World Health Organization (WHO) in 1973, corresponding to the to the degree of anaplasia of the cancer. According to this classification, urothelial cancers of the bladder are divided into 3 degrees [1, 2, 4, 5].
Grade 1: Well differentiated.
Grade 2: Moderately differentiated.
Grade 3: Poorly differentiated cancer.
The WHO classification of urothelial cancer in 2004 without muscle invasion is as follows:
1) Hyperplasia (Non-papillary flat lesion or flat lesion without atypia).
2) Reactive atypia (atypic flat lesion).
3) Unsignificant atypia.
4) Urothelial papilloma.
5) Urothelial carcinoma in situ.
6) urothelial dysplasia.
7) Papillary urothelial neoplasia with low malignant potentials (PUNLMP).
8) Urothelial papilloma inverted type.
9) high grade and low grade papillary urothelial cancer.
One of the most important goals in the staging of BC is to determine whether the cancer is muscle invasive or not, is urgent in the treatment decision and shows how vital the appropriate sampling and pathological examination are [1, 3, 5, 7].
i 2009 TNM Classification of BC [6, 7]
a T Primary Cancer
1) Tx Primary cancer not evaluated.
2) T0 No evidence for the presence of cancer.
3) Ta Non-invasive papillary carcinoma.
4) Tis Carcinoma in situ: Flat cancer.
5) T1 Cancer has invaded to the subepithelial connective tissue (Lamina propria).
6) T2 Cancer shows prominent invasion to the muscularis mucosa.
7) T2a Inner half of the muscle layer is invaded (Microscopical).
8) T2b Outer half of the muscle layer has been invaded (Macroscopical).
9) T3 Cancer has invaded the perivesical tissue.
10) T3a Microscopical extravesical spread.
11) T3b Macroscopic spread (perivesical mass) is present.
12) T4 Cancer shows spread to seminal vesicle, prostate, vagina, uterus, pelvic and abdominal wall.
13) T4a Cancer reveals invasion to the vagina, uterus or prostatic stroma.
14) T4b Cancer presents invasion to the pelvic and/or abdominal wall.
b N Lymph Node (LN)
1) Regional lymphs contain primary drainage areas. Remaining ones above the aorto-iliac bifurcation are assumed to be distant LN metastasis.
2) Nx LN could not be evaluated.
3) N0: Without any LN metastases.
4) N1: Positive single regional LN metastasis within true pelvis (obturator, external iliac, hypogastric, presacral).
5) N2 Presence of Multiple regional LN metastases within true pelvis (obturator, external iliac, hypogastric, presacral).
6) N3 Common iliac LN metastasis.
c M Distant Metastasis
1) M0 Distant metastasis negative.
2) M1 Distant metastasis positive.
One of the biggest problems in the staging of BCs is low staging, which is observed at a rate of 34-64%, when radical cystectomy specimens are analysed, 27% of patients with preoperative pT1 cancer have pT2 disease. Likewise, it has been reported that 49% of pT2 patients increased to T3 stage. Therefore, the American Urology Association and European Urology Association Guidelines recommend re-Transurethral Resection (TUR) for restaging in T1 disease [7, 8]. Approximately 15-30% of papillary and submucosal BCs become muscle-invasive cancers within five years. It has been known that the risk of stage progression is high in the high-risk patient group, such as presence of multifocal cancer, presence of pT1 cancer, high-grade cancer, cancer with CIS and cancer size greater than 3 cm however, appropriate and enough evidences are not still present in the international literature regarding the prognostic importance of vascular invasion, increased microvascular density, depth of submucosal invasion, high cancer markers and molecular genetic changes [3, 6-8]. It has been reported that performed re-TUR significantly reduces understaging. Residual disease, including muscle-invasive cancer, can also be demonstrated with re-TUR [7-9].
The staging of BCs is mostly based on pathological examination after TUR and radical cystectomy. CT is limited in the staging (between 40-60%), it has been reported that it cannot exactly distinguish inflammation from cancer after TUR and its value in LN involvement is 70-90% [2, 3, 5, 8]. MRI may be insufficient to detect microscopic extravesical spread, but its sensitivity in the staging of bladder cancers exists between 75-92% [10]. Average rate of accurate staging was 92%, and the rate of distinguishing patients with and without muscle invasion was found to be 85-95% by multiparametric use of T2 Weighted imaging(T2W)- Diffusion-weighted imaging (DWI) and Dynamic MRI [11-13]. According to these results, CT and MRI are more valuable, especially in identifying the patients over T2b stage [2, 5, 11].
The basic imaging methods for detecting bladder pathologies are intravenous urography, retrograde pyelography, cystography, voiding cystourethrography. With the introduction of cross-sectional imaging methods such as ultrasonography (US), CT and MRI, important developments and innovations are performed in the diagnosis of bladder pathologies. However, none of these modalities has overcome the need for conventional cystoscopy [1, 6, 8].
II Study Selection and Data Extraction
i CT Applications
Today, CT has a major role in investigating the etiology of haematuria, especially after invention of 64 and higher multi-slice. CTs and with their increased spatial resolution has increased the diagnostic success [1, 3, 4]. In addition, its high speed, ability to take very thin sections, reducing motion-related image distortions, and a significant reduction in the amount of administered contrast material, reduced the risk of nephrotoxicity [1-4]. CT is the most common utilized imaging facility in the depiction of BC and also serves fascinating diagnostic performance in the analysis of nodal and distant visceral metastases [1-4, 9].
Contrast material can be given by three methods in urinary CT scan; single-dose (single-bolus), two-dose (split bolus), and three-dose (triple-bolus). In the single-dose technique, all of the contrast material is applied at once and scanning is performed for arterial, venous, and pyelogram phases. In the two-dose technique, part of the contrast agent is given and the remaining part is administered until the pyelogram phase is obtained, is scanned after second dose while obtaining the nephrogram phase. Thus, the pyelogram and nephrogram phases are superimposed. In the three-dose technique, the scanning is started once the last of three divided doses is in the corticomedullary phase so corticomedullary-nephrographic and pyelographic phases are obtained simultaneously [1, 3, 9]. However, the negativity we encounter here is the significant decrease in the amount of contrast material that will reach the bladder during the pyelogram phase, this may cause missing of small lesions [3, 9]. Because of that, if bladder cancer is especially investigated, either a single dose technique should be used and/or oral-intravenous hydration together with diuretics should be used to increase the diagnostic success by increasing the amount of diluted contrast-containing urine passing into the bladder; Lesions with features of small filling defects may become visible [1, 3, 8, 9].
Diagnostic success of CT is very dependent on the technical parameters searching for bladder cancer, low accuracy rates are inevitable if single-phase imaging is performed before the patient is adequately hydrated and optimal bladder distension is not achieved. Acquisition of CT after TUR, carcinoma in situ, lesions smaller than 1 cm, flat and thin lesions, drugs administered into the bladder, systemic chemotherapy, inflammation, TUR or bladder biopsy before CT, are the causes of false negative CT [1-4]. Interventions through bladder before CT, staining and/or thickening of the mucosa or bladder wall; may reduce the specificity of CT by causing streaking and fibrosis in the perivesical adipose tissue [2-4, 9].
ii CT Virtual Cystoscopy
In the last decade, three-dimensional (3D) imaging techniques have been created by the development of CT devices, capable of rapid and volumetric scanning with accompanying developments in computer hardware and software technologies, endoscopy-like visualization of intraluminal pathologies such as bladder tumors is possible by these approaches [13].
Several studies have been reported, in which "volume scan" or "surface display" method is used, sufficient contrast should be created between the bladder wall or the mass and the lumen for virtual endoscopic visualization of bladder tumors, carbon dioxide and/or air can be given to the bladder lumen or positive contrast agents can be used in order to create and maintain this contrast [14, 15]. Sensitivity rates between 60% to 90% and 90-95% specificity have been presented in the diagnosis of bladder cancer by using this technique [14-16]. During CT virtual cystoscopy, Field of view (FOV) range can be kept wide and possible pelvic-paraaortic lymphadenopathies and upper urinary system pathologies can be detected, however, this technique has some handicaps such as catheterization is required if air-carbon dioxide is used as a contrast agent, has nephrotoxic effect if IV contrast agent is used, and its high radiation exposure [13-15]. CT and MR Urography are rarely needed in the diagnosis and staging of bladder tumors, CT Urography is the most important imaging approach for the diagnosis of renal pelvis tumors and urothelial cancers [3, 9].
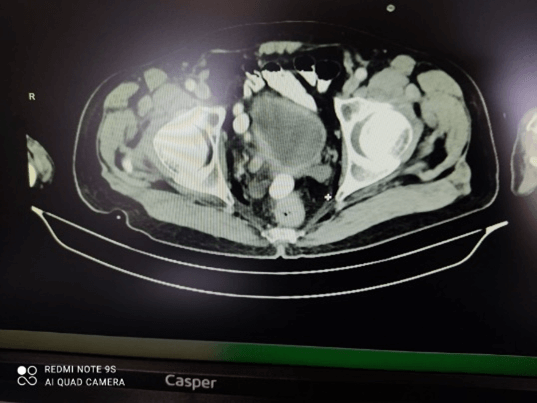
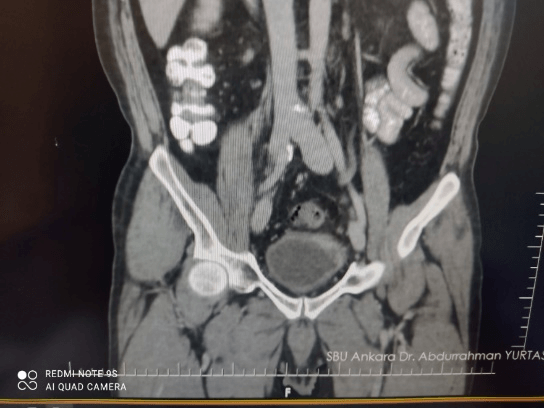
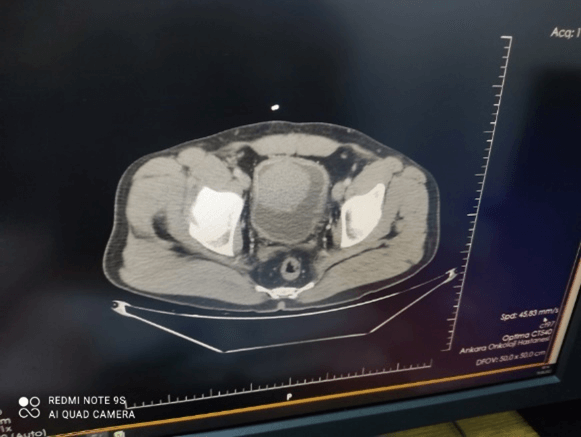
Overall, CT has many advantages for the initial diagnosis of BC due to its relative cost, high speed and accessibility, may strictly challenge with cystoscopy,urine studies and with even cytopathology (Figures 1 & 2). CT is probably the most common utilized imaging modality for the diagnosis and staging of BC, also supply beneficial diagnostic informations to the visualization of patients with suspicious concomitant upper urothelial tract carcinomas (Figure 3 & 4). Limitations of CT; Ionizing radiation exposure and limited availability in the accurate differentiation of local T-staging corresponding with the other imaging approaches [1-4, 9, 15, 17].
Figure 1: T2a tumor in the right lateral wall and in the base of bladder, visualized in contrast enhanced axial CT.
Figure 2: T3a tumor in the apex and upper left lateral bladder Wall, seen in contrast-enhanced coronal CT.
Figure 3: A nodular enhancing T2b tumor in the bladder lumen, shown in axial contrast ehanced CT.
Figure 4: A & B) A high contrast enhancing T4 tumor in the left basis and left lateral bladder wall, extending through left perivesical fatty area and left seminal vesicle with prominent diffusion restriction, seen in post-contrast T1W axial MR images and DWI.
iii MRI Applications
Correct T staging for BC before treatment is very important as it directly affects the therapeutic approaches. If the cancer is superficial and/or at T1 stage, TUR is sufficient, while radical cystectomy is required in T2 (muscle invasive tumor) and in higher stages [1 ,3, 7, 8]. The high soft tissue resolution of MRI and its ability to distinguish between bladder layers are the reasons for its superiority in local staging. The right treatment method can be selected by showing the depth of invasion of the tumor through the wall with MRI, accuracy of MRI in local staging is only possible with a high-quality acquisition [1, 5, 10, 11].
Optimal bladder distension has to be is achieved, slice thickness is 3 mm or less and must be taken continuously, high spatial and contrast resolution parameters has to be applied, MRI can be acquired at least 2 days after the withdrawal of a bladder balloon catheter to exclude the artefacts of intravesicular gas, particularly on DWI, on the other hand overfilled bladder can result to increasing patient discomfort during the MRI acquisition leading to the excessive motion artifacts,bowel motion and its artefacts can be eliminated by antispasmodic agent administration such as glucagon and/or buscopan [1, 10].
MRI acquisitions can be done on both 1.5T and 3T imaging systems for the diagnosis of BC however, 3T MRI has shown better acquisitions than 1.5T due to its higher temporal and spatial resolution, signal-to-noise and contrast-to-noise ratios; A phased array external surface multichannel coil and/or body coil is recommended to further optimization of whole sequences [1, 10, 18]. In the standard examination, three-dimensional fast spin echo T1W and T2W sequences are obtained with and/or without fat suppression. DWI is performed. Dynamic T1W sequences with pre and post-contrast acquisitions are also included in the multiparametric analysis (Figures 5A & B) [1, 10-13].
Figure 5: A & B) T4 tumor in the left half of bladder, extending to the perivesical fatty tissue at left side and beyond the apex,invading left seminal vesicle with prominent contrast-enhancement, visualized in substraction and dynamic axial MRI series.
Bladder wall consists of four layers: Urothelium (mucosa) that surrounds inner lumen of bladder; submucosa(vascular lamina propria); muscularis propria; and outer serosa, Three separate bladder wall layers: the inner layer of mucosa (urothelium), submucosal layer (lamina propria); muscularis propria (detrusor muscle); and perivesical fatty tissue can be seen on imaging modalities but those layers unfortunately cannot be well differentiated on all MRI sequences [1, 2, 11]. Urothelium and lamina propria(High vascularized inner layer) can not be reliably identified on T2W imaging and DWI, but can be captured in dynamic contrast enhanced imaging(DCE) as they enhance rapidly in the early arterial phase, approximately 20 sec. after IV contrast administration. In addition, muscularis propria enhances later than inner layers, show slow and progressive enhancement (approximately 60 s after contrast administration) [1, 11, 12, 18]. Muscularis propria is usually seen as an intermediate linear signal on DWI and with low-signal intensity line on T2W imaging [10-12, 18].
On T1W images, the extravesical extension is well evaluated, bone metastases and lymphadenopathies can also be distinguished.T2W images are suitable for investigating pathologies, the invasion of muscle layer can be reviewed in T2W sequences. Perivesical cancer extension, invasion of surrounding organs such as prostate and vagina can also be investigated (Figures 6A & 6B) [1, 11, 12]. If muscle invasion does not exist, hypointense line of muscle in the bladder wall does not deteriorate, focal thickening and staining on the wall and wall irregularity at the tumor base, can be seen in terms of muscle invasion [1, 10-12].
Figure 6: A & B) A heterogeneous T4 tumor mass,particularly hypointense in T2W images and highly enhancing substraction dynamic axial MRI series, tumor predominantly expands up to pelvic wall in the left lateral side and at apex.
T3A tumor cannot be easily detected in MRI and CT which is the microscopic perivesical invasion, tissue changes after TUR or a combination of chemoradiotherapy are also seen as exaggerated tumorextension with conventional CT and MRI, post-treatment residual cancer cannot be clearly differentiated from scar tissue by T2W examination [11, 12]. Angiogenesis leading to hypervascularity and early arterial contrast enhancement in tumors, those can be conducted by DCE imaging, mostly acquired in 2D or 3D T1W gradient echo sequences with fat-suppression performed before, during, and after IV administration of gadolinium-based contrast agent typically in 30 sec., 3D acquisitions are preferred for DCE imaging, due to its higher spatial resolution [1, 12, 13].
In contrast-enhanced dynamic MRI, rapid and distinct staining of local recurrences has been reported, postoperative inflammatory changes may retain contrast material for years and cause false positive results in the evaluation of tumor recurrence [12, 13, 19]. Suspicious lesions for BC have hypointense signal in T2W imaging with iso-hyperintense intensity change over muscle layer, reveal higher signal on DWI and low signal on ADC, indicating a diffusion restriction with early arterial post-contrast enhancement. A positive correlation between the grade of tumor and size of tumor is assumed to be present with regard to larger tumors as being high grade lesions, tumor location is also important for staging, since tumors located in bladder neck have a higher tendency for muscle invasion [1, 2, 5, 12, 13, 19].
In conclusion, single uses of both T2W sequence and contrast-enhanced dynamic MRI have limited role in the treatment and follow-up. When DWI is added and multiparametric examination is performed, much more successful results are obtained in both diagnosis, staging and follow-up processes [1, 10, 12, 13, 18-20]. One can realize that it may be possible to differentiate stage ≤T1 (non-muscle invading tumor) and ≥T2 (muscle invading tumor,either T2a or T2b stage tumors or high staging tumors extending through and/or beyond perivesical fat by acquisitions of all sequences, included in multiparametric-MRI [1, 5, 12, 19].
iv DWI
DWI is based on diffusion of protons in water molecules and is a functional imaging technique. It measures the random movement of the water molecule against the cell membrane barrier., A diffusion gradient is applied to the desired area with DWI and after a certain period of time, the signal is collected from the same area [1, 20, 21]. If the amount of cells per unit area is high (such as malignant tissue), water molecules cannot move quickly and remain in the same area where the gradient is sent thus, a high signal is obtained with diffusion restriction which is the restriction of the movement of water molecules [1, 20-23]. If the amount of cells per unit area is low, such as in benign tissues, water molecules will traverse, freely and randomly rotate without any restriction, causing decreased signal intensity [1, 20, 23]. ADC value is the 'Apparent diffusion coefficient' is roughly the path traveled by the water molecules.
Since the movement is limited in malignant tissues, the water molecules cannot go far away and the ADC value is lower than the normal tissues [1,10,18]. Bladder tumors also show restricted diffusion in DWI, has very important role in non-contrast evaluations, especially in patients with impaired renal function and having reluctancy to administer contrast agent due to side effects such as nephrogenic systemic fibrosis [12, 13, 20, 24]. Due to the non-solid structure of the bladder and its deteriorated morphology after chemo-radiotherapy, it is subjective and difficult to investigate the response to the treatment with anatomical imaging methods (such as basic MRI sequences and CT). Therefore, decreased amount of cells after the treatment will facilitate free movement of water molecules and lead to an increase in the ADC value. Thus, the response against treatment can also be monitored with DWI [13, 19, 24, 25]. Submucosal inflammation and fibrosis beneath the mass may result in overdiagnosis of non-invasive cancer as muscle-invasive on T2W images and/or dynamic contrast-enhanced MRI, this false staging can be prevented by distinguishing between invasion and inflammation or fibrosis with DWI [1, 11, 12, 19, 24, 25]. A similar mechanism is valid for the differentiation of perivesical spread from inflammation/fibrosis in stage T3 cancer; DWI prevents further advanced staging by providing discrimination in this topic as well [12, 24, 25].
Free-breathing spin-echo echo-planar imaging(EPI)-DWI could be performed in axial and coronal planes, these DWI planes and FOV should match with the ones used for T2W and DCE images, Nevertheless, ADC map should be generated with at least two b-values, including a high b-value >=800-1000 s/mm2 to establish sufficient contrast resolution; Increasing the number of excitations,parallel imaging, and using of potential simultaneous multislice techniques might be complementary strategies for accelerating the acquisition of DWI [1, 12, 19, 24]. If LN involvement is present in BC, the case is considered to be stage 4. The accuracy rate of LN involvement in CT is reported to be between 73-93%. In LN staging, sensitivity of DWI has been reported as 75-80% and specificity as 85-90% [2, 4, 5, 26].
Results
I Vesical Imaging-Reporting and Data System (VI-RADS)
VI-RADS 1: CE and DW, SC category 1, muscle invasion is highly unlikely.
VI-RADS 2: SC category 2-3 CE and/or DW category 2, muscle invasion is unlikely present.
VI-RADS 3: SC, CE and DW category 3, muscle invasion is equivocal.
VI-RADS 4: SC category 3-5 DW and/or CE category 4, muscle invasion is likely to be present.
VI-RADS 5: SC category 4-5 DW and/or CE category 5, invasion of muscle and beneath the bladder wall is very likely to be present.
DCE(CE-category), T2WI(SC-category) and DWI(DW-category), combined MRI findings, may predict the probability of clinically significant cancer that is, explained by the presence of any of the followings:
Each lesion is assumed to get 1 to 5 scores, regarding the possibility of clinically significant cancer [27-29].
II Assessment for T2WI with Structural Category (SC)
SC1-Category: Lesion <1 cm with continuous low signal line, presenting intact muscularis propria high signal thickened inner layer and/or exophytic tumor with stalk.
SC2-Category: Lesion >1 cm with continuous low signal line presenting intact muscularis propria, high signal thickened inner layer.and/or sessile/broad-based tumor or exophytic tumor with stalk.
SC3-Category: Sessile/broad-based tumor without thickened hyperintense inner layer, presence of an exophytic tumor without stalk and without any clear disruptions of hypointense muscularis propria, associated with negative category 2 findings.
SC4-Category: Intermediate signal tumor extending to muscularis propria via visualizing the interruption of low signal line.
SC5-Category: Invasion of entire bladder wall and extravesical tissues by extension of intermediate signal tumor to the extravesical fatty tissue [29, 30].
III Assessment for DCE with Contrast-Enhanced Category (CE)
CE1-Category: No early arterial enhancement of muscularis propria lesions with correspondence to SC1 findings.
CE2-Category: Presence of early arterial enhancement of inner layer lesions without early enhancement of muscularis propria corresponding to SC2 findings.
CE3-Category: Without any clear disruptions of hypointense lesions of muscularis propria regarded to SC3 findings, with lack of category 2 findings.
CE4-Category: Early tumoral enhancement which presents a focal extension to muscularis propria.
CE5-Category: Early arterial tumoral contrast enhancement which shows extension to the extravesical fatty tissue and entire bladder wall [27, 28, 30].
IV Assessment for DWI/ADC with DW Category (DW)
DW1-Category: Lesion <1 cm, intermediate continuous signal on DWI, muscularis propria shows diffusion restriction that is with high signal on DWI and hypointense on ADC and/or hypointense thickened inner layer on DWI with or without stalk.
DW2-Category: Lesion >1 cm, continuous intermediate signal on DWI, muscularis propria is shows diffusion restriction that is with high signal on DWI and hypointense on ADC, broad-based/sessile tumor with low/intermediate signal thickened inner layer on DWI or low signal thickened inner layer on DWI and/or with low signal stalk.
DW3-Category: Without any clear disruptions of low signal muscularis propria and without presence of category 2 results with correspondence to T2 category 3 results.
DW4-Category: Tumor shows diffusion restriction that is hyperintense on DWI and hypointense on ADC which presents focal extension to muscularis propria.
DW5-Category: Tumor, hyperintense on DWI and hypointense on ADC maps, shows precise extension to the extravesical fatty tissue and entire bladder wall [27-31].
Discussion
Clinical Applications of CT and MRI in Routine Practice
There were several researches in the literature concerning to the diagnosis,staging and treatment options of BC with CT and MRI. Mirmomen and his colleagues.regarded 91% diagnostic accuracy in the depiction of urothelial malignant tumors by CT, also presented 49-93% accuracy in the tumors of > stage T3 with perivesicular invasion [2]. CT shows superiority over cystoscopy for diagnostic accuracy in bladder diverticulum tumors, very rare (~1.5% of all bladder tumors), especially when a diverticula has narrow necks causing difficulties in accessing the tumor with limited visualization and tissue sampling via the cystoscopic approach [17].
Trinh and his colleagues analysed the causes of false-negative and false-positive observations on CT with regard to well-known cystoscopy, false-positive findings were probably due to posttreatment changes, benign prostatic hypertrophy, bladder trabeculation and intravesical blood clots.False-negative findings were mainly caused by flat urothelial lesions due to inadequate bladder lumen filling during the excretory phase of CT which had stated that negative predictive values and sensitivity were considered to be highest in the corticomedullary phase (99% and 95%) respectively [3]. Metastatic disease is generally well recognized by CT, Rajesh et al. reported that 6% of all-BCs presented distant metastases, most commonly to the retroperitoneal lymph nodes, peritoneal metastases ranged between 7.6 to 16% of cases were also described, which were particulary observed in atypical variant histologic cases of BC with increasing frequency [4, 32].
In the near future, new eras for CT is composed of radiomic processing protocols, machine learning and neural networks. Newer reports have clarified that decision of computerized -supporting systems may improve accuracy of radiologists, also decline interobserver variability to identify the response against treatment that involves entire reaction to neoadjuvant chemotherapy, applied against muscle-invasive BCs [1, 13, 32]. Studies investigating the validity of VI-RADS assessed approximately 76 and 95%, sensitivity, 44 and 93% specificity in the discrimination of Muscle-invasive BC from Non-Muscle Invasive BC [27, 30, 31].
Kobayashi et al. indicated significant differences between Ta and T1 disease and between T1 and T2 disease,correlated with ADC values[10]. Huang et al. analysed 17 researches, 1449 BC patients in their meta-analysis and declared that pooled sensitivity and specificity of MRI were % 90 and % 88 respectively, for differentiating tumors <=stage T1 from those >=stage T2, DWI and use of 3.T MRI improved sensitivity to 95% and specificity to 95%.,they demonstrated high diagnostic performance of MRI in the discrimination of T1 or lower tumors from T2 or higher tumors in patients with BC in their meta analyis [11]. Al Johi et al. studied 102 patients with BC, they added DWI and ADC values to T2W images to improve accuracy of MRI in the diagnosis of BC, however they reported that MRI cannot replace TUR and biopsy yields [20].
Yuan et al. conducted a retrospective study with 163 BC patients and presented that T2W imaging and DCE imaging plus DWI provided useful information for T staging,grading in BC and distinguishing Ta stage from T1 stage [12]. Artificial Intelligence(AI) was also added to CT and MRI researches in last few years, corresponding with the diagnosis-staging and treatment response evaluations of BC -Kozikowski et al. analysed 8 studies with 860 BC patients in their meta-analysis, predicted 82-81% sensitivity and specificity for the diagnosis of muscle invasive BC with Radiomics [33]. Cha et al. acquired radiomics-based predictive models by inserting pre- and post-treatment images, acquired by CT, searched whether they could discriminate between BCs with and without complete chemotherapy responses and indicated that Radiomics taken from CT of BC patients distinctly aid to assist in the assessment of treatment response [34].
Hammouda et al. developed a multiparametric computer-aided diagnostic system for BC staging, especially to differentiate between T1 and T2 stages, by using T2W imaging and DWI in their study, they established the framework with bladder wall segmentation, whole BC volume localization and its extention through the wall, radiomic features were estimated from T2W acquisitions and morphological features in order to describe geometry of tumors, presented 95.24%, 95.24%, 95.24% accuracy,sensitivity and specificity [35]. Xu et al. studied 1104 radiomics texture with T2W imaging and DWI retrospectively to discriminate between non-muscle-invasive bladder carcinomas from the muscle-invasive ones preoperatively under 3.T MRI and regarded 92.6%, 100%, 96.3%, average sensitivity, specificity and accuracy for the differentiation of muscle invasion in BC, preoperatively [36].
Xu S et al. investigated the value of radiomics results, derived from DWI in the differentiation of muscle-invasive BC from non-muscle-invasive BC.Radiomics models based on DWI, were established by using random forest (RF) and all-relevant (AR) methods. RF model was more sensitive than TUR(0.873) in the discrimination of muscle-invasive BC. RF in addition to TUR lead to an increased sensitivity up to 0.964 and finally reported that Combined radiomics features of DWI plus TUR could easily strengthen the accuracy, sensitivity for the differentiation of muscle invasive BC in routine practices [37]. To our experience, urologists and medical oncologists would feel themselves so safe in the diagnosis, treatment and follow-up of BC patients with regard to all those researches, Current CT and MRI yields also supply so valuable informations in the staging of BC, leading to a more trustable TUR and/or radical cystectomies [1, 5, 12, 13, 38, 39].
Conclusion
Corresponding to different modalities, BC imaging supplies very important informations in the diagnosis and staging of bladder tumors. CT is the most frequently utilized and widely available imaging approach in the detection of BC, also serves extremely high performance in capturing of visceral and nodal metastatic extentions. MRI preserves superior potentials for the evaluation of muscular invasion and locoregional staging of BC, which has a critical role in determining prognosis and deciding the most appropriate treatment.
Key Points
1) CT and MRI in the diagnosis of BC.
2) CT and MRI in the staging of BC.
3) CT and MRI in the discrimination of muscle-invasive from Nonmuscle invasive BC.
4) VIRADS score in the diagnosis of BC.
Funding
None.
Competing Interests
None.
Conflicts of Interest
None.
Ethical Approval
Not applicable.
Consent to Participate
Applicable.
Data and Material Availability
Suitable data transparency.
Author Contributions
Study concept and design: YÖ. Acquisition of data: EYB. Analysis and interpretation of data: HA,YÖ. Drafting of the manuscript: YÖ, MBA. Critical revision of the manuscript for important intellectual content: HA. Statistical analysis: EYB,MBA. Administrative, technical, and material support: YÖ.MBA. Study supervision: HA,EYB.
Acknowledgement
None.
Abbreviations
BC: Bladder Cancer
CT: Computed Tomography
MRI: Magnetic Resonance Imaging
CIS: Carcinoma in situ
PDT: Photo-Dynamic Diagnosis
NBI: Narrow-Band Imaging
CLE: Confocal Laser Endomicroscopy
OCT: Optical Compatibility Tomography
WHO: World Health Organization
PUNLMP: Papillary Urothelial Neoplasia with Low Malignant Potentials
LN: Lymph Node
TUR: Transurethral Resection
T2W: T2 Weighted imaging
DWI: Diffusion-Weighted Imaging
US: Ultrasonography
3D: Three-Dimensional
FOV: Field of View
DCE: Dynamic Contrast Enhanced imaging
ADC: Apparent Diffusion Coefficient
EPI: Echo-Planar İmaging
VI-RADS: Vesical Imaging-Reporting and Data System
DCE: CE-Category
T2WI: SC-category
DWI: DW-category
SC: Structural Category
CE: Contrast-Enhanced category
DW: DW category
AI: Artificial Intelligence
RF: Random Forest
AR: All-Relevant
Article Info
Article Type
Review ArticlePublication history
Received: Thu 22, Dec 2022Accepted: Mon 30, Jan 2023
Published: Wed 03, May 2023
Copyright
© 2023 Hasan Aydin. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2023.01.01
Author Info
Hasan Aydin Ezel Yaltirik Bilgin Yasin Ozdemir Muazzez Bengi Akyol
Corresponding Author
Hasan AydinRadiology Department, Ankara Oncology Education and Research Hospital, Ankara, Turkey
Figures & Tables



References
1. Galgano SJ, Porter
KK, Burgan C, Rais Bahrami S (2020) The Role of Imaging in Bladder Cancer
Diagnosis and Staging. Diagnostics (Basel) 10: 703. [Crossref]
2. Mirmomen SM,
Shinagare AB, Williams KE, Silverman SG, Malayeri AA (2019) Preoperative
imaging for locoregional staging of bladder cancer. Abdom Radiol (NY)
44: 3843-3857. [Crossref]
3. Trinh TW, Glazer
DI, Sadow CA, Sahni VA, Geller NL et al. (2018) Bladder cancer diagnosis with
CT urography: Test characteristics and reasons for false-positive and
false-negative results. Abdom Radiol (NY) 43: 663-671 [Crossref]
4. Rajesh A, Sokhi H,
Fung R, Mulcahy KA, Bankart MJ (2011) Role of whole-body staging computed
tomographic scans for detecting distant metastases in patients with bladder
cancer. J. Comput Assist Tomogr 35: 402-405. [Crossref]
5. Lee CH, Tan CH, de
Castro Faria S, Kundra V (2017) Role of Imaging in the Local Staging of
Urothelial Carcinoma of the Bladder. AJR Am J Roentgenol 208: 1193-1205.
[Crossref]
6. Pichler R, De Zordo
T, Fritz J, Kroiss A, Aigner F et al. (2017) Pelvic Lymph Node Staging by
Combined 18F-FDG-PET/CT Imaging in Bladder Cancer Prior to Radical
Cystectomy. Clin Genitourin Cancer 15: e387-e395. [Crossref]
7. Allen BC, Oto A,
Akin O, Alexander LF, Chong J et al. (2019) ACR Appropriateness Criteria®
Post-Treatment Surveillance of Bladder Cancer. J Am Coll Radiol 16:
S417-S427 [Crossref]
8. Babjuk M, Burger M,
Capoun O, Cohen D, Compérat EM et al. (2022) European Association of Urology
Guidelines on Non-muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in
Situ). Eur Urol 81:75-94. [Crossref]
9. Helenius M, Dahlman
P, Lönnemark M, Brekkan E, Wernroth L et al. (2016) Comparison of post contrast
CT urography phases in bladder cancer detection. Eur Radiol 26: 585-591
[Crossref]
10. Kobayashi S,
Takemura K, Koga F (2022) Apparent Diffusion Coefficient Value as a Biomarker
for Detecting Muscle-Invasive and High-Grade Bladder Cancer: A Systematic
Review. Appl Sci 12: 1278.
11. Huang L, Kong Q,
Liu Z, Wang J, Kang Z et al. (2018) The Diagnostic Value of MR Imaging in
Differentiating T Staging of Bladder Cancer: A Meta-Analysis. Radiology
286: 502-511 [Crossref]
12. Yuan L, Li D, Mu D,
Zhang X, Kong W et al. (2020) Combined T2 SPAIR, Dynamic Enhancement and DW
Imaging Reliably Detect T Staging and Grading of Bladder Cancer With 3.0T MRI. Front
Oncol 10: 582532. [Crossref]
13. Ahmed SA, Taher
MGA, Ali WA, Ebrahem MAES (2021) Diagnostic performance of contrast-enhanced
dynamic and diffusion-weighted MR imaging in the assessment of tumor response
to neoadjuvant therapy in muscle-invasive bladder cancer. Abdom Radiol (NY)
46:2712-2721. [Crossref]
14. Bernhardt TM, Rapp
Bernhardt U (2001) Virtual cystoscopy of the bladder based on CT and MRI data. Abdom
Imaging 26: 325-332 [Crossref]
15. Abrol S, Jairath A,
Ganpule S, Ganpule A, Mishra S et al. (2015) Can CT Virtual Cystoscopy Replace
Conventional Cystoscopy in Early Detection of Bladder Cancer? Adv Urol
2015: 926590. [Crossref]
16. Gabr AH, Elbadry M,
Elsherief A, Tawfiek ER (2013) Computed tomography-virtual cystoscopy in the
evaluation of a bladder mass: Could it replace standard conventional
cystoscopy? Arab J Urol 11: 369-374. [Crossref]
17. Walker NF, Gan C,
Olsburgh J, Khan MS (2014) Diagnosis and management of intradiverticular
bladder tumours. Nat Rev Urol 11: 383-390. [Crossref]
18. Fujimura M,
Sakamoto S, Sekita N, Takeuchi N, Nishikawa R et al. (2016) Apparent diffusion
coefficient value for estimating clinicohistological factors in bladder cancer
including infiltration style and lymphatic invasion. Springerplus 5:
848. [Crossref]
19. Wang X, Tu N, Sun
F, Wen Z, Lan X et al. (2021) Detecting Muscle Invasion of Bladder Cancer Using
a Proposed Magnetic Resonance Imaging Strategy. J Magn Reson Imaging 54:
1212-1221. [Crossref]
20. Al Johi RS,
Seifeldein GS, Moeen AM, Aboulhagag NA, Moussa EM et al. (2018) Diffusion
weighted magnetic resonance imaging in bladder cancer, is it time to replace
biopsy? Cent European J Urol 71: 31-37. [Crossref]
21. Aydin H, Kizilgoz
V, Hekimoglu B (2011) Is the quantitative Diffusion-Weighted MR Imaging and ADC
mapping with b-values of 50, 400, and 800 sec/mm(2) a reliable method for
evaluation of meniscal tears in the knee? Pol J Radiol 76: 30-40. [Crossref]
22. Metin MR, Aydın H,
Çetin H, Özmen E, Kayaçetin S (2016) The efficacy of diffusion weighted imaging
and apparent diffusion coefficients mapping for liver metastasis of colonic
adenocarcinomas. Saudi Med J 37 (4): 379-385. [Crossref]
23. Aydin H, Tatar IG,
Hekimoglu B (2014) The Role of Diffusion Weighted MR Imaging in the Diagnosis
of Acute Pancreatitis. Int J Emerg Ment Health 16: 93-98. [Crossref]
24. Razik A, Das CJ,
Sharma S, Seth A, Srivastava DN et al. (2018) Diagnostic performance of
diffusion-weighted MR imaging at 3.0 T in predicting muscle invasion in urinary
bladder cancer: utility of evaluating the morphology of the reactive tumor
stalk. Abdom Radiol (NY) 43: 2431-2441. [Crossref]
25. Meng X, Hu H, Wang
Y, Hu D, Li Z et al. (2021) Application of bi-planar reduced field-of-view DWI
(rFOV DWI) in the assessment of muscle-invasiveness of bladder cancer. Eur J
Radiol 136:109486. [Crossref]
26. Thoeny HC,
Froehlich JM, Triantafyllou M, Huesler J, ;Bains LJ et al. (2014) Metastases in
Normal-sized Pelvic Lymph Nodes: Detection with Diffusion-weighted MR. Imaging.
Radiology 273: 125-135. [Crossref]
27. Woo S, Panebianco
V, Narumi Y, Del Giudice F, Muglia VF et al. (2020) Diagnostic Performance of
Vesical Imaging Reporting and Data System for the Prediction of Muscle-invasive
Bladder Cancer: A Systematic Review and Meta-analysis. Eur. Urol. Oncol
3: 306-315. [Crossref]
28. Pecoraro M,
Takeuchi M, Vargas HA, Muglia VF, Cipollari, S et al. (2020) Overview of
VI-RADS in Bladder Cancer. AJR Am J Roentgenol 214:1259-1268. [Crossref]
29. Panebianco V,
Narumi Y, Altun E, Bochner BH, Efstathiou JA et al. (2018) Multiparametric
Magnetic Resonance Imaging for Bladder Cancer: Development of VI-RADS (Vesical
Imaging-Reporting And Data System). Eur Urol 74: 294-306. [Crossref]
30. Kim SH (2020)
Validation of vesical imaging reporting and data system for assessing muscle
invasion in bladder tumor. Abdom. Radiol (NY) 45: 491-498. [Crossref]
31. Sakamoto K, Ito M,
Ikuta S, Nakanishi Y, Kataoka M et al. (2020) Detection of Muscle-Invasive
Bladder Cancer on Biparametric MRI Using Vesical Imaging-Reporting and Data
System and Apparent Diffusion Coefficient Values (VI-RADS/ADC). Bladder
Cancer 6:161-169.
32. Turkbey B, Basaran
C, Karcaaltincaba M, Akpinar E, Oguz B et al. (2008) Peritoneal carcinomatosis
in urinary bladder cancer. Clin. Imaging 32: 192-195 [Crossref]
33. Kozikowski M,
Suarez Ibarrola R, Osiecki R, Bilski K, Gratzke C, et al. (2022) Role of
Radiomics in the Prediction of Muscle-invasive Bladder Cancer: A Systematic
Review and Meta-analysis. Eur Urol Focus 8: 728-738. [Crossref]
34. Cha KH, Hadjiiski
L, Chan HP, Weizer AZ, Alva A et al. (2017) Bladder Cancer Treatment Response
Assessment in CT using Radiomics with Deep-Learning. Sci Rep 7: 8738. [Crossref]
35. Hammouda K, Khalifa
F, Soliman A, Ghazal M, El-Ghar MA et al. (2021) A multiparametric MRI-based
CAD system for accurate diagnosis of bladder cancer staging. Comput Med
Imaging Graph. 90: 101911. [Crossref]
36. Xu X, Zhang X, Tian
Q, Wang H, Cui LB et al. (2019) Quantitative Identification of
Nonmuscle-Invasive and Muscle-Invasive Bladder Carcinomas: A Multiparametric
MRI Radiomics Analysis. J Magn Reson Imaging 49: 1489-1498 [Crossref]
37. Xu S, Yao Q, Liu G,
Jin D, Chen H et al. (2020) Combining DWI radiomics features with transurethral
resection promotes the differentiation between muscle-invasive bladder cancer
and non-muscle-invasive bladder cancer. Eur Radiol 30:1804-1812 [Crossref]
38. Zhang G, Wu Z, Xu L, Zhang X, Zhang D et al. (2021) Deep Learning on Enhanced CT Images Can Predict the Muscular Invasiveness of Bladder Cancer. Front Oncol 11 :654685. [Crossref]
39. Zhang X, Xu X, Tian Q, Li B, Wu Y et al. (2017) Radiomics assessment of bladder cancer grade using texture features from diffusion-weighted imaging. J Magn Reson Imaging 46: 1281-1288. [Crossref]
