Journals
Coupling Failure as the Forth Category in the Classification of Congenital Spinal Deformity
A B S T R A C T
Study Design: A retrospective study
Objective: To analyze the discordant relationship between anterior and posterior structure in congenital spinal deformity (CSD).
Summary of Background Data: Winter classified CSD into three categories, formation failureW,1, segmentation failureW, and mixed type. While it has been widely used for analysis of CSD for more than 30 years, there are some types of CSD with atypical vertebral anomalies (VAs), which do not belong to any of the three categories.
Methods: Three-dimensionally reconstructed CT images of 332 patients with CSD were evaluated to clarify the relationship between the anterior and posterior structure of each VA according to the algorism for evaluation of CSD presented by Kawakami. Those that belonged to the multiple complex types (MC) were analyzed to determine the presence of discordancy.
Results: Of 332, 104 patients were classified as Solitary simple (SS), 69 as Multiple simple (MS), 35 as SF, and 124 as MC. 38 of the 124 patients with MC were subclassified into the Mismatch malformation type (MMC). Twelve of the 38 patients with the MMC exhibited three types of unusual VAs; 2 patients with a combination of a normal vertebral body (VB) with hemilaminae (Posterior mismatch type); 2 with normal laminae with contralateral hemivertebral bodies (Anterior mismatch type); and 8 with a discordant combination of multiple contralateral hemivertebral bodies and hemilaminae (Anteroposterior mismatch type). This study proposed to put these three types with mismatch phenomena together and was termed “Coupling failure”, which was regarded as a fourth category of CSD.
Conclusion: Coupling failure is completely different from both formation failureW and segmentation failureW in terms of the developmental mechanisms and characteristics of discordancy. The addition of coupling failure facilitates the understanding of complicated CSD, which can then be classified clearly into four categories, including formation failureK, coupling failure, segmentation failureK, and Mixed failure.
K E Y W O R D S
congenital spinal deformity, classification, formation failure, segmentation failure, coupling failure, mixed failure
I N T R O D U C T I O N
Congenital vertebral anomaly (CVA) is recognized as one of the major etiologies of spinal deformity. Some patients may have only one congenital abnormal vertebra and in such a case, spinal deformity (SD) may be strongly dependent solely on its morphological characteristics. Others may have assortment of multiple vertebral anomalies that may exist separately or consecutively; it may be too difficult to evaluate exactly which abnormal vertebrae are responsible for the SD. Congenital spinal deformity (CSD) includes scoliosis, kyphosis, lordosis, or their combination and the type and severity of CSD mainly depend on location, numbers, and types of CVAs.
Winter classified congenital scoliosis into three categories such as formation failure W 1, segmentation failure W, and mixed type W [1, 2]. On the other hand, McMaster and Singh presented congenital kyphosis into anterior failure of vertebral body formation, anterior failure of vertebral body segmentation, and mixture of formation and segmentation failure [3]. These two classifications have been widely accepted and recognized as the golden standard in describing each type of vertebral anomalies in CSD. In essence, both classifications have contributed to the planning of surgical strategies, clarifying natural history of CSD, and researching surgical outcomes reported in literature. Although their concepts are well organized to allow the comprehension of more complicated CSDs in much simpler terms, we still encounter patients with complicated vertebral anomalies that are too difficult to classify with the present classifications. Furthermore, progression of some types of CSD deviate from what is expected by the natural history presented by McMaster. Along similar lines, Winter reported that some patients with hemivertebrae, had shown a pattern of natural regression in their scoliosis, and described that it was not always easy to expect how much progression of CS due to hemivertebrae will occur during the growth period [4].
Regarding surgical treatment with vertebrectomy, wrong level surgery is one of the most worrisome of potential complications. In particular, recent shift to posterior only approach for vertebrectomy in congenital scoliosis requires the surgeon to locate the vertebral anomalies from viewing the posterior structure only. Most well-experienced spine surgeons surely have some experiences of disorientation when detecting anatomical landmarks of target congenital anomalous vertebrae at the time of posterior exposure for vertebrectomy. Such unpleasant experiences definitely come from the fact that both classifications were conducted based on analysis using two-dimensional images of CVAs. Winter’s classification does not provide us with any information related to posterior structure of CVAs. Furthermore, it does not put any anomalous change of posterior structure in CVA into the basic concept of their classifications.
On the other hand, Nakajima, et al. investigated three-dimensional morphology of vertebral anomalies due to formation failureW [5]. They found various types of posterior structure and presented discordant relationship between anterior and posterior structure in CVAs for the first time. Furthermore, Kawakami, et al. presented new classification with four categories based on analysis of three-dimensional morphology of CSD in terms of the relationship between anterior and posterior structure; they were type I: solitary simple (SS), type II: multiple simple (MS), type III: mixed complex type (MC), type IV: segmentation failureK (SFK) [6]. However, this classification is overly complicated and difficult to use in clinical practice.
One example of previously untapped information derived from three-dimensional analysis of CSD presented by Nakajima and Kawakami were the detection of previously unclassified vertebral anomalies in CVAs; thus far, anomalies that they have presented have not been recognized by analyzing plain X-ray images only. This approach has some possibilities to clarify the complex anomalies of CSD more clearly and to solve some clinical problems, such as inferring natural course and avoid possible disorientation during posterior vertebrectomy. The purpose of this study was to present previously unclassified types of CVAs followed by the introduction of a new category for CSD classification, and to simplify the previous overly complicated classification of CSD into a simpler but more accurate and versatile form.
Material and Methods
This study was conducted under IRB approval in Meijo Hospital. Since 2001 to 2013, 566 patients with CVA visited Meijo hospital complaining back deformity. Spinal deformity in 566 patients varied from “no” or “slight” to “very severe.” Of them, 332 patients with CSDs were evaluated using 3D-CT images to investigate whether they should be surgically treated or not, and if applicable, to determine surgical strategy for vertebrectomy. The mean age of the 332 patients at the time of CT acquisition was 8.9 years (2-50). Distribution of sex was male in 144 and female in 187. We did not perform CT check-up for children younger than 2 years partly as our principle of CSD for surgical treatment was over 2 years and also due to a large proportion of cartilaginous tissue in the vertebrae of very young pediatric patients that may potentially interfere with the evaluation of vertebral anomalies. Open spine lesions including spina bifida except those that occur only in the sacrum were excluded in this study.
According to 3D-Classification presented by Kawakami, et al, 332 were classified into four types such as SS, MS, MC, and SFK. Anterior, posterior structure, and the relationship between them in each patient were evaluated according to the algorism of evaluating CSD by two veteran spine surgeons (NK, TS) who were familiar with 3D-CT images of CSD.
3D-CT images were mainly taken using the TOSHIBA AquilionTM 64, with a slice thickness of 2 mm. Three-dimensional images were expressed by volume rendering. The imaging slices were generally extended over the entire spinal column exhibiting SD.
Results
Of 332 patients, 104 were classified into SS, 69 into MS, 35 into SFK, and 124 into MC (Figure 1). 124 patients with MC were subdivided into 38 patients of mismatch complex type (MMC) and 86 patients of complex malformation type (CM); the latter was the type with an overly complicated set of vertebral abnormalities.
Evaluation of discordancy in 38 patients with the MMC type clarified that 12 of 38 patients exhibited very unusual vertebral anomalies in addition to the mismatch phenomena (Table). There were three types with respect to the relationship among normal and abnormal structure of vertebrae. The first type was one of vertebral anomalies with a combination of normal vertebral bodies and multiple contralateral hemilaminae (Figure 2). Two patients belonged to this type in this study. The second was one of those combining multiple contralateral hemivertebral bodies with normal laminae (Figure 3). Two patients of this study were seen with this type. The third was one with a discordant combination with multiple contralateral hemivertebral bodies and multiple contralateral hemilaminae (Figure 4). Eight patients in this study were of this type. The common features of these types were:
- some specific type of discordant anomaly with a discordant combination of normal vertebral bodies and/or laminae,
- relative difficulty in differentiating normal vertebrae from the abnormal.
Although 22 patients out of the 26 in the MMC type had vertebral anomalies that were classified into the third type, in reality, segmentation failure and/or other complex vertebral malformation have combined together with mismatched anomalies in these patients (Figure 5). Four patients of 26 had only one hemivertebra with discordancy of the lamina (Figure 6).
Figures & Tables
Figure 1: Types of Vertebral anomalies in 332 patients.
Figure 2: The Anterior type of Coupling failure
While laminae demonstrated almost normal shape with a little bit asymmetry except of sacral spina bifida, two contralateral hemivertebrae exist.
Figure 3: The Posterior type of Coupling failure
Lt. hemilamina of T5 and Rt. Hemilamina of T6 exists although vertebral bodes of T5, T6, T7, T8 looks normal with disc space narrowing on T5/6, T7/8.
Figure 4: The Anterosterior type of Coupling failure
Anterior structure: a butterfly vertebra on C5, semisegmented hemivertebral body on lt. C7 (arrow), and semisegmented hemivertebral body on rt. T7 (arrow).
Posterior structure; a semisegmented hemilamina on the lt. C5 with a normal lamina on T1 (arrow), and a fully-segmented hemilamina on the rt. T8 (arrow).
Figure 5: The Mixed failure: multiple vertebral anomalies with formation, coupling, and segmentation failure.
Anterior structure: a semisegmented hemivertebral body on the rt. T5 (arrow) and semisegmented vertebral body on the lt. T8 (arrow). With T6 & T7 fused congenitally.
Figure 6: The Mixed failure: A hemivertebral body with a discordant hemilamina
A semisegmented hemivertebral body exists on L4 with normal lamina
Figure 7: A Proposal of a New Classification of Congenital Spinal Deformity.
Relationship of each category in the new classification to others presented previously.
Table: Patients with Vertebral Anomalies with sole Mismatch Phenomena
|
Case |
Sex |
Type |
Vertebral anomalies |
scoliosis |
|
1 |
M |
Anteroposterior |
Rt.T3(FSHV+discordant SSHL), Rt.T7 & Rt.T11(SSHV+SSHL), Lt. L5(FSHV+SSHL) |
60 |
|
2 |
F |
Anteroposterior |
Lt.T8, Rt.L1 (FSHV+discordant FSHL) |
55 |
|
3 |
M |
Anteroposterior |
Lt. T10(FSHV+FSHL)、Rt.T12(SSHV、discordant FSHL) |
19 |
|
4 |
F |
Anteroposterior |
Rt.T3 (FSHV+discordant FSHL), Lt.T6(FSHV+SSHV), Rt.T8(FSHV+SSHL),Lt.T10( SSHV+discordant SSHL) |
32 |
|
5 |
F |
Anteroposterior |
Lt.T7 (FSHV+discordant FSHL), Rt.T10 (SSHV+discordant SSHL), Lt.L1 (SSHV+discordant SSHL) |
35 |
|
6 |
M |
Anteroposterior |
Lt C7(SSHV+NL)、Rt T7(SSHV+NL), T8-T10 Hemilamina |
51 |
|
7 |
M |
Anteroposterior |
Lt.T10 (FSHV+discordant FSHL), T12(BV), Rt. L2(FSHV+SSHL), Lt.L6 (pedicle defect) |
45 |
|
8 |
F |
Anteroposterior |
Rt T1(SSHV+FSHL), Lt.T8 (FSHV+NL), Rt.T10 (SSHV+NL)、Rt.T13(SSHV+NL) |
32 |
|
9 |
F |
Anterior |
Lt. T1 (FSHV+NL)、Rt. T8 (FSHV+NL)、Lt. T13 (FSHV+NL) |
65 |
|
10 |
F |
Anterior |
Lt. L2 (FSHV+NL), Rt. L4 (SSHV+NL) |
36 |
|
11 |
F |
Posterior |
Lt. T5 (NVB+FSHL), Rt.T6 (NVB+FSHL) |
33 |
|
12 |
M |
Posterior |
Rt.T6(NVB+FSHL), Lt.T8 (NVB+SSHL), Lt.T9 (NVB+SSHL), Rt. T10 (NVB+FSHL) |
40 |
FSHV: fully-segmented hemivertebral body, SSHV: semisegmented hemivertebral body, BV: butterfly vertebra
FSHL: fully-segmented hemilamina, SSHL: semisegmented hemilamina, NVB: normal vertebral body, NL: normal lamina
D i s c u s s i o n
Congenital spinal deformity is defined as a spinal deformity due to congenitally abnormal vertebrae. Congenital scoliosis, kyphosis, and their combination, kyphoscoliosis, are often encountered in scoliosis clinics. Winter and McMaster presented the classification of congenital scoliosis with three types, formation failureW, segmentation failureW, and mixed typeW [1, 2, 7]. On the other hand, McMaster & Singh also introduced a classification for congenital kyphosis that shared basic concepts with the classification for congenital scoliosis [3]. The differences among these are whether the anterior structure of vertebral anomalies predominates over the posterior, or the lateral. These classifications have been accepted in the world for more than 20-30 years due to their simplicity and easily understood nature.
However, congenital spinal deformities vary greatly in their types, numbers, and existence of segmentation of vertebral anomalies causing spinal deformity. Both Winter and McMaster paid close attention to the abnormalities of the vertebral body because plain X-ray images that were used for evaluation had shown anterior structure much more clearly than the posterior structure. Limited quality in resolution and two-dimensional images impeded attention to the abnormalities in posterior structure in their days [1-3, 7].
Recent developments in technology have made it possible to reconstruct three-dimensional images from axial CT images and demonstrated the ability to visualize the three-dimensional morphology of CSD with not only vertebral body anomalies but also several types of abnormalities in the posterior structure just the same as those seen in the anterior structure. Several authors investigated and presented the usefulness of 3D-CT images in clinical practice of spinal deformities [8, 9 ,10]. Nakajima, et al. presented several types of posterior structure of vertebral anomalies in formation failure and first reported existence of discordancy between the anterior and the posterior structure [5].
Kawakami, et al. reported a classification of CSD that was consisted of four types, SS, MS, MC, and SFK [7]. The SS describes existing solitary abnormal vertebra with formation failure and one third of patients belonged to this type in this study. MS includes multiple vertebral anomalies that strongly relate to the onset of CSD without any accordant relationship between anterior and posterior structure. In this study, 66 patients were recognized of possessing this type. SFK should be limited only for CSD with no formation defect but with some segmentation defects. If a formation defect occurs in conjunction with some segmentation defects, such CSD should not be classified into this type. In our series, many patients had formation defects in addition to segmentation defects even in the same level. These patients belonged to MC and not in SFK. Consequently, only 35 patients exhibited pure type of segmentation defects.
The use of MC by Kawakami et al. was analogous to the mixed type by Winter, as a way to group anomalies that did not fit the respective classification scheme. In other words, it was sort of a box labeled “other”, for those anomalies that were somehow different from the rest. This ambiguity may have been a necessity in the time of two-dimensional imaging; however, investigation by Kawakami, et al. of three-dimensional modeling it has been demystified one step further by subdividing MC into MMC and CM. This study was conducted to investigate the MMC in greater detail. 19 patients out of 124 in this study could be classified into three groups in terms of discordancy between the anterior and the posterior structure. As described in the results, the first type exhibited normal vertebral bodies with multiple hemilaminae (Posterior mismatch type). The second type exhibited multiple hemivertebral bodies with normal laminae (Anterior mismatch type). The third type exhibited a discordant combination of hemivertebral bodies and hemilaminae (Anteroposterior mismatch type). While they may have the appearance that resembles some other type of formation failure in spite of existence of discordancy, they should not be grouped in either formation failureW or segmentation failureW. In fact, previously they had been jumbled together into the Mixed typeW by Winter’ and McMaster’ classification, as the mismatch phenomena were not recognized.
Although developmental mechanisms of the mismatch phenomena are not yet known, it could be hypothesized as an embryonic false fusion of bilateral vertebral germs during the somite period. This is a time when the bilateral sclerotomes that originate from the somites couple and differentiate into the vertebrae and ribs. Tsou reported the development mechanism of hemivertebrae; a single hemivertebra is formed by hemimetameric asynchronous development, which is thought as false fusion of primordia during this period [11]. Saito, et al. three-dimensionally investigated hemimetameric shift and presented two types; unison and discordant type [12]. The latter was the same as those that were classified into the Posterior type or the Anteroposterior type in this study. Lehman reported that contralateral hemivertebrae were formed by false coupling of somites [13]. Based on these developmental considerations, the mismatch phenomena should be separated from formation failureW, which can be explained by the concept of partial formation defect of vertebrae. We have placed these three types that occur due to the mismatch phenomena together and have termed it as “Coupling failure (CF)”, which should be regarded as the fourth category of CSD.
The Mixed typeW in the classification presented by Winter and McMaster and the Mixed complex type in the classification by Kawakami, et al. could be regarded as an assembly of multiple vertebral anomalies due to combination of formation, segmentation, and/or coupling failure. In another word, this type can be expressed “Mixed failure.” The rest 26 patients in this study, who had coupling failure with some segmentation defects and/or some formation defects, should belong to the Mixed failure.
The new category “Coupling failure,” introduced in this paper will play an important role in clinical practice. First, once coupling failure is diagnosed using 3DCT images, surgeons will be able to approach target vertebrae without disorientation; thus, avoiding wrong level surgery and can contribute in preventing over-exposure. Second, with the addition of coupling failure, prediction of the natural courses of each type of CSD may become more reliable, particularly for those involving formation failureW. In the future, new information regarding the natural history of CSD may be possible by the accumulation of 3DCT images of formation failureK with the combination of MRI images. Third, although many studies regarding surgical outcomes of vertebrectomy have been reported in the literature, those outcomes and surgical complications vary significantly between surgeons to surgeons. One reason that can be proposed for this phenomenon is that previous studies may include both hemivertebral bodies with coupling failure and with formation failureW without differentiating between the two. The occurrence of postoperative complications including re-progression and junctional kyphosis may be influenced by existence of mismatch phenomena in formation failureW. There are two main limitations of this classification, which are the requirement of 3DCT images and a learning curve to read the images correctly. Although obtaining 3DCT images require some irradiation exposure, it is definitely important to make a correct diagnosis and to form an appropriate strategy for surgery in CSD. If these processes are noncommittal, some patients with CSD who are surgically treated may be thrown into much serious complications that may otherwise be preventable; such situations must require more irradiation exposure due to repeated X-ray and CT check-ups.
With respect to the learning curve issue, reading 3DCT images of more complicated CSDs correctly may be an issue. It takes time to learn how to read. Some of CSD are too complicated to read by a veteran surgeon even when using high-resolution 3DCT images. For such CSDs, recent development of three-dimensional plastic models constructed using a 3D-printer from 3DCT DICOM data may be great help to understand three-dimensional anatomical relationship between the anterior and posterior structure.
C o n c l u s i o n
A new category of vertebral anomalies was introduced and was termed “Coupling failure”, which was completely different from both formation failureK and segmentation failureK in terms of developmental mechanism and common morphological characteristics in these three types. Coupling failure was defined as vertebral anomalies with either anterior or posterior discordancy, or both (Anterior, Posterior, Anteroposterior type). By adding to the coupling failure, congenital spinal deformity may be classified more clearly into four categories, Formation failureK, Coupling failure, Segmentation failureK, and Mixed failure (Figure 7). This new classification may lead us to better understanding of the morphological characteristics of CSD and provide us with the tools to solve previously unsolved problems that were often encountered in clinical practice
Funding
This study was not provided any financial support for the conduct of the research and/or preparation of the article
Conflict of Interests
Authors do not have any conflict of interests related to this work.
Acknowledgements
We would like to acknowledge Sachiko Hiraiwa, Naoko Kojima, for their help in preparing X-Rays and clinical charts.
The authors would also like to thank Enago (www.enago.jp) for the English language review.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 19, Mar 2018Accepted: Mon 02, Apr 2018
Published: Fri 06, Apr 2018
Copyright
© 2023 Noriaki Kawakami. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2018.10.002
Author Info
Kazuki Kawakami Noriaki Kawakami Ryoji Tauchi Toshiki Saito
Corresponding Author
Noriaki KawakamiDepartment of Orthopaedics and Spine Surgery, Meijo Hospital
Figures & Tables
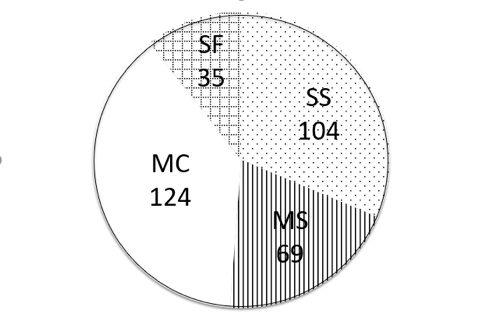
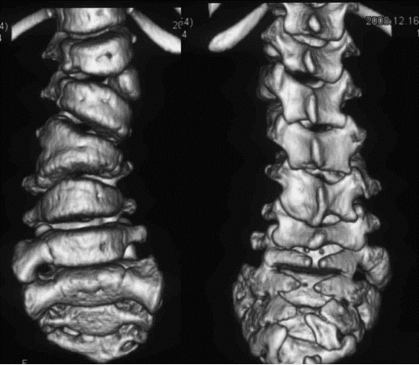
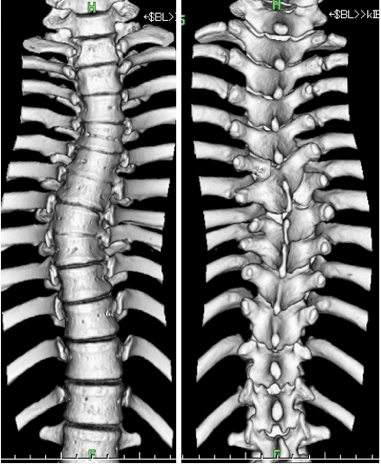
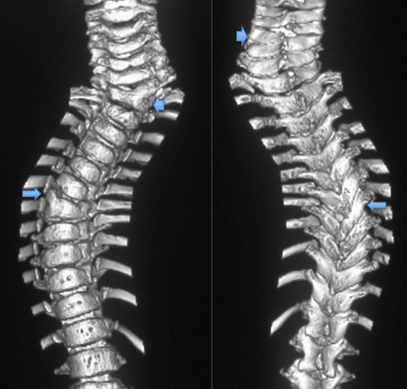


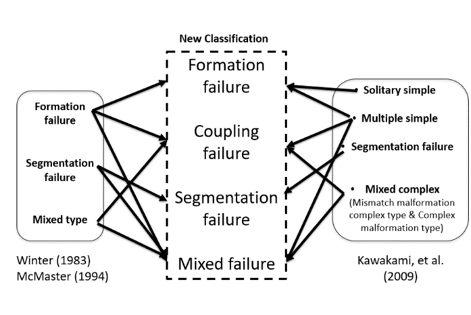
Figure legends
Fig. 1: Types of Vertebral anomalies in 332 patients
Fig. 2: The Anterior type of Coupling failure
While laminae demonstrated almost normal shape with a little bit asymmetry except of sacral spina bifida, two contralateral hemivertebrae exist.
Fig. 3: The Posterior type of Coupling failure
Lt. hemilamina of T5 and Rt. Hemilamina of T6 exists although vertebral bodes of T5, T6, T7, T8 looks normal with disc space narrowing on T5/6, T7/8.
Fig. 4: The Anterosterior type of Coupling failure
Anterior structure: a butterfly vertebra on C5, semisegmented hemivertebral body on lt. C7 (arrow), and semisegmented hemivertebral body on rt. T7 (arrow).
Posterior structure; a semisegmented hemilamina on the lt. C5 with a normal lamina on T1 (arrow), and a fully-segmented hemilamina on the rt. T8 (arrow).
Fig. 5: The Mixed failure: multiple vertebral anomalies with formation, coupling, and segmentation failure.
Anterior structure: a semisegmented hemivertebral body on the rt. T5 (arrow) and semisegmented vertebral body on the lt. T8 (arrow). With T6 & T7 fused congenitally.
Posterior structure: Two small contralateral semisegmented hemilaminae on the rt. T5 (arrow) and the lt. T8 (arrow).
Fig. 6: The Mixed failure: A hemivertebral body with a discordant hemilamina
A semisegmented hemivertebral body exists on L4 with normal lamina
Fig. 7: A Proposal of a New Classification of Congenital Spinal Deformity.
Relationship of each category in the new classification to others presented previously.
Table: Patients with Vertebral Anomalies with sole Mismatch Phenomena
|
Case |
Sex |
Type |
Vertebral anomalies |
scoliosis |
|
1 |
M |
Anteroposterior |
Rt.T3(FSHV+discordant SSHL), Rt.T7 & Rt.T11(SSHV+SSHL), Lt. L5(FSHV+SSHL) |
60 |
|
2 |
F |
Anteroposterior |
Lt.T8, Rt.L1 (FSHV+discordant FSHL) |
55 |
|
3 |
M |
Anteroposterior |
Lt. T10(FSHV+FSHL)、Rt.T12(SSHV、discordant FSHL) |
19 |
|
4 |
F |
Anteroposterior |
Rt.T3 (FSHV+discordant FSHL), Lt.T6(FSHV+SSHV), Rt.T8(FSHV+SSHL),Lt.T10( SSHV+discordant SSHL) |
32 |
|
5 |
F |
Anteroposterior |
Lt.T7 (FSHV+discordant FSHL), Rt.T10 (SSHV+discordant SSHL), Lt.L1 (SSHV+discordant SSHL) |
35 |
|
6 |
M |
Anteroposterior |
Lt C7(SSHV+NL)、Rt T7(SSHV+NL), T8-T10 Hemilamina |
51 |
|
7 |
M |
Anteroposterior |
Lt.T10 (FSHV+discordant FSHL), T12(BV), Rt. L2(FSHV+SSHL), Lt.L6 (pedicle defect) |
45 |
|
8 |
F |
Anteroposterior |
Rt T1(SSHV+FSHL), Lt.T8 (FSHV+NL), Rt.T10 (SSHV+NL)、Rt.T13(SSHV+NL) |
32 |
|
9 |
F |
Anterior |
Lt. T1 (FSHV+NL)、Rt. T8 (FSHV+NL)、Lt. T13 (FSHV+NL) |
65 |
|
10 |
F |
Anterior |
Lt. L2 (FSHV+NL), Rt. L4 (SSHV+NL) |
36 |
|
11 |
F |
Posterior |
Lt. T5 (NVB+FSHL), Rt.T6 (NVB+FSHL) |
33 |
|
12 |
M |
Posterior |
Rt.T6(NVB+FSHL), Lt.T8 (NVB+SSHL), Lt.T9 (NVB+SSHL), Rt. T10 (NVB+FSHL) |
40 |
FSHV: fully-segmented hemivertebral body, SSHV: semisegmented hemivertebral body, BV: butterfly vertebra
FSHL: fully-segmented hemilamina, SSHL: semisegmented hemilamina, NVB: normal vertebral body, NL: normal lamina
References
1. Winter RB (1973) Congenital Scoliosis. Clin Orthop & Relat Res 93: 75-94.
2. Winter RB (1983) Congenital Deformities of the Spine. New York, NY: Thieme-Stratton.
3. McMaster MJ, Singh H (1999) The Natural history of congenital kyphosis and kyphoscoliosis. J Bone Joint Surg Am 1: 1367-1383. [Crossref]
4. Winter RB, Lonstein JE (2010) Scoliosis Secondary to a Hemivertebra: Seven Patients with Gradual Improvement Without Treatment. Spine 35: E49-E52. [Crossref]
5. Nakajima A, Kawakami N, Imagama S, et al. (2007) Three-Dimensional Analysis of Formation Failure in Congenital Scoliosis. Spine 32: 562-567. [Crossref]
6. Kawakami N, Tsuji T, Imagama S, Lenke LG, Puno RM, et al. (2009) Classification of Congenital Scoliosis and Kyphosis. A New Approach to the Three-Dimensional Classification for Progressive Vertebral Anomalies Requiring Operative Treatment. Spine 34: 1756-1765. [Crossref]
7. McMaster MJ (1994) Congenital Scoliosis. In the Pediatric Spine (Weinstein SL. edit.) Raven Press, New York, 227-244.
8. Newton PO, Hahn GW, Fricka KB, Wenger DR, (2002) Utility of three dimensional and multiplanar reformatted computed tomography for evaluation of pediatric congenital spine abnormalities. Spine 27: 844-850. [Crossref]
9. Hedequist DJ, Emans JB (2003) The correlation of preoperative three-dimensional computed tomography reconstructions with operative findings in congenital scoliosis. Spine 28: 2531-2534. [Crossref]
10. Rubin GD (2003) 3-D imaging with MDCT. Eur J Radiol 45 (Suppl 1): 37-41. [Crossref]
11. Tsou PM, Arthur Y, Hodgson AR (1980) Embryogenesis and prenatal development of congenital vertebral anomalies and their classification. Clin Orthop & Relat Res 152: 211-231.
12. Saito T, Kawakami N, Tsuji T, Ohara T, Suzuki Y, et al. (2016) Three-Dimensional Analysis of Hemimetameric Segmental Shift. J Pediatr Orthop in print. [Crossref]
13. Hermann Lehmann-Facius (1925) Die Keilwirbelbildung bei der kongenitalen Skoliose. Frankfurt Z.Path 31: 489.
