Journals
Comparison of In Vitro Dose Perturbation Effects of Amalgam, Composite Resin, Glass Ionomer Cement and Ketac Silver During Head and Neck Radiation with Photon Beam
A B S T R A C T
The most common oral manifestation from head and neck radiotherapy is mucositis. A part of complications is backscattering from metallic dental materials in radiation field, resulting in a dosage enhancement at the tissue-metal interface. The proper management of the patient’s restorative materials must be performed preoperatively to reduce these complications. This research compared the relative dose enhancement (RDE) in the different restorative materials (Amalgam, Composite resin, Glass ionomer cement and Ketac Silver®), the different tooth preparations (Class I, Class I other, Class II MOD, Cusp Tipping and Core build-up) and the location of ionizing chamber (buccal, occlusal, lingual surface). The dimension of controlled 20 teeth are as followed lower third molar, buccolingual width (10.41±0.82mm), mesiodistal width (11.28±0.72mm), dentin and enamel buccolingual width (1.5±0.5mm). The experiment is set using a modular radiation beam analyzer with at least 2 cm water as soft tissue equivalent material, 3 times irradiated with LINAC 6MV 200MU. The backscattering occurred in the amalgam filled tooth at the buccal and occlusal aspect in every preparation. The highest RDE occurring at the buccal aspect of cusp tipping amalgam filled tooth was 2.7%. In the lingual aspect, every preparation of amalgam filled tooth demonstrated lower RDE. The composite resin and glass ionomer cement produced low backscattering, while Ketac Silver® produced higher RDE. For any amalgam restorations in the radiation field, we recommended using the one-layer glass ionomer technique, which is suitable in preparing patient ahead of head and neck radiation. The recommended filling technique may decrease mucositis the adjacent area and improve the patient’s quality of life.
Keywords
Backscatter dose, forward scatter dose, Co-60 gamma-ray, dental restorative material
Introduction
Radiation therapy plays an important role in the treatment of patients suffering from head and neck cancer. The purpose of radiotherapy is to eradicate a tumor by exposing it to ionizing radiation. Ideally, radiation therapy is well-tolerated by surrounding structures, while in practice, some degree of transient or permanent tissue damage invariably occurs. In curative radiotherapy, the total radiation dose is high, and the treatment is usually prolonged and physically taxing. The oral complications from head and neck radiotherapy include xerostomia, loss of taste, mucositis, hyposalivation, radiation caries, periodontal disease, osteoradionecrosis, and trismus.
The presence of metallic dental materials in the radiation field results in a dosage enhancement at the tissue-metal interface. This enhancement is caused by the interaction of ionizing radiation with the atoms of the metal. When high-energy photons or electrons are liberated from the metal and set into motion in an opposing direction to that of the primary radiation beam, backscattered radiation results. The electron set into the same or similar direction that are referred to the primary beam. The dental restoration has a high atomic number this reason leads it to have a backscattering effect.
This was followed by a localized overdose of radiation. If the surrounding mucous membrane in this area lies directly against the metal surface, it is exposed to a considerably higher dose of radiation. Until now, damage to the neighboring soft tissue has appeared to be unavoidable. Thilman et al. assessed the degree of radiation scatter on tissue immediately adjacent to the endosseous and restorative dental alloys in the conventional radiation treatment and discovered substantial dose enhancement and attenuation [1].
Their results at the surface of different dental materials were the fixed golden caps (61%), the specimen containing gold (68%), the specimen of palladium (33%) and the specimen of amalgam (61%). The biological radiation effect at the spots of elevated dosage is higher than in their surroundings. Therefore, painful mucosa lesions may be expected, and the use of prophylactic measures should be adopted. Fuller et al. studied the effect of the accurate degree of dose disruption on the intended tissue target in computer-assisted tomotherapeutic intensity modulated radiation therapy (IMRT), which is an advanced form of three-dimensional radiation therapy [2]. Their study compared the measured dose enhancement in vivo and the calculated enhanced dose from IMRT affected by amalgam restoration but did not include composite resin, glass ionomer cement and KetacSilver® restorative material. In consequence, this study kept the focus on the relative dose enhancement from the restoration material to know the suitable materials in head and neck radiation patients.
Methods
In this study, we recruited 333 teeth from dental clinics for the measurement of dose perturbation. The mandibular third molars' human teeth were collected from 16 to 40-year-old and caries-free. Immediately after extraction, the teeth were thoroughly washed in running water and, in the case of human teeth, all blood and adherent tissue was eliminated by the clinician. The teeth were then be placed in normal saline at room temperature. We substituted ox dried bone for human jaws. The sizes of teeth measured by Vernier caliper was 10.41 mm in buccolingual (BL) width (SD=+0.41) and 11.28 mm in mesiodistal (MD) width (SD= +0.36). Before tooth preparation, every tooth was examined for the enamel and dentin thickness by radiographic method in MD and BL views and the thickness was measured by UNC-15 probe. The thickness of enamel and dentin was in between 1.5±0.5 mm for both views. All teeth’s characteristics excluded in this study were cavitated caries lesions larger than the preparation size (MDxBLxOC 2x5x2 mm), teeth with enamel hypoplasia or fluorosis, previously restored teeth, and the teeth with thickness of enamel and dentin smaller than 1.5±0.5mm in both views. After filling the cavity, every tooth was examined again for filling quality by radiographic method. If there was poor adaptation or void existed, the tooth was refilled. After completion of the restoration, the specimens were preserved in closed boxes at room temperature [3].
In this study divided into 20 categories (each category contained twenty-seven teeth). There were class I amalgam filling, class I other amalgam filling, class II MOD amalgam filling, cusp tipping amalgam filling and amalgam core build-up teeth, class I composite resin filling, class I other composite resin filling, class II MOD composite resin filling, cusp tipping composite resin filling and composite resin core build-up teeth, class I KetacSilver® filling, class I other KetacSilver® filling , class II MOD KetacSilver® filling, cusp tipping KetacSilver® filling and KetacSilver® core build-up teeth , Class I glass ionomer cement filling, class I other glass ionomer cement filling, class II MOD glass ionomer cement filling , cusp tipping glass ionomer cement filling and core build-up glass ionomer cement. Seven of sound teeth were used as control group. To pair the control tooth with the experimental tooth, we needed to measure the buccolingual width of each tooth, and the size must be equal or ±0.2 mm.
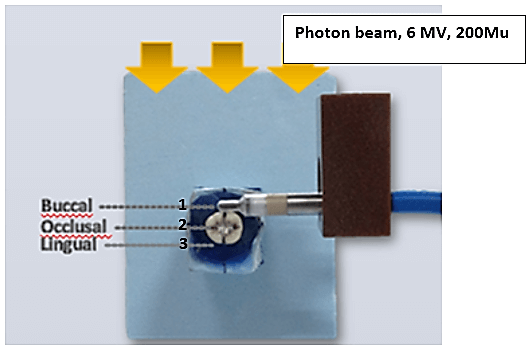
In this experiment, the sample tooth was irradiated, and the relative dose enhancement was measured from the primary beam at the same side as the radiation beam (buccal side) three times. Then the electron chamber position was moved to the occlusal and lingual side and the relative dose enhancement was measured (Figure 1). The dose enhancement is relatively measured in nanocoulomb (nC). The linear accelerator Siemens Primus at 6MeV with radiation dose at 200MU with field size at 5x5 cm2 were set [4-10]. The distance from the radiation source to the center of the tooth is 80 cm. The angle of the radiation was perpendicular to the tooth axis. The dosimeter PTW UNIDOS E measured in relative dose (nanocoulomb: nC) and the Ionizing chamber Semiflex ionization chambers type 31010 with diameter 5.5 mm and 6 mm in length connects to the dosimeter PTW UNIDOS E [11, 12].
Figures 1: Electrode placement in the position 1) back-scatter side (buccal), 2) upper side (occlusal), and 3) forward-scatter side (lingual). The electrode holder (in brown color) locked the measurement position.
The mean and standard deviation (SD) were calculated. The data compared the difference of relative dose enhancement of the primary beam radiation in each location of the ionization chamber (buccal, occlusal and lingual surfaces) and compared the difference of relative dose enhancement of the primary beam radiation between the types of tooth preparation (class I, class I other, class II MOD, cusp tipping and core build-up) in the same material.
Results
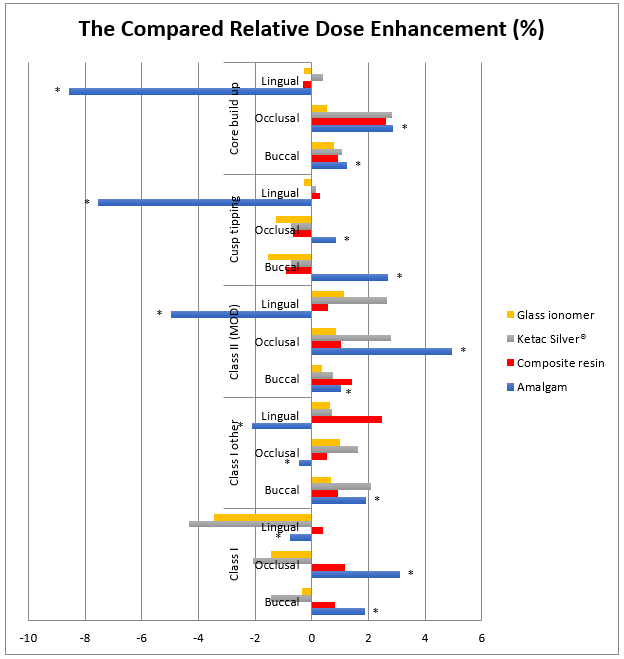
The relative dose enhancement of teeth restored with four restorative materials (amalgam, composite resin, Ketac Silver® and glass ionomer) in five tooth preparations (class I, class I other, class II MOD, cusp tipping and core build-up) is shown in (Figure 2). The ionization chamber was placed in 3 different positions (buccal, occlusal and lingual surface). The relative dose enhancement in the amalgam-filled tooth increased in the buccal and occlusal aspects, while the radiation absorption occurred on the lingual side. The relative dose enhancement on the buccal, occlusal and lingual surfaces was increased in the buccal aspect of the amalgam filled tooth by the maximum dose presented at cusp tipping, followed by class I other and class I, core build-up and class II MOD. At the occlusal aspect, the relative dose enhancement was the largest in class II MOD, followed by class I, core build-up, and cusp tipping. The most radiation scatter happened in the class II MOD group. Meanwhile, the radiation absorption occurred in class I other filling tooth. In the lingual aspect, every type of tooth preparation demonstrated signs of radiation absorption, the highest in core build-up, followed by cusp tipping, class II MOD, class I other and class I.
Figures 2: The compared relative dose enhancement (%) in every tooth preparation and restorative material (* statistically significant difference).
In composite resin filled tooth, the relative dose enhancement increased as measured at the buccal and occlusal aspects in class I, class I other, class II MOD and core buildup group and decreased in the cusp tipping group. At the lingual aspect, the relative dose enhancement increased in every tooth preparation except in core buildup group, where it declined. In Ketac Silver® filling tooth, the relative dose enhancement increased as measured at the buccal and occlusal aspects in class I other, class II MOD and core buildup group and decreased in class I and cusp tipping group. At the lingual aspect, the relative dose enhancement increased in every tooth preparation except in class I group, where it declined. In glass ionomer filling tooth, the relative dose enhancement increased in the buccal and occlusal aspect in class I other, class II MOD and core buildup group whereas it decreased in class I and cusp tipping group. At the lingual aspect, the relative dose enhancement increased in class I other and class II MOD unlike in class I, cusp tipping and core buildup group where it decreased.
Discussion
In this study, the highest relative dose enhancement occurred at the buccal aspect of cusp tipping amalgam filled tooth at 2.7% due to the wide contact point of amalgam surface. The result was similar to Chin DW et al. who measured the backscatter dose in tooth restored with amalgam on the buccal surface at 2%. In the lingual aspect, every type of preparation of amalgam filled tooth demonstrated lower relative dose enhancement as an effect of attenuation by the high-density, high atomic-number absorbing material in amalgam composition such as silver, tin and copper [13]. Farahani et al. and Thilmann et al. showed that a higher atomic number material has higher radiation scatter and attenuation [1, 14]. In the occlusal aspect, the radiation absorption occurred in class I other filling as there was no restorative material at this side. Slightly higher backscatter radiation occurred at the occlusal than the buccal aspect except in class I other and cusp tipping type. The MOD preparation had the highest backscatter radiation dose as a consequence of the large restorative material surface on the occlusal side. In class I and core buildup, there was no statistically significant difference of the backscatter radiation even though there was slight difference in the exposed restorative material surface. Low relative dose enhancement occurred in cusp tipping (which has larger amount of restorative material than MOD type) maybe due to the tooth anatomy limitation by deep occlusal grooves, steep inclined planes and also the size of radiation probe which caused the difficulty in probe positioning. The probe was slightly away from the tooth interface, which might lead to the lower relative dose enhancement. The lowest relative dose enhancement occurred in class I other that has no restorative material at this side. Ketac Silver®, containing silver and titanium dioxide that might cause higher relative dose enhancement at the buccal and occlusal aspecst than the glass ionomer and composite resin which does not have any metal components. In this study, we did not find any statistically significant differences between Ketac Silver®, Glass ionomer and composite resin.
However, in our experiment, we simulated the oral cavity condition by using water as soft tissue equivalent material and measured the relative dose enhancement with the ionizing chamber. The relative dose enhancement, when compared with its control tooth, demonstrated the higher or lower dose at the contact between different electron density materials but could not tell the actually increased radiation dose. The backscatter radiation occurred at the buccal side results in the higher dose of radiation which can affect soft tissue and cause more chance of mucositis. Chin DW et al. have found that the backscatter radiation could travel 4 mm in air and suggested using at least 2 mm shield to prevent the backscatter radiation effect, which is similar to the work of Reiteneier B et al. that recommended 3 mm stent [8, 13]. We recommend using amalgam enormous filling in the cavity and making the outer surface with glass ionomer. Because the amalgam has ability to absorb radiation the most. Nowadays, amalgam is rarely used in many countries owing to mercury toxicity. On the other side, amalgam can absorb some ray and may help the mucositis in head and neck radiation cases. Moreover, the large or small glass ionomer presented a good absorbing tendency. Therefore, the outer glass ionomer filled should be suggested to cover the cavity and its capability to release fluoride should be embraced. As radiation therapy usually caused lower saliva production and was followed by radiation caries, this technique is our recommendation [7]. Also, the radiation measurement tools to use for further study is the thermoluminescence dosimeters (TLD) or others that are able to measure actual enhanced radiation dose and very precisely to achieve the higher accurate radiation dose and result.
Acknowledgement
Authors would like to acknowledge Faculty of Dentistry, Thammasat University to support this study and acknowledge gratefully the Radiology department, Bhumibol Adulyadej hospital, and Physicist Mr. Paisarn Suwannakorn, for providing the laboratory and instruments.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 15, Apr 2020Accepted: Fri 01, May 2020
Published: Mon 11, May 2020
Copyright
© 2023 Kuson Tuntiwong. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.02.05
Author Info
Corresponding Author
Kuson TuntiwongDepartment of Orthodontics, Faculty of Dentistry, Western University, Pathum Thani, Thailand
Figures & Tables
References
- Thilmann C, Adamietz IA, Ramm U, Rahn R, Mose S et al. (1996) In vivo dose increase in the presence of dental alloys during 60Co-gamma-ray therapy of the oral cavity. Med Dosim 21: 149-154. [Crossref]
- Fuller CD, Diaz I, Cavanaugh SX, Eng TY (2004) In vivo dose perturbation effects of metallic dental alloys during head and neck irradiation with intensity modulated radiation therapy. Oral Oncol 40: 645-648. [Crossref]
- Hassan K, Khier S (1997) Effect of Therapeutic Gamma Radiation on Dimetral Tensile Strength and Microhardness of Photo-cured Glass Ionomer Cements. SDJ 9: 120-124.
- Carvalho FG, Fucio SB, Pascon FM, Kantovitz KR, Correr Sobrinho L et al. (2009) Effect of gamma irradiation on fluoride release and antimicrobial activity of resin dental materials. Braz Dent J 20: 122-126. [Crossref]
- Cruz AD, Cogo K, Bergamaschi Cde C, Boscolo FN, Groppo FC et al. (2010) Oral streptococci growth on aging and non-aging esthetic restorations after radiotherapy. Braz Dent J 21: 346-350. [Crossref]
- vonFraunhofer JA, Curtis P Jr, Sharma S, Farman AG (1989) The effect of gamma radiation on the properties of composite restorative resins. J Dent 17: 177-183. [Crossref]
- De Moor RJ, Stassen IG, van 't Veldt Y, Torbeyns D, Hommez GM (2011) Two-year clinical performance of glass ionomer and resin composite restorations in xerostomic head- and neck-irradiated cancer patients. Clin Oral Investig 15: 31-38. [Crossref]
- Reitrmeier B, Reitrmeier G, Schmidt A, Schaal W, Blochberger P et al. (2002) Evaluation of a device for attenuation of electron release from dental restorations in a therapeutic field. J Prosthet Dent 87: 323-327. [Crossref]
- Beyzadeoglu M, Dirican B, Oysul K, Ozen J, Ucok O (2006) Evaluation of scatter dose of dental titanium implants exposed to photon beams of different energies and irradiation angles in head and neck radiotherapy. Dentomaxillofac Radiol 35: 14-17. [Crossref]
- Spiridovich S, Papiez L, Langer M, Sandison G, Thai V (2006) High density dental materials and radiotherapy planning: Comparision of the dose predictions using superposition algorithm and fluence map Monte Carlo method with radiochromic film measurements. Radiother Oncol 81: 309-314. [Crossref]
- Prasad SG, Parthasaradhi K, Bloomer WD, Al Najjar WH, McMahon J et al. (1998) Aluminum, copper tin and lead as shielding materials in the treatment of cancer with high-energy electrons. Radiat Phys Chem 53: 361-366.
- Webster GJ, Hardy MJ, Rowbottom CG, Mackay RI (2008) Design and implementation of a head-and –neck phantom for system audit and verification of intensity-modulated radiation therapy. J Appl Clin Med Phys 9: 2740. [Crossref]
- Chin DW, Treister N, Friedland B, Cormack RA, Tishler RB et al. (2009) Effect of dental restorations and prostheses on radiotherapy dose distribution: a Monte Carlo study. J Appl Clin Med Phys 10: 2853. [Crossref]
- Farahani M, Eichmiller FC, McLaughlin WL (1990) Measurement of absorbed doses near metal and dental material interfaces irradiated by x- and gamma-ray therapy beams. Phys Med Biol 35: 369-385. [Crossref]
