Journals
Conceptual model to optimize implant positioning in edentulous mandible treated with an over denture; A case series preliminary report
A B S T R A C T
Statement of problem:
There are no clear diagnostic guidelines for producing a mandibular implant overdenture (IOD).
Purpose:
The aim of this clinical report was to present a set of principles that can be used during diagnosis and treatment planning for later ideal implant positioning and promotion of optimal patient-centered outcomes.
Materials and Methods:
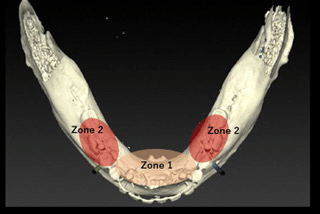
With our novel method for determining an ideal implant position, the mandibular arch is divided into 3 zones (Zone 1, 2, 3) according to the relationship between the alveolar crest and artificial tooth position. Following implant placement, the patient is provided with a mandibular IOD.
At the 2-year follow-up evaluation of prostheses placed in 2 patients, the chief complaints were totally resolved, and no complications were noted.
Conclusions:
Although out findings are limited, they indicate that the present diagnostic method for planning mandibular IOD treatment results in a good outcome. Future well-designed clinical studies are necessary before making definitive conclusions.
Keywords
implant over denture (IOD), implant positioning, zoning method, locator attachment
I N T R O D U C T I O N
Complete function of removable dentures in fully edentulous patients is often inadequate. In particular, severe atrophy of the alveolar crest makes it difficult to wear a conventional denture appliance because of lack of retention and inherent instability. Together with the poor load-bearing capacity of related tissues, oral pain and poor oral function are often the result. Thus, use of implants has become a well-established clinical method to treat edentulous patients [1]. Implant overdenture (IOD) therapy has significantly increased in popularity in recent years and shown to lead to improved oral health clinical function and quality of life [2]. The primary focus of early clinical studies of IODs was survival of implants and issues related to oral hygiene, while more recently prosthetic maintenance and economic aspects in the context of value-based dentistry have been the focus of various studies [3]. In addition, complications associated with mandibular IODs, comparisons of retention devices, OD maintenance, and related costs have been reported [4, 5, 9, 11, 14]. IODs require more involvement regarding diagnosis and treatment planning than a conventional complete denture. Furthermore, an important consideration when fabricating a mandibular IOD is confirmation of sufficient space for the prosthetic components of the implant attachment system, as inadequate space can result in an excessive occlusal vertical dimension, an over-contoured prosthesis, and prosthesis fracture, resulting in patient dissatisfaction [1, 2]. Unfortunately, no guidelines related to principles used when considering the positioning of implants to support an optimally functioning mandibular overdenture are available. Optimal implant placement diminishes the risks of denture fracture, attachment damage, and weak denture retention, as well as the ensuing compromises in function and patient quality of life.
The aim of this clinical report was to develop a set of principles to use during diagnosis and treatment planning for ideal implant positioning and promotion of an optimal patient-centered outcome.
Clinical Report
Diagnosis and treatment planning
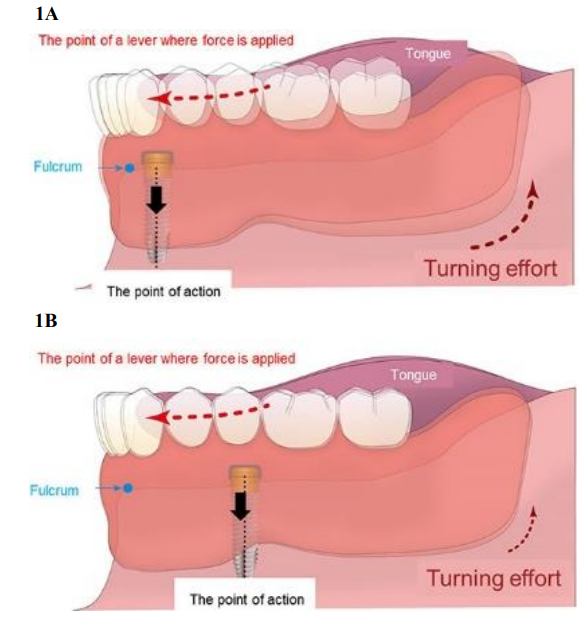
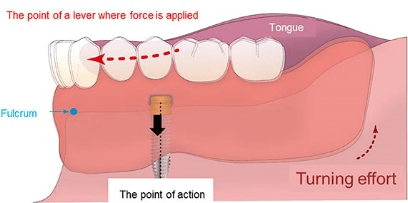
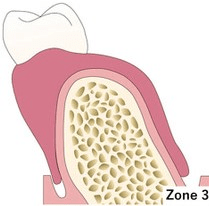
An IOD is a useful choice for diagnosis of an edentulous mandible and residual ridge resorption, as well as an unstable, non-retentive, and poorly fitting denture [4]. The aim of such treatment is to improve patient quality of life by providing a functional dentition for the mandible in order to increase the ability to chew harder foods, while concurrently producing a long-lasting and durable prosthesis. Al-Ghafli, et al. reported that improper implant angulation has negative effects on attachment retention and longevity in cases with IOD treatment and is a possible limiting factor for achieving an optimal treatment outcome [5]. To achieve an ideal outcome, implants should be placed as parallel as possible to each other directly below artificial teeth. In addition, since complete denture mandibular movement must occur when the tongue is moved in a superior or anterior direction, a lever effect is created to lift the complete denture based on the line across the crest of the alveolar ridge between the two implants acting as a fulcrum line. To reduce such movement, implants should be placed in a manner so as to yield only limited movement of the denture around the fulcrum line (Figure 1A, B). This treatment objective requires a more distal placement position, within the anatomical opportunities and constraints of each case, in order to move the fulcrum line in a distal manner.
Figure 1 A,B: When the implant point of attachment becomes the point of action with tongue thrusting, the fulcrum is the anterior alveolar crest (blue) and the lever where force is applied is the anterior lingual surface of the artificial crown (red) (Figure 1A). To reduce denture turning, the implant should be placed as far as possible from the fulcrum point (Figure 1B).
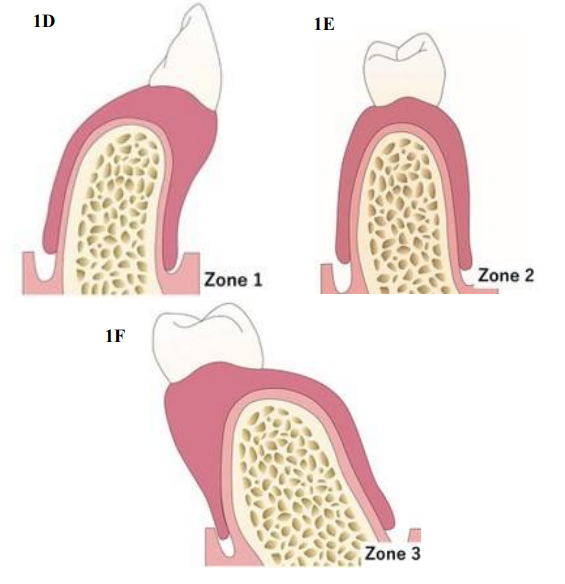
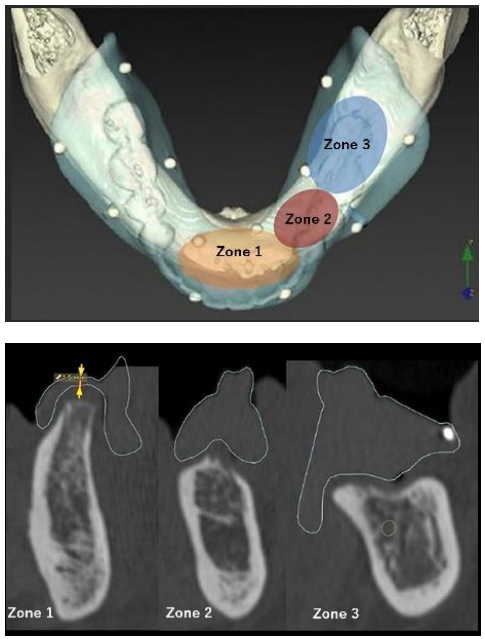
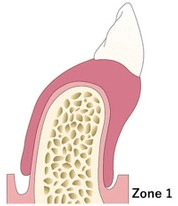
Figure 1 C: Relationship between line of alveolar crest (blue) and artificial crown (red). Zone 1 is the area anterior to the line from the artificial crown to alveolar crest. Zone 2 is the area where the line of the artificial crown and alveolar crest come together. Zone 3 is the area lingual from the artificial crown and positioned against the alveolar crest.
Figure 1 D,E,F: Each zone has individual characteristics. In proportion to the coronal section of each zone, an implant cannot be placed directly below the artificial crown in Zone 1 (Figure 1D) or 3 (Figure 1F). Furthermore, the thickness of the denture space is thin in Zone 1 and 3. In contrast, an implant can be placed just below the artificial crown in Zone 2 (Figure 1E), because of adequate thickness for the attachment.
In our proposed model, the mandibular arch is divided into 3 zones (Zone 1, 2, 3) according to the relationship between the alveolar crest and artificial tooth position (Figure 1C). Zone 1 is defined as the area in which the artificial teeth are positioned labial/buccal to the alveolar crest, thus implants cannot be placed directly below the artificial teeth in this zone. Furthermore, the denture (attachment housing space) is usually smaller in Zone 1, resulting in maintenance challenges and complications such as denture fracture, denture deformation, and weak denture retention (Figure 1D). Zone 2 is the area in which the artificial teeth are positioned so as to come together close to or directly over the alveolar crest. Implants positioned in this zone can be placed under the artificial teeth. Since the fulcrum line lies below the artificial teeth, there is less rotational movement of the denture during tongue movement, allowing the patient to masticate more effectively and eat more challenging foods. If sufficient bone quality and quantity is present in Zone 2, it is the preferred site for parallel bilateral implant placement (Figure 1E). Zone 3 is the area in which the artificial teeth are positioned lingual from the alveolar crest and implants in this zone cannot be placed directly below them (Figure 1F). Following diagnostic procedures to determine the desired artificial tooth position and availability of bone for implant placement, the mandible can be zoned according to the aforementioned classification system and optimal implant placement in Zone 2 is preferred. This classification system is particularly helpful because it has prognostic value, with implants placed in Zone 2 predicted to yield a better prognosis and patient-centered outcome. For investigating patient’s satisfaction against their prosthesis, OHIP-14 questionnaire test was completed [6].
Representative cases
Patient 1
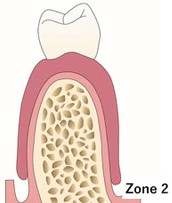
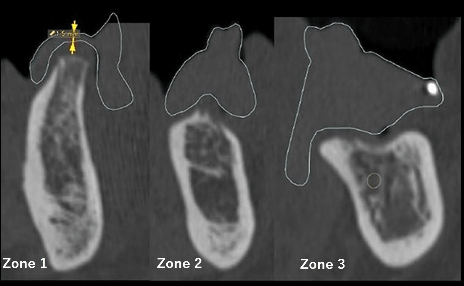
A 60-year-old man came to our dental clinic with poor chewing function while using a mandibular removable complete denture. During the clinical examination, it was noted that the patient was wearing a Kennedy Class I removable partial denture on the maxillary arch with sufficient stability (Figure 2A, B). However, the mandibular complete denture was non-retentive, and the patient stated that he could not eat hard foods. The sore of OHIP-14 questionnaire test was 33 points. This score suggested his huge stress and unsatisfaction about his mandibular prosthesis. For obtaining additional diagnostic information, computerized tomography (CT) scanning was performed with the patient wearing the removable denture (Figure 2C). It was determined that the patient had large Zone 1 and Zone 3 areas (Figure 2D). Sagittal CT images revealed that sufficient bone volume for implant placement existed in Zone 1, though the thickness of the denture (attachment housing space) would be too small, making the prosthesis vulnerable to deformation and/or fracture. Sagittal CT imaging (Fig. 2E) of the Zone 2 area revealed plenty of bone to accommodate implant placement that would allow for placement of 2 implants just under the overlying artificial teeth (on the same axis). In addition, the implants could be placed parallel to each other in the Zone 2 region.
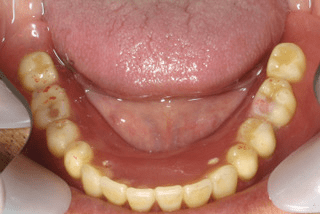
Figure 2A: Occlusal view of mandible showing resorbed mandibular ridge.
Figure 2B: Occlusal view of maxilla.
Figure 2C: CT image showing occlusal view of mandible with removable denture. The line of the artificial crown (solid line) different from that of the alveolar crest (broken line).
Figure 2 D,E: Zone 1, 2, and 3 are classified according to the relationship between the line of the alveolar crest and artificial crown (Figure 2D). Sagittal CT imaging (Figure 2E) revealed adequate bone for implant placement, though the thickness of the denture (attachment housing space) was thin in Zone 1. We were able to place the implant just below the artificial crown in Zone 2. There was insufficient bone volume for the implant placement in Zone 3.
A minimum of approximately 12 mm of vertical restorative space (crest of bone to occlusal plane) is considered necessary to provide assistance for a mandibular implant over a denture [6]. Therefore, the estimated attachment space was more than 15 mm above the implant, and 3 mm in both the buccal and lingual directions in this case. Treatment planning included placement of 2 implants in Zone 2. The Locator attachment system (Zest Anchors Inc) and Nobel Biocare implants (Nobel Biocare AB) were selected for this patient. With use of a surgical guide, 2 endosseous implants, each measuring 4.0 x 11.5 mm (Nobel Biocare Mk III), were inserted, with time allowed for healing after placement of cover screws and flap re-approximation. Eight weeks later, a second surgical procedure was performed during which the implants were exposed, and final abutments placed. A relationship of the Locator housings to the overdenture so as to attach the abutments was accomplished intraorally using acrylic resin, based on the manufacturer’s recommendations (Unifast, GC). During subsequent visits, minor denture adjustments were performed as necessary. At 1- and 2-year post-placement examinations, no complications were observed, and the patient reported that the previous poor chewing function had been completely resolved (Figure 2F, G, H, I). The sore of OHIP-14 questionnaire test was 5 points. Against the score of before treatment (33 points), his satisfaction about his prosthesis was quite improved.
Figure 2 F: Oral findings obtained 2 years after treatment. The final prosthesis was an implant-supported and retained mandibular complete denture, as opposed to a conventional mucosa tooth-supported partial denture.
Figure 2 G: Final appearance of prosthetic restoration and mucosal surface.
Figure 2 H: Intraoral view showing attachment devices mounted onto the implants.
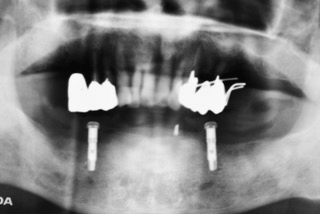
Figure 2 I: Radiological appearance of prosthetic field after insertion of dental implants and their osseous integration. Note the parallel positioning of the 2 implants.
Patient 2
A 57-year old man came to us in 2011 with a chief complaint of lack of denture stability and inability to properly chew food. During the clinical examination, we observed a bilateral cantilever removable partial denture on the maxillary arch, which had sufficient stability, support, and retention (Figure 3A, B). CT scanning was performed to assist in the diagnosis and treatment plan process. The sore of OHIP-14 questionnaire test before treatment was 24 points. This score suggested unsatisfaction about his mandibular prosthesis.
In the mandibular arch, the patient had a large Zone 1, while the Zone 3 area was negligible (Fig. 3C). Sagittal CT images (Figure3D) revealed that sufficient bone volume for implant placement was present in Zone 1, though denture thickness (attachment housing space) was minimal, and complications such as denture fracture and deformation of the denture would likely develop even if implants could be placed in Zone 1. Sagittal CT imaging of the Zone 2 area revealed sufficient bone volume for implant placement and that they could be placed below the artificial teeth. Furthermore, implants could be placed parallel to each other in Zone 2. The estimated attachment space was greater than 15 mm in the vertical, and 3 mm in the buccal and lingual directions. Therefore, implants were placed in Zone 2 using appropriate attachment (Locator; Zest Anchors Inc) and implant (Nobel Biocare AB) systems. With a surgical guide, 2 endosseous implants measuring 4.0 x 11.5 mm (Nobel Biocare Mk III) were placed and then 8 weeks were allowed for healing, after which a second surgical procedure was performed to uncover the implants. Final Locator abutments were then placed, along with housings related to the attachments and denture directly in the mouth (Figure 3E, F, G). Denture adjustments were performed as necessary. At the 2-year evaluation of the prosthesis (Figure 3H, I, J, K), the chief complaints of the patient were totally resolved, and no complications had occurred. 4-year after the treatment, the sore of OHIP-14 questionnaire test was 9 points. Against the score of before treatment (24 points), his satisfaction about his prosthesis was quite improved.
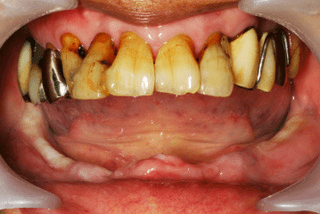
Figure 3A: Frontal view obtained prior to treatment, without mandibular denture.
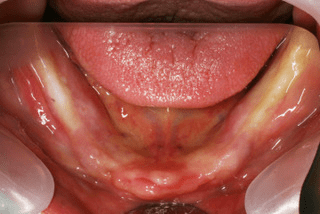
Figure 3B: Occlusal view of mandible.
Figure 3 C,D: CT image showing occlusal view of mandible with removable denture. Zone 1 and 2 were classified based on the relationship between the line of the alveolar crest and the artificial crown (Figure 3C). There was no Zone 3 in this patient. Sagittal CT imaging (Figure 3D) revealed that adequate bone for implant placement existed, though the thickness of the denture (attachment housing space) was thin in Zone 1. We were able to place the implant just below the artificial crown in Zone 2.
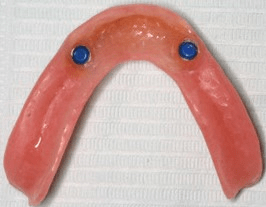
Figure 3E: Occlusal appearance of intaglio surface used as attachment space.
Figure 3F: Occlusal appearance immediately after attachment of the denture. Acrylic resin can be seen exiting from the vent hole.
Figure 3G: Attachments on abutments prior to transfer. Spacer rings were placed over the abutments to prevent acrylic resin from sticking to the attachments.
Figure 3H: Frontal view obtained 2 years after treatment. The finished prosthesis was an implant-supported and retained mandibular complete denture, as opposed to a conventional mucosa tooth-supported partial denture.
Figure 3I: Final prosthetic restoration.
Figure 3J: Intraoral view showing attachment devices mounted to the Implants.
Figure 3K: Radiological appearance of prosthetic field after insertion of dental implants and their osseous integration.
Discussion
No previous report has described a method for determining optimal implant positioning that provides both retention and support of an overdenture. McGill and York proposed that a mandibular 2-implant overdenture be the first choice for edentulous patients. In terms of the number of implants needed to yield patient satisfaction, a 2-implant retained overdenture is a well-accepted treatment option, as oral hygiene is facilitated, and easy modification of the prosthesis base is possible without great financial burden associated with a fixed implant complete denture [7-9]. Jemt, et al. noted cumulative success rates of 94.5% and 100% for implants and overdentures, respectively [10]. In the present cases, following IOD treatment, patient complaints were totally resolved. Especially in terms of mastication disorder when eating harder foods, both were able to crush hard foods easily because of the strong bite support provided by the 2 implants. For maintenance and treatment, the patients visit our clinic every 3 months, at which time we examine the denture, implant, and other residual teeth, and adjust the IOD as necessary. Every year at the maintenance recall examination, the retention discs are changed. During the study period, no complications, such as marginal bone loss around the implant or denture fracture, or denture attachment breakage, were noted.
One of the most compromising factors contributing to denture instability is tongue thrusting, as it elevates the anterior lingual aspect of the denture, thus generating a class II lever mechanism. In this scenario, the fulcrum is the anterior alveolar crest and the point of force where the lever is created is the anterior lingual aspect of the denture. Therefore, an implant should be positioned as far as possible from the fulcrum point in order to have maximum effect. Both of our patients enjoyed improved sufficient denture stability during wide mouth opening and loud speaking, a benefit likely attained by positioning the implants to oppose denture instability (Figure 1A, B). With our zoning method, the relationship of the line between the artificial crown and alveolar crest in CT images is noted, then the intersection area of those lines is determined (Zone 2).
For best results, we recommend implant placement near Zone 2, within the individual anatomical limitations. One advantage of choosing Zone 2 for implant placement is that 2 implants can be directly placed under the artificial crown (on the same axis), while another factor is the ability to position the implants in parallel. Regarding parallel implant positioning for IOD treatment, Ortegón SM reported that there was decreased retention in patients with divergent implants and divergent attachments as compared to those with parallel implants and parallel attachments [11]. The present patients noted satisfaction with denture retention during use and the durability of the attachment was high, which was likely because of the parallel positioning. Furthermore, no denture fracture occurred throughout the observation period in either case, likely because of the use of Zone 2, which has sufficient space for the prosthetic components of the implant attachment system. On the other hand, Zone 1 does not have sufficient space for prosthetic components, resulting in maintenance challenges and complications, such as denture fracture, deformation, and weak retention. When an implant is not directly placed under an artificial crown it becomes difficult to chew harder food, which is an important factor in patient quality of life. Generally, an edentulous patient will lose the ability to have an optimal chewing cycle and maximum bite force is reduced, leading to oral frailty. Shimada, et al. found a significant relationship between oral frailty and mild cognitive impairment and Kwok, et al. reported that poor oral function results in a low body mass index (BMI) score [12, 13]. For avoiding or solving such problems, not only recovery from mastication disorders but also appropriate nutrition instructions are needed. The body mass index score of the present case 1 patient was 19.5 following IOD treatment, as compared with 18.5 prior to treatment. From this point of view, Zone 2 is considered the ideal area for implant placement for mandibular IOD treatment.
In this study, we show only 2 cases of IOD treatment. The average improvement of OHIP-14 score of another 9 cases (data not shown) of mandibular IOD patient planed using our Zoning method is 16.6 points. The sample size is still small, but the change of OHIP-14 questionnaire score before and after treatment suggest the efficacy of our method. We will continue to investigate. The proposed zoning method considers the relationship between artificial tooth position and alveolar crest position, and seeks to find the intersection in Zone 2, which is the recommended location for implant placement. Nevertheless, it should be noted that the position of Zone 2 varies widely among patients according to the shape of the alveolar bone crest as well as the position of artificial teeth, thus a diagnostic stent is required for diagnosis and treatment planning. In addition, anatomical restrictions, such as positioning of the inferior alveolar nerve and mental foramina, must be considered.
Summary
The present proposed novel zoning method considers the relationship between artificial tooth position and alveolar crest position and seeks to find the intersection in Zone 2. This classification system is particularly helpful because implants placed in Zone 2 typically yield better prognosis and patient-centered outcomes.
Disclosure
The authors have no conflicts of interest to declare in association with this study.
Article Info
Article Type
Case ReportPublication history
Received: Tue 12, Mar 2019Accepted: Sat 30, Mar 2019
Published: Wed 10, Apr 2019
Copyright
© 2023 Kouhei Shinmyouzu. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2019.02.01
Author Info
Kazuhiko Kaneda Kouhei Shinmyouzu Maki Nishimura Saho Kobayashi Takuya Yamada
Corresponding Author
Kouhei ShinmyouzuTanpopo Dental Clinic, Tokyo, Japan
Figures & Tables















References
- Esposito M, Hirsch JM, Lekholm U, Thomsen P (1998) Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci 106: 527-551. [Crossref]
- Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ et al. (2002) The McGill consensus statement on Overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology 19: 3-4. [Crossref]
- Bassi F, Carr AB, Chang TL, Estafanous EW, Garrett NR et al. (2013) Functional outcomes for clinical evaluation of implant restorations. Int J Prosthodont 26: 411-418. [Crossref]
- Nishimura I, Atwood DA (1994) Knife-edge residual ridges: a clinical report. J Prosthet Dent 71: 231-234. [Crossref]
- Al-Ghafli SA, Michalakis KX, Hirayama H, Kang K (2009) The in vitro effect of different implant angulations and cyclic dislodgement on the retentive properties of an overdenture attachment system. J Prosthet Dent 102: 140-147. [Crossref]
- Sousa PC, Mendes FM, Imparato JC, Ardenghi TM (2009) Differences in responses to the Oral Health Impact Profile (OHIP14) used as a questionnaire or in an interview. Braz oral res 23: 358-364. [Crossref]
- Pasciuta M, Grossmann Y, Finger IM (2005) A prosthetic solution to restoring the edentulous mandible with limited interarch space using an implant-tissue-supported overdenture: a clinical report. J Prosthet Dent 93: 116-120. [Crossref]
- Ekelund JA, Lindquist LW, Carlsson GE, Jemt T (2003) Implant treatment in the edentulous mandible: a prospective study on Branemark system implants over more than 20 years. Int J Prosthodont 16: 602-608. [Crossref]
- Gotfredsen K, Holm B (2000) Implant-supported mandibular overdentures retained with ball or bar attachments: a randomized prospective 5-year study. Int J Prosthodont 13: 125-130. [Crossref]
- Naert I, Gizani S, Vuylsteke M, Van Steenberghe D (1999) A 5-year prospective randomized clinical trial on the influence of splinted and unsplinted oral implants retaining a mandibular overdenture: prosthetic aspects and patient satisfaction. J Oral Rehabil 26: 195-202. [Crossref]
- Jemt T, Chai J, Harnett J, Heath MR, Hutton JE et al. (1996) A 5-year prospective multicenter follow-up report on overdentures supported by osseointegrated implants. Int J Oral Maxillofac Implants 11: 291-298. [Crossref]
- Ortegon SM, Thompson GA, Agar JR, Taylor TD, Perdikis D (2009) Retention forces of spherical attachments as a function of implant and matrix angulation in mandibular overdentures: an in vitro study. J Prosthet Dent 101: 231-238. [Crossref]
- Shimada H, Makizako H, Doi T, Yoshida D, Tsutsumimoto K et al. (2013) Combined prevalence of frailty and mild cognitive impairment in a population of elderly Japanese people. J Am Med Dir Assoc 14: 518-524. [Crossref]
- Kwok T, Yu CN, Hui HW, Kwan M, Chan V (2004) Association between functional dental state and dietary intake of Chinese vegetarian old age home residents. Gerodontology 21: 161-166. [Crossref]