Journals
Comparative analysis between bone-guided (endo-exo) prostheses and soft-tissue guided shaft prostheses for rehabilitation after thigh amputation, with special emphasis on its socio-economic aspects
A B S T R A C T
Background: A prompt and effective rehabilitation after a thigh amputation has significant advantages in terms of the functional and psychological acceptance of the prosthetic restoration. As at now the rehabilitation after thigh amputation is carried mainly by soft tissue guided shaft prostheses. Over the years, various authors reported on a variety of problems with shaft prosthetics. In Sweden, for example, an alternative procedure was developed based on dental implantology in the 1990s, in which the transmission of thigh stump to exo-prosthesis takes place by means of an intramedullary, percutaneously guided implant (OPRA procedure). OPRA stands for "Osseointegrated Prosthesis for the Rehabilitation of Amputees". This special procedure involving two surgical steps was first performed in 1999 in Lübeck. There are now more than 200 patients worldwide with Endo-exo-femoral prosthetics.
Methods/Design: During a period of 14 years (1999-2013), 75 patients were treated with the endo-exo-femoral prosthesis in the Sana Clinic Lübeck. Patients were included in the study who had the endo-exo-femoral prosthesics for at least 12 months and who reliably had regular check-ups. Based on this, a random sample of a total of twenty-one (21) patients treated with the endo-exo-femoral prosthesis between 1999 and 2012 was obtained. Since a total of nineteen of the twenty-one patients had experience with soft tissue guided shaft prostheses, we took the opportunity to ask them about their subjective experience with the prosthetics. For this purpose, a questionnaire was drawn up with 49 very extensive questions. The content of the questions relates to endo-exo prostheses and soft tissue guided shaft prostheses, family, socio-economic, quality of life and patient satisfaction.
Conclusion: Based on this analysis, the Integral Leg Prosthesis (ILP) is of great benefit in the health and socio-economic aspects of rehabilitation.
K E Y W O R D S
Osseointegration, Integral Leg Prosthesis (ILP), Endo-Exo-Femurprosthesis (EEFP)
Background
A prompt and effective rehabilitation after a thigh amputation has significant advantages in terms of the functional and psychological acceptance of the prosthetic restoration [1]. As at now the rehabilitation after thigh amputation is carried out mainly by soft tissue guided shaft prostheses. Over the years, various authors [14, 19] reported on a variety of problems with shaft prosthetics. In Sweden, for example, an alternative procedure was developed based on dental implantology [5] in the 1990s, in which the transmission of thigh stump to exo-prosthesis takes place by means of an intramedullary, percutaneously guided implant (OPRA procedure) [6]. OPRA stands for "Osseointegrated Prosthesis for the Rehabilitation of Amputees". The term osseointegration was coined by Branemark and Albrekktsson [26]. Endo-Exo-femoral prosthetics is a similar procedure in which recovery of walking ability occurs in a similar way by osseointegrated force carriers, to which the Exoprosthetic can be easily docked [2]. This special procedure involving two surgical steps was first performed in 1999 in Lübeck [9]. There are now more than 200 patients worldwide with Endo-exo-femoral prosthetics. Although the first successful results with bone-guided implants (tooth implantology) were only achieved in humans in the 70's and 80's, literature tell us that similar attempts had already been made as far as 65 years ago. During and after the Second World War, the Americans and Germans independently undertook experiments with bone-guided lower leg prostheses. Since then, further attempts followed. The breakthrough came in 1990 with BRÄNEMARK R, who for the first time supplied a femoral amputee with a threaded, screwed intraosseous anchored and two-time percutaneously delivered femoral implant [4].
In 1999, the first restoration of a thigh amputee with an endo-exo-femoral prosthesis in Lübeck was performed [9]. By December 2014, 86 patients in Lübeck had been treated with the endo-exo-femoral prosthesis. The standardized procedure in two operating steps has been the subject of the procedure catalog since 2008 (Systematic List of Surgery and Procedure Keys - International Classification of Procedures in Medicine) [12]. The two operation steps can be found under the numbers:
5-828.0 Implantation of a partial bone replacement.
5-869.3 Inserting a connector for an endo-exo-prosthesis.
A surgical stabilization of the FC was indicated, and a minimally invasive approach was preferred, and the informed consent taken. As first step, sternal fixation was performed with a titanium plate (DePuy Synthes, Johnson&Johnson, Raynham, Massachusetts, US) and a Nuss bar (Pectus Support Bar System; PTY Medical Device, Shanghai, China) was then placed with video assisted thoracoscopic support to stabilize the bilateral rib fractures: two 4 cm incisions were performed bilaterally, along the fifth intercostal space. A pre-shaped still bar was passed into the pleural space under thoracoscopic monitoring. The bar was then rotated and fixed to the lateral arch of the fifth ribs with metallic sutures (Figure 2). Surgical time was 120 minutes with minimal blood loss. The patient was extubated 4 days later and recovered well. Written informed consent was obtained.
Discussion
FC is a serious condition with high mortality rate [1-3]. It leads to hypoventilation and ineffective coughing, increasing exponentially the risk of complications. Recently, several studies have shown that surgical stabilization decreases ICU stay, mortality, pulmonary complications, long term chest deformity and, ultimately costs [1-3]. Several methods and materials are available in order to choose the best surgical approach: locked plates, rib-clamp systems and intramedullary K-wires are the most commonly employed [2]. However, all of them require direct access to the fractured ribs, and when bilateral fractures occur, long or multiple incisions are needed [3]. In our case various conditions affected the surgical strategy.
Figure 1: Model of an endo-exo-prosthesis (Dr. Aschoff, Lübeck).
Since 2006, the procedure of the Endo-Exo-prosthesis belongs to the "New examination and treatment methods (NUB)". The Sana Klinik Lübeck applied for the NUB for the Endo-Exo-procedure in 2006 for the first time and renewed the approval for it every year. It thus has an outstanding unique selling point throughout Germany.
Problems of conventional soft-tissue guided prostheses after thigh amputation
Conventional prostheses are soft tissue-guided shaft prostheses used for the rehabilitation of thigh amputees. The prosthetic shafts are fixed by static friction or a vacuum system on the thigh stump. Then the coupling of the knee lower leg prosthesic system takes place on the prosthetic shaft. The prosthetic shafts thus serve as a connection between the stump and the prosthesis. The static friction and the negative pressure system can cause discomfort on the stump as well as in the pelvic and lumbar area. Changes in the stump volume, whether daily or in case of weight often-used rigid shaft. Sweating often leads to the loss of static friction and thus to the loss of the prosthetic seat. The prostheses are generally held about 1 to 2 cm shorter than the healthy leg in order to allow a better swinging of the prosthetic leg. This circumstance leads to static deviations in the frontal and sagittal plane. It compensatorily leads to hyperlordosis through the pelvic tilting forward [10]. Over time, the lack of movement due to amputation, pain and muscle contractures, leads to a reduction of mobility in the affected hip joint [21, 22]. Furthermore, the prosthetic shaft leads to other complaints / difficulties such as: Pressure points, Pain, Irritations / -Ulcers, Abscesses, Fixation problems (due to daily volume fluctuations), Sweating, Swelling, Congestion, Intolerance of the prosthesis stem, Need for surgery BRINCKMANN, 2002 also cited the concept of zero tolerance in his work on the biomechanical aspects of the skin, cited also by Pauls E. 2010 [10]. "If the compressive stress remains within the tolerance limits with regard to how much and duration, then all vessels open after pressure has been applied and swelling occurs. If the required recovery time is not guaranteed until the next compressive stress, the tolerance limits for the second stress are reduced. If recovery times are too short, repeated compressive stress can lead to zero tolerance [13]. This factor is also evident in patients with poorly adapted orthoses, splints and shoes. In most cases, they do not use them after a short wearing period. "If there is a significant increase in stump volume, there is an additional increase in shear forces, which have a negative impact on the stump. The friction can lead to skin redness, chronic ulcers and to abscesses.
These complaints and problems have led, for decades now, to considerations for the realization of bone-guided prosthetics. This idea has been developed by numerous experiments on animals and humans since World War II. As a result, various bone-guided, percutaneously delivered implants from various working groups from Sweden, Holland, Australia and Germany can be found today. BRANEMARK R. in 1990 was the first to have permanently and successfully tested such an implant on humans. In 1999, GRUNDEI presented in Lübeck a significantly modified implant in philosophy and design, which was used for the first time in the same year and has since been used in everyday clinical practice. However, several other design changes have been required and implemented, especially in the area of skin-penetrating components [9, 1].
Indication and Contraindications to the endo-exo-femoral prosthesis
Patients who receive the endo-exo-femoral prosthesis are those amputated due to trauma, tumor and infection-related. This includes those in which a satisfactory rehabilitation using shaft prostheses is limited or not possible, or in which the use of the shaft prosthesis cannot be guaranteed due to a too short amputation stump. Excluded are patients with the following comorbidities or criteria [25, 25]: Diabetes mellitus, Arterial circulatory disorders, Mental illness, Continuous medication with chemotherapy or cortisone, Disability, Pregnancy / Breastfeeding, Unfinished skeletal growth, Lack of compliance, Prisoners.
Surgical Technique
The supply of the endo-exo-femoral prosthesis takes place at two levels. In the first step, the actual implant (endomodule) is first introduced into the bone tube. In the second step, after about 6 weeks, a stoma is created on the distal amputation stump and the components passing through the skin are mounted.
Step 1: Implantation of a partial bone replacement.
Via a lateral access, the distal femoral shaft is exposed. The selection of the endo-module depends on the shaft diameter. Then the implant is inserted into the femur and the soft tissue is closed [2, 15].
Figure 2 a-e: Implantation of a bone substitute (Step 1: Dr Aschoff, Lübeck).
Step 2: Inserting a connector for the endo-exo-prosthesis.Generally six weeks after the first operation, the second step is performed by inserting a connector to which the Exo prosthesis together with an artificial knee joint can be connected [2, 15].
Figure 3 a-d: Inserting a connector (Step 2: Dr. Aschoff, Lübeck).
Figure 4: Patient with a complete endo-exo-femoral prosthesis (Dr. Aschoff, Lübeck).
For the detailed procedure on the surgical technique and for the preoperative planning I refer to the work of Pauls E. on the operative results and the quality of life after treatment with an endo-exo-femoral prosthesis, 2010 [10] and Aschoff HH et al. 2011 [15].
Study objectives
Even today, compared to the attempt of limb maintenance, amputation frequently leads to a shortening of the treatment time with expected functioning and resilient prosthesis supply and the resulting rapid return to the familiar environment, work and social environment [3]. A study conducted in Sweden on material and treatment costs suggests that the OPRA procedure (OPRA: Osseointegrated Prosthesis for the Rehabilitation of Amputees) is an alternative to the shaft prosthesis from a health economics point of view over the five-year period [7, 8].
Both material and treatment costs are not transferable to the Endo-Exo-process and the circumstances in Germany. A comparative analysis of the benefits and costs of the endo-exo patients treated in Lübeck will shed light on the economic impact of rehabilitation and reintegration into working and social life. The majority of patients examined were very young at the time of the amputation with a median of 27 years. The relatively young age of these patients is due to the fact that the amputations were mainly because by trauma. This results in a relatively long-life expectancy with correspondingly high demands on mobility and thus an adequate rehabilitation.
In order to assess these conditions, we developed and administered a questionnaire that took into consideration the individual aspects of the problem with the respective prostheses, such as: Duration of wear and comfort, use in everyday life and satisfaction with the respective prosthesis supply queries. All patients received the same questionnaire and had to select the appropriate answers, after which the questionnaires were analyzed. The data analysis focused on: gender distribution, age distribution, cause of amputation, number of prostheses already used, adjustments made per prosthesis, duration of rehabilitation, maximum wearing time without interruption, maximum running distance with or without walking aid, falls with the respective prosthesis, prosthesis as an obstacle in everyday life, sports / leisure, assessment of the current standard of living, cost estimation per prosthetic.
A detailed cost estimate for both the shaft prosthetics and for an endo-exo-femur prosthetic restoration is presented in the appendix on the basis of data from the Federal Guild for Orthopedic Technology for the shaft prosthesis and data from the Sana Clinic Lübeck.
Sample
From 1999 to December 2013, 75 patients were treated with the endo-exo-femoral prosthesis in the Sana Clinic Lübeck. Patients were included in the study who had the endo-exo-femoral prosthesis for at least 12 months and who were reliably provided for the regular check-ups. From the bottom of this criteria, a random sample of a total of twenty-one (21) patients treated with the endo-exo-femoral prosthesis between 1999 and 2012 was obtained. The sample consist of five women and sixteen men. One patient underwent a bilateral thigh amputation, all other patients were unilaterally amputated. Since a total of nineteen of the twenty-one patients had experience with shaft prostheses, we took the opportunity to question them about their subjective experience with the shaft prosthetics. For this purpose, a questionnaire was drawn up with 49 very extensive questions (see Appendix). The content of the questions relates to endo-exo prostheses and shaft prostheses, family, socio-economic, quality of life and patient satisfaction. The costs for the treatment with the Endo-Exo-prosthesis were taken from the data of the Sana Klinik in Lübeck. We received the cost data of the shaft prosthesis from the company "Orthopädie Technik Bauche GmbH” in Germany.
Table 1: Exemplary cost estimate for the provision of a shaft prosthesis within one year
For patient 1: (2009-2010)
|
Cost (gross)/Euros |
|
|
Elastic plaster bandages |
16,79 |
|
Cellona plaster bandages |
150,14 |
|
Thermolyn, stiff |
104,34 |
|
Clutch Lock |
299,30 |
|
ICECROSS Transfemoral standard |
837,72 |
|
Perlon pull-on stocking |
17,82 |
|
Cotton stump sock |
15,96 |
|
Thigh shaft made of cast resin |
1483,11 |
|
Knee mounting |
8,88 |
|
Flexible stem for thigh prosthesis |
373,95 |
|
Clutch-lock |
332,87 |
|
Icecross transfemoral Standard |
931,67 |
|
Mounting Adapter |
17,75 |
|
Working hours |
1653,83 |
|
Stockings |
78,88 |
|
Repair on shaft |
373,95 |
|
Working hours |
145,32 |
|
Stockings |
46,30 |
|
Medi RELAX Night care |
197,42 |
|
Dressinghelp |
64,95 |
|
Shank in clasp technology |
1790,61 |
|
Foam Form + connection cap |
473,17 |
|
Knee mounting |
7,98 |
|
Stockings |
46,30 |
|
Final sum |
9469,01 |
Table 2: Exemplary cost estimate for the provision of a shaft prosthesis within one year
Patient 2 (2008-2009)
|
Cost(gross)/Euros |
|
|
Plaster negative |
171,20 |
|
Schaft |
1600,00 |
|
Fitting |
149,80 |
|
Connection Adapter |
37,45 |
|
lamination anchor |
116,63 |
|
Hospital care |
25,64 |
|
Stem narrowing |
119,00 |
|
Hospital care |
28,51 |
|
Butt pads |
35,70 |
|
Final sum |
2283,93 |
Results and Discussion
The gender distribution shows a significant dominance of the male sex. Of twenty-one patients, sixteen were male (76.2%) and five were female (23.8%). A similar distribution can also be found in the literature [7, 14]. The average age at the time of amputation was 30.8 years for our patients. This is almost as high as other references. At the time of implantation, the average age from other literature was 45.8 years. [2, 3, 14]. Regarding the causes of the amputation of the patients in question, 81% were amputated because of trauma. The remaining 19% required amputation because of a tumor. Similar data can be found in related literature, in which states that patients are mainly amputated due to an accident [7, 14, 15]. The high number of male patients is also reflected in the results of other studies [3, 7, 14]. For the high male ratio, it is to be assumed that men are more likely to engage in physical labor than women and men are more likely to overestimate themselves. The same author continued to report that education plays an important role, namely that people with low educational attainment have both a higher risk of accidents at work and on the road [3].
Table 3: Exemplary cost statement for the supply of an EEFP within one year.
Patient 3
|
Cost (gross)/Euros |
|
|
Step 1 |
4317,54 |
|
Step 2 |
4317,54 |
|
Reimbursement implant by the health insurance company to hospital |
4200 |
|
Knee connection adapter |
1259,50 |
|
Allen key |
27,85 |
|
Extension module |
1046,72 |
|
Working hours |
453,99 |
|
Torsionsadaptation |
474,10 |
|
Working hours |
162,14 |
|
Final sum |
16259,38 |
Table 4: Exemplary cost statement for the supply of an EEFP within one year.
Patient 4
|
Service and Material |
Cost (gross)/Euros |
|
Step 1 DRG 1.542 |
4806,97 |
|
Step 2 DRG 1.385 |
4317,54 |
|
Hospitalisation because of stoma complaints DRG 1.163 |
3625,49 |
|
Reimbursement implant by the health insurance company to hospital |
4200,00 |
|
Extension module |
1046,72 |
|
Knee connection adapter |
1259,50 |
|
Allen key |
27,85 |
|
Working hours |
713,41 |
|
Final sum |
19997,48 |
Considering the number of required changes with the shaft prosthetic and compared to the number of necessary revisions or corrections on the endo-exo-modules, it is noticeable that the majority of patients with shaft prostheses needed changes several times. Considering the number of adjustments made to both types of prostheses, it becomes even clearer that the patients in our study had significantly more problems with the shaft prostheses as compared to the endo-exo-femoral prostheses. The reasons for the high number of changes made on the shaft prostheses were pressure points, irritation / ulcers, abscesses, fixation problems, technical problems till even the need for surgery for a soft tissue adaptation.
RACK A. describes in her dissertation that the orthopedic mechanic can only provide a patient with a good and functional prosthesis [3] if the surgeon forms a good stump. DILLINGHAM TR et al. (2001) report in their study that despite a wearing period of about 80 hours per week, which means a relatively high use of the shaft prosthesis, only 43% of the patients were satisfied with their prostheses. 25% of the patients had complaints such as irritation, wound and phantom pain [16]. Furthermore, DILLINGHAM reported that patients received a new shaft prosthesis almost every other year. This fact is reflected in our study. There was a comparatively high need for shaft corrections or readjustments, which were mostly based on an unsatisfactory suiting of the prosthetics. In a study by HAGBERG K and BRÄNEMARK (2001) similar problems with the shaft prosthesis are reported. The main concerns of the interviewed patients were sweating, ulcers, skin irritation, unsatisfactory suiting of the femoral stump, and the resulting inability to walk ergonomically or quickly. Nearly 50% of their patients also complained of stump phantom pain, back pain, and contralateral leg pain [14]. NICHOLAS (1993) made comparable statements on this problem [19].
The principle of the intramedullary percutaneously drained endo-exo-prosthesis avoids these problems completely and offers significant benefits in terms of walking safety, energy consumption and comfort by the direct transmission of forces from the skeleton to the Exo-prosthetics. However, special attention must be paid to the skin penetration site of the components of the implant. Initially the penetration site showed irritations with erythema, swelling, hypergranulation and pain, which either had to be treated conservatively or frequently had to be treated surgically. CLAUSEN A. (2007) showed in their work on the endo-exo-femoral prosthesis that bacterial cultures are detectable in every patient in the area of the stoma. However, these cultures were merely a colonization of the soft tissue channel by a local flora, which does not necessarily lead to infections and thus does not necessarily develop a disease value [11].
However, these stoma irritations necessitated various design changes of the skin pernetrating components. These changes affected both the circumference and the quality of the surface of the components; with the introduction of the double cone used since 2009, undesired surgical measures at the skin penetration site have become unnecessary [2, 11, 53]. When comparing the absolute number of required visits to the orthopedic technician, the group of endo-exo patients shows a marked reduction in these visits compared to the number of visits of the femoral shaft prosthetic wearers during the same period. Because of the above problems, the shaft prosthetic wearers often had to make adjustments to their shafts. Even slight variations in the weight of the patients led to high incidence to fit inaccuracies of the sleeve, which made a visit to the orthopedic technician necessary. Even daily fluctuations in the stump volume caused the patient fixation problems of the shaft. This problem is completely eliminated in the case of bone-guided, percutaneously guided prosthetics [10].
HAGGSTROM EE et al. (2013) show in a study on the first 100 patients with osseointegrated, percutaneously-guided prosthetics in Gothenburg / Sweden that visits to the orthopedic technician were significantly less frequently required for these patients than for shaft prosthesis wearers. Patients with stem prostheses visited the orthopedic technician 7.2 times a year, and the patients treated with bone graft only 3.1 times [7]. This results in the same results in the Swedish and Lübeck patients. The uninterrupted wearing period shaft prosthesis was in the vast majority of patients (14), less than twelve hours. Only five patients were able to wear the prosthesis for fourteen hours without interruption. For the Endo-Exo prosthetic, seventeen patients can wear their prosthesis for over fourteen hours. The remaining four wore theirs for less than fourteen hours. Here is a significant increase in wearing time with the Endo-Exo-prosthesis. When looking at the difference in maximum distance covered between the two types of prostheses, the positive development in terms of walking ability and walking distance is impressive. The number of patients who can walk for any length of time has risen by about 32.8% after being supplied with the integral-leg-prosthesis. The vast majority of patients with shaft prosthesis recorded the highest number falls (two to five) during the total time of each shaft supply. There is a drastic decrease in the number of falls with the Endo-Exo-femoral prosthetic. Whether all the falls were actually due to specific features of the shaft prosthetics, could not clearly answer the patient. However, it is reasonable to assume that at least a partial liability can be found here. Bruises, ligament tears and overstretching, abrasions and muscle strain were the results of the falls. Although the patients did not suffer serious injuries due to the falls with both the shaft prosthesis and the osseointegration, a significant decrease in the tendency to fall is, of course, per se desirable. A significant difference can also be found when it concerns the extent at which patients feel disabled by the shaft prosthesis or the endo-exo-femoral prosthesis in sports , leisure activities in everyday life and whether they are coping with everyday obstacles, in this case climbing stairs and if so - with what effort. 76.2% of the patients said they felt hindered by the shaft prosthesis when exercising sports and in leisure time. Only 9.5% of patients in the endo-exo group made this statement. When climbing stairs, the number of patients who can do this with no efforts doubled, and so there was an overall significant improvement in climbing stairs with the endo-exo-femoral prosthesis.
LEGRO et al. reported as early as 1999 that comfort when standing or sitting is very important in the provision of a prosthesis [28]. His findings show that shaft prosthesis leads to significant limitations in terms of mobility and comfort. This fact is also confirmed by HAGBERG, PERRY and JOHNSTON. An adequate mobility in the hip joint is necessary for an adequate coping with everyday life [18]. In 1970, JOHNSTON and SMIDT concluded that a flexion of at least 120 °, an abduction of 20 ° and an external rotation of 20 ° in the hip joint are needed for adequate coping with everyday life [20]. In order to enable a course with normal increment, the human needs an adequate extension radius in the hip joint. A femoral amputation compromises muscular balance, mobility, and muscle strength in the hip joint of the affected side [21, 22]. Due to immobility and pain and loss of muscle mass after amputation, the risk of developing a hip muscle contraction increases [23]. The risk of developing a contracture is highest in hip flexors, and the shorter the stump, the more likely patients will develop a contracture of abductors and external rotators [18]. If a contracture develops, there will inevitably be difficulties in adapting the prosthesis and consecutive problems during walking [30]. A research question from HAGBERG et al (2005) [18] deals with this question.
HAGBERG K et al. investigated in their study from 2005 the alternative forms of treatment after thigh amputation with respect to the mobility of the affected hip joint and the respective comfort of both types of prostheses. As a result, 44% of patients with shaft prosthesis but only 5% of patients with the intramedullary implant complained of moderate sitting discomfort. The analysis of hip mobility revealed that patients with endo-exo-femoral prostheses have a largely normal flexion (112 ° -129 °) in the affected hip joint. None of the patients with shaft prosthesis reached nearly such values. The reasons for the difficulties with sitting with the shaft were mainly the limited flexion, the lack of rotation and pressure points on the stump due to the shaft. Because of these difficulties with the stem prosthesis, patients with a fitted endo-exo-femoral prosthesis can therefore sit better [18]. The walk of femoral amputees with shaft prosthesis is always asymmetrical. The running speed of the amputees is lower than that of non-amputees and correlates in the same direction with the range of motion in terms of extension flexion in the hip joint on the affected side. The energy expenditure of the amputees in walking is higher than that of non-amputees and seems to be related to the length of the residual stump and the possible extent of abduction and adduction of the hip joint on the affected side [17, 33, 34].
In a comparative gait analysis of thigh amputee patients with shaft prosthesis and patients with the endo-exo-femoral prosthesis versus healthy volunteers, the data showed that the gait safety and the gait symmetry in carriers of the endo-exo-femoral prosthesis hardly differ from those of the healthy. The energy consumption when running certain distances in a certain time can be significantly reduced by osseointegration compared to the shaft prosthesis [33]. WATERS et al. (1976), HAUNG et al. (1979), JAEGERS et al (1993) and other authors have described that running with the shaft prosthesis leads to an increase in energy expenditure and a reduction in running speed [29, 30, 31]. The relatively young age of the examined patients at the time of the amputation calls for effective rehabilitation in order to enable the affected patients to participate in professional and social life as fully as possible. In the US, according to a study by ANDREW et al (2010), it is recommended a running distance of at least 600m should be ensured during rehabilitation so that patients can meet their everyday needs [32].Amputees have limited functionality. The ability to walk is closely linked to the quality of life and everyday life. The amputees have a limited ability to walk and the walking distance decreases.
According to a study by PERNOT (2000) in Limburg, of the 43 patients treated with shaft prosthesis, only 7 patients were able to walk more than 500m one year after amputation [35]. HAGGBERG K. et al. in "Consequences of Non-Vascular Trans-femoral Amputation - Survey of Quality of Life, Prosthetic Use and Problems 2002" reported on the walking distance of patients with stem prosthesis in a period of three months. They found that 85% of patients were 50m, 63% 200m, 35% 500m and 14% over 2km on several days a week. Only about 35% of the patients in this survey achieved those of ANDREW A. W. et al. (2010), recommended running distance of 600m [14]. The references cited above confirm the results of my study. Patients treated with shaft prostheses have a significantly better walking ability, improved harmony and improved walking safety compared to endo-exo-femur-prosthetically treated patients with significantly extended individually possible walking distance.
An important issue in this work is the time needed to resume occupation. The rehabilitation of a thigh amputee should be quick and effective so that the time to resume the occupation can be kept as short as possible. The duration of hospital stays and the stay in rehabilitation facilities played an important role. The longer a job loss lasts, the more difficult it is usually to reintegrate into the work process. In this analysis, patients with the endo-exo-femoral prosthesis need fewer rehabilitation stays. Rehabilitation is not desirable for most people and is medically acceptable as they feel safer with the Endo Exo prosthesis.
SCHOPPEN T. et al (2001) showed that an average of approximately 2.3 years elapsed before patients with amputations of the lower limbs resumed work [36]. RACK A. calculated the length of stay in inpatient and rehabilitation facilities at about 9.8 - 19.9 months [3]. HAGBERG K. et al., (2005), speak of a rehabilitation period of 4 to 6 months with the osseointegration in femoral amputees [37]. Here it must be mentioned that HAGBERG K. usually waits 3 to 6 months after implantation of the endomodule until the second step. For this reason, there is an extended rehabilitation period. Further arguments for this tendency come from the patient's point of view. Many patients enthusiastically report better comfort, improved proprioception, and a significant decrease in walking effort. Patients even refer to osseointegration as a 'revolution', a 'practical prosthesis', a 'delusional limb', and even as a 'part of me' [39]. Patients also report improved feel and control with the Endo-Exo prosthesis, and can now use it to identify what kind of floor they are walking or standing on (for example, on asphalt, gravel or grass). One patient reported after 3 years with the endo-exo-femoral prosthesis that she felt that her phantomlimb was slowly regrown [38]. The phenomenon of improved tactile threshold identification by means of the bone guided prosthesis is referred to as osseoperception and was first described in dental implantology. The ability of so-called tactile threshold detection is ensured by mechanoreceptors of the joints, the skin, the mucous membrane, the bone and the musculature [38, 40-44].
The above circumstances allow patients to better manage the Endo Exo prosthesis than the shaft prosthesis. Other significant factors involved include work reintegration: age at the time of amputation, level of education and wearing comfort of the prosthesis [45]. Elderly patients with a low level of education and problems wearing the shaft prosthesis have a harder time relocating. As unemployment in and of itself leads to further comorbidities, it is very important that it is kept as low as possible.
The following literature reviews refer to patients treated with shaft prostheses after amputation. DASGUPTA et al. (1997) found in a study of trauma-induced trans-tibial amputee amputees that out of 27 patients who were able to work, only 16 (59%) returned to work after amputation [46]. MILLSTEIN et al. (1985), had a value of 87% in lower extremity amputations. However, their study involved patients who had suffered trauma at work and were given the opportunity to continue working after the amputation [47]. In a study by FISHER K. et al. (2003), in which 64% of patients were amputated traumatically, 66% of patients worked after amputation [48]. In the same study, FISHER K. et al. Of 25 patients who complained of a decrease in performance at work, 12 (48%) had problems with the shaft prosthesis. 34% were unemployed and in 62% of the unemployed, the reason was the amputation or problems with the shaft prosthesis. In a study by WHYTE A.S. et al., 2001, where 47% of patients were amputated due to trauma, returned to work only 43.5% of 75% of the patients who had worked prior to amputation [49]. In this study, out of twenty-one patients, twelve (57.1%) were employed and nine (42.9%) retired. Of the twelve working patients, only two (16.7) were still in the first job. Ten (83.3%) had changed jobs. These data are very similar to those in the work of several other authors [46, 48, 49].
As mentioned above, 19 patients in this study before the EEFP had worn shaft prostheses. Some were already covered in time with the stem prosthesis. Therefore, the comparison of reintegration with the shaft prosthesis with that of an endo-exo-femoral prosthesis is not very representative. This work should serve as a suggestion to carry out further studies to investigate the reintegration conditions in patients who were primarily treated with the Endo Exo prosthesis. If you compare the costs for Pateint 1 and 2 you notice a big discrepancy in the sums (see appendix) If we look at the tables we immediately realize that Patient 1 had a lot to deal with repairs compared to Patient 2.
In Patient 3 and 4 the small difference is due to an additional co-morbidity in Pateint 4.
At first sight, the provision of the shaft prosthesis seems to be much more economical. However, if one extrapolates the data that has been collected over a longer period of time, comparable costs result. This suggests that patients with shaft prostheses more often have problems that we have already mentioned above, and therefore need more often to the technician or even get a new prosthesis. HAGGSTROM, HANSSON et al. (2013) showed in their study that the costs incurred in the treatment with both the endo-exo-femoral prosthesis and the conventional shaft prosthesis over a period of about 10 years are comparable [52]. As experience with the EEFP increased, many details were improved on the design of the prosthesis and on the surgical procedure. For these reasons, no revisions have taken place since 2011 at the Sana Clinic in Lübeck following the implantation of an EEFP (ILP) 53. SMITH DG et al (1995) found that costs between $ 6,203 to $ 20,070 arise within 5 years for the restoration and adjustments to a shaft prosthesis [54].
Considering these fact we can surmise that within a period of 10 years the ILP will cost less.
Summary
Due to the relatively young age of the patients at the time of amputation, a prosthetic restoration is to be ensured which offers high mobility, high resilience and a high degree of wearing comfort. The most compromised area after limb amputation is the socioeconomic area of the patient. The aim of this study is to compare both the satisfaction in the private and social life as well as the economic aspects with those, which one finds in the supply of a shaft prosthesis. The EEFP also known as ILP (Integral_leg-Prothesis), represents an alternative to the care after thigh amputations by means of osseointegration. The study has shown in many ways that the patients are more satisfied with the EEFP than with the stem prosthesis on the basis of the questionnaires. Bearers of shaft prostheses must regularly expect, as demonstrated in the analysis, to make visits to the orthopedic technician. The number of visits to the orthopedic technician could be drastically reduced by the EEFP. Problems such as bruises, irritations, adjustments in weight changes or even new productions u.s.w. occurred with the supply by Endo Exo prosthesis no longer on. With the EEFP, patients experience a significant increase in quality of life. The tracks with applied prosthesis could be extended enormously after the supply with the EEFP. The number of patients with unrestricted walking distance has doubled with the supply of EEFP.
Wearing comfort was significantly better with the EEFP [50, 51]. Rehabilitation time is significantly reduced by the EEFP. A look at the pie charts on the obstacles in everyday life shows how much the patients with the help of the EEFP better cope with everyday life compared to times with the shaft prostheses.
Overall, the results of this study correlate with the results of the works already cited above. Nevertheless, we were unable to accurately represent the economic aspects of both the shaft prostheses and the endo-exo-femoral prostheses because the evaluable study time available in this work was one year, meaning too short to oversee the cost. The difficulty to estimate the costs was that the majority of the patients came from supra-regional and therefore did not carry out their follow-up entirely in Lübeck, but instead close to home. This made it difficult to analyze the economic aspects accurately. Another limitation of this study is the small number of patients. A longer-term study and full follow-up of aftercare for both the shaft prosthesis and the EEFP would also provide more insight into the peculiar aspects of the two types of care. Nevertheless, it can be said on the basis of the tested patients that the costs of treatment for the EEFP are initially high compared to those of the shaft prosthesis (see case studies) Constantly increased costs and with uncomplicated endo-exo-restoration after 4-5 years the breakeven point has been reached and henceforth the bone guided prosthetics can be reduced.
Conclusion
Based on this analysis, the Integral Leg Prosthesis (ILP) is of great benefit in the health and socio-economic aspects of rehabilitation. The day-to-day activities of patients are better managed with the ILP. In fact, the Process of acquiring and using an ILP is not only less cumbersome but also enables patients to go through a shorter period of recovery. Moreover, patients using ILP feel more secured in their movements thereby enabling them to rehabilitate faster and so facilitating a faster return to normal day-to-day activities and to jobsites. The shortened rehabilitation period contributes in cutting down on costs. Experiences from SMITH, HAGGSTROM and HANNSON have shown that, after a long period the cost of using an ILP is much more reduced than that of a conventional Prosthesis.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 07, Mar 2019Accepted: Tue 09, Apr 2019
Published: Fri 19, Apr 2019
Copyright
© 2023 Fungwe Jah. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSR.2019.01.03
Author Info
Christian Blöchle Fungwe Jah Horst H. Aschof
Corresponding Author
Fungwe JahDepartment of General, Visceral and Thoracic Surgery, University of Hamburg, Germany
Figures & Tables
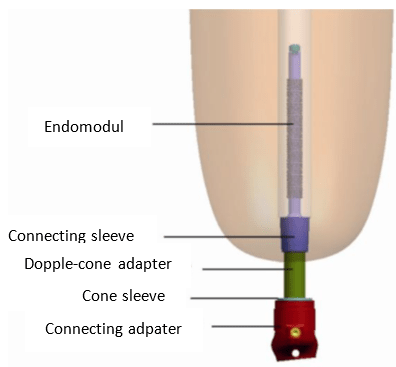
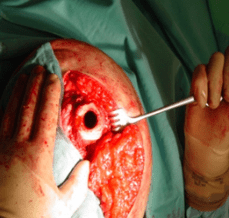
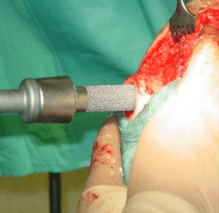
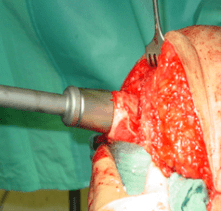
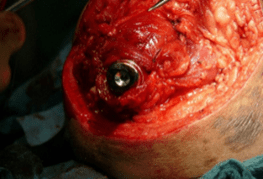
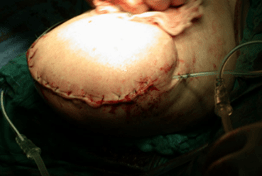

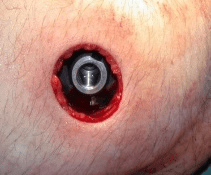

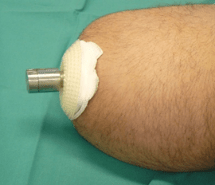

Table 1: Exemplary cost estimate for the provision of a shaft prosthesis within one year
For patient 1: (2009-2010)
|
Cost (gross)/Euros |
|
|
Elastic plaster bandages |
16,79 |
|
Cellona plaster bandages |
150,14 |
|
Thermolyn, stiff |
104,34 |
|
Clutch Lock |
299,30 |
|
ICECROSS Transfemoral standard |
837,72 |
|
Perlon pull-on stocking |
17,82 |
|
Cotton stump sock |
15,96 |
|
Thigh shaft made of cast resin |
1483,11 |
|
Knee mounting |
8,88 |
|
Flexible stem for thigh prosthesis |
373,95 |
|
Clutch-lock |
332,87 |
|
Icecross transfemoral Standard |
931,67 |
|
Mounting Adapter |
17,75 |
|
Working hours |
1653,83 |
|
Stockings |
78,88 |
|
Repair on shaft |
373,95 |
|
Working hours |
145,32 |
|
Stockings |
46,30 |
|
Medi RELAX Night care |
197,42 |
|
Dressinghelp |
64,95 |
|
Shank in clasp technology |
1790,61 |
|
Foam Form + connection cap |
473,17 |
|
Knee mounting |
7,98 |
|
Stockings |
46,30 |
|
Final sum |
9469,01 |
Table 2: Exemplary cost estimate for the provision of a shaft prosthesis within one year
Patient 2 (2008-2009)
|
Cost(gross)/Euros |
|
|
Plaster negative |
171,20 |
|
Schaft |
1600,00 |
|
Fitting |
149,80 |
|
Connection Adapter |
37,45 |
|
lamination anchor |
116,63 |
|
Hospital care |
25,64 |
|
Stem narrowing |
119,00 |
|
Hospital care |
28,51 |
|
Butt pads |
35,70 |
|
Final sum |
2283,93 |
Table 3: Exemplary cost statement for the supply of an EEFP within one year.
Patient 3
|
Cost (gross)/Euros |
|
|
Step 1 |
4317,54 |
|
Step 2 |
4317,54 |
|
Reimbursement implant by the health insurance company to hospital |
4200 |
|
Knee connection adapter |
1259,50 |
|
Allen key |
27,85 |
|
Extension module |
1046,72 |
|
Working hours |
453,99 |
|
Torsionsadaptation |
474,10 |
|
Working hours |
162,14 |
|
Final sum |
16259,38 |
Table 4: Exemplary cost statement for the supply of an EEFP within one year.
Patient 4
|
Service and Material |
Cost (gross)/Euros |
|
Step 1 DRG 1.542 |
4806,97 |
|
Step 2 DRG 1.385 |
4317,54 |
|
Hospitalisation because of stoma complaints DRG 1.163 |
3625,49 |
|
Reimbursement implant by the health insurance company to hospital |
4200,00 |
|
Extension module |
1046,72 |
|
Knee connection adapter |
1259,50 |
|
Allen key |
27,85 |
|
Working hours |
713,41 |
|
Final sum |
19997,48 |
References
- Sathishkumar S, Manigandan C, Asha T, Charles J, Poonoose PP et al. (2004) A cost-effective, adjustable, femoral socket, temporary prosthesis for immediate rehabilitation of above-knee amputation. Int J Rehabil Res 27: 71-74. [Crossref]
- Aschoff HH, Juhnke DL (2012) [Evaluation of 10 years’ experience with endo-exo femur prostheses- background, data and results]. Z Orthop Unfall 150: 607-614. [Crossref]
- RACK A. (2003) Med. Dissertation: Psychosoziale Auswirkungen posttraumatischer Amputationen an der unteren Extremitäten.
- Branemark R, Branemark PI, Rydevik B, Myers RR (2001) Osseointegration in skeletal reconstruction and rehabilitation: a review. J Rehabil Res Dev 38: 175-181. [Crossref]
- Branemark PI, Hansson BO, Adell R, Breine U, Lindstrome J et al. (1977) Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 16: 1-132. [Crossref]
- Hagberg K, Branemark R (2009) One hundred patients treated with osseointegrated transfemoral amputation prostheses--rehabilitation perspective. J Rehabil Res Dev 46: 331-344. [Crossref]
- Haggstrom EE, Hansson E, Hagberg K (2013) Comparison of prosthetic costs and service between osseointegrated and conventional suspended transfemoral prostheses. Prosthet Orthot Int 37: 152-160. [Crossref]
- Hagberg K, Branemark R, Gunterberg B, Rydevik B (2008) Osseointegrated trans-femoral amputation prostheses: prospective results of general and condition-specific quality of life in 18 patients at 2-year follow-up. Prosthet Orthot Int 32: 29-41 [Crossref]
- Staubach KH, Grundei H (2001) [The first osseointegrated percutaneous prosthesis anchor for above-knee amputees]. Biomed Tech (Berl) 46: 355-361. [Crossref]
- Pauls E (2010) Bachelorarbeit: Operative Ergebnisse und Lebensqualität nach Versorgungmit einer Endo-Exo-Femurprothese.
- CLAUSEN A (2007) Med. Dissertation. Orthopädische Klinik und Poliklinik Ludwigs-Maximilians-Universität München. Die EEFP-Endo-Exo-Femurprothese. Anwendung und Verlaufsbeobachtung sowie Anpassung des Implantatdesigns unter Berücksichtigung der Erkenntnis mikrobiologischer und histologischer Untersuchungen an der Grenzzone
- Prozeduren-Katalog DIMDI-OPS Version 2015.
- Brinckmann P (2002) Biomechanische Aspekte Der Haut. Manuelle Therapie 2: 87.
- Hagberg K, Branemark R (2001) Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int 25: 186-194. [Crossref]
- Aschoff HH, Clausen A, Tsoumpris K, Hoffmeister T (2011) [Implantation of the endo-exo femur prosthesis to improve the mobility of amputees] Oper Orthop Traumatol 23: 462-472. [Crossref]
- Dillingham TR, Pezzin LE, Mackenzie EJ, Burgess AR (2001) Use and satisfaction with prosthetic devices among persons with trauma-related amputations: a long-term outcome study. Am J Phys Med Rehabil 80: 563-571. [Crossref]
- Boonstra AM, Schrama J, Fidler V, Elisma WH (1994) The gait of unilateral transfemoral amputees. Scand J Rehabil Med 26: 217-223. [Crossref]
- Hagberg K, Haggstrom E, Uden M, Branemark R (2005) Socket versus bone-anchored trans-femoral prostheses: hip range of motion and sitting comfort. Prosthet Orthot Int 29: 153-163. [Crossref]
- Nicholas JJ (1993) Problems experienced and perceived by prosthetic patients. J Prosthet Orthot 5: 16-19.
- JohnstonRC, Smidt GL (1970) Hip motion measurements for selected activities of daily living. Clin Orthop Relat Res 72: 205-215. [Crossref]
- Gottschalk F (1999) Transfemoral amputation. Biomechanics and surgery. Clin Orthop Relat Res 361: 15-22. [Crossref]
- Jaegers SM, Arendzen JH, de Jongh HJ (1995) Changes in hip muscles after above-knee amputation. Clin Orthop Relat Res 319: 276-284. [Crossref]
- Gailey RS, Clark CR (2004) Physical therapy. In: Smith G, Michael JW, Bowker JH, editors. Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. Rosemount, IL: American Academy of Orthopaedic Surgeons 589-619.
- Murnaghan JJ, Bowker JH (2004) Musculoskeletal complications. In: Smith G, Michael JW, Bowker JH, editors. Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. Rosemont, IL: American Academy of Orthopaedic Surgeons 683-700.
- Aschoff HH, Clausen A, Hoffmeister T (2009) [The endo-exo femur prosthesis--a new concept of boneguided, prosthetic rehabilitation following above-knee amputation]. Z Orthop Unfall 147: 610-615. [Crossref]
- Albrektsson T, Albrektsson B (1987) Osseointegration of bone implants. A review of an alternative mode of fixation. Acta Orthop Scand 58: 567-577. [Crossref]
- Juhnke Dora-Lisa. Dissertation (2010) Orthopädische Klinik und Poliklinik Ludwigs-Maximilians-Universität München. Über die Endo-Exo-Femurprothese -Erarbeitung von Konzepten für die Qualitätssicherung knochengeführter Oberschenkelprothesen durch ganganalytische Bestimmungen und Auswertung von Druckverläufen unter dem Fuß.
- Legro MW, Reiber G, del Aguila M, Boone DA, Larsen JA et al. (1999) Issues of importance reported by persons with lower limb amputations and prostheses. J Rehabil Res Dev 36: 155-163. [Crossref]
- Waters RL, Perry j, Antonelli D, Hislop H (1976) Energy cost of walking of amputees: the influence of level of amputation. J Bone Joint Surg Am 58: 42-46. [Crossref]
- Huang CT, Jackson JR, Moore NB, Fine PR, Kuhlemeier KV et al. (1979) Amputation: energy cost of ambulation. Arch Phys Med Rehabil 60: 18-24. [Crossref]
- Jaegers SM, Vos LD, Rispens P, Hof AL (1993) The relationship between comfortable and most metabolically efficient walking speed in persons with unilateral above-knee amputation. Arch Phys Med Rehabil 74: 521-525. [Crossref]
- Andrews AW, Chinworth SA, Bourassa M, Garvin M, Benton D et al. (2010) Update on distance and velocity requirements for community ambulation. J Geriatr Phys Ther 33: 128-134. [Crossref]
- Bell JC, Wolf EJ, Schnall BL, Tis JE, Tis LL et al. (2013) Transfemoral amputations: the effect of residual limb length and orientation on gait analysis outcome measures. J Bone Joint Surg Am 95: 408-414. [Crossref]
- Baum BS, Schnall BL, Tis JE, Lipton JS (2008) Correlation of residual limb length and gait parameters in amputees. Injury 39: 728-733. [Crossref]
- Pernot HF, Winnubst GM, Cluitmans JJ, De Witte LP (2000) Amputees in Limburg: incidence, morbidity and mortality, prosthetic supply, care utilisation and functional level after one year. Prosthet Orthot Int 24: 90-96. [Crossref]
- Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken LN et al. (2001) Employment status, job characteristics, and work-related health experience of people with a lower limb amputation in The Netherlands. Arch Phys Med Rehabil 82: 239-245. [Crossref]
- Hagberg K (2005) Physiotherapy for patients having a trans-femoral amputation. In: Brånemark P-I, ed. The Osseointegration Book: From Calvarium to Calcaneus. Berlin, Chicago: Quintessence: 477-487.
- Hagberg K (2008) Osseoperception and Osseointegrated Prosthetic Limbs. Psychoprosthetics. P. Gallagher, D. Desmond and M. MacLachlan, Springer London: 131-140.
- Lundberg M, Hagberg K, Bullington J (2011) My prosthesis as a part of me: a qualitative analysis of living with an osseointegrated prosthetic limb. Prosthet Orthot Int 35: 207-214. [Crossref]
- Haraldson T, Carlsson GE (1977) Bite force and oral function in patients with osseointegrated oral implants. Scand J Dent Res 85: 200-208. [Crossref]
- Klineberg I, Murray G (1999) Osseoperception: sensory function and proprioception. Adv Dent Res 13: 120-129. [Crossref]
- van Steenberghe D (2000) From osseointegration to osseoperception. J Dent Res 79: 1833-1837. [Crossref]
- Klineberg I, Calford MB, Dreher B, Henry P, Macefield V et al. (2005) A consensus statement on osseoperception. Clin Exp Pharmacol Physiol 32: 145-146. [Crossref]
- Rydevik B (1994) Amputation prostheses and osseoperception in the lower and upper extremity. In: Brånemark P-I, Rydevik B, Skalak R, eds. Osseointegration in Skeletal Reconstruction and Joint Replacement. Berlin, Chicago: Quintessence: 175-182.
- Schoppen T, Boonstra A, Groothoff JW, van Sonderen E, Goeken LN et al. (2001) Factors related to successful job reintegration of people with a lower limb amputation. Arch Phys Med Rehabil 82: 1425-1431. [Crossref]
- Dasgupta AK, McCluskie PJ, Patel VS, Robins L (1997) The performance of the ICEROSS prostheses amongst transtibial amputees with a special reference to the workplace--a preliminary study. Icelandic Roll on Silicone Socket. Occup Med (Lond) 47: 228-236. [Crossref]
- Millstein S, Bain D, Hunter GA (1985) A review of employment patterns of industrial amputees--factors influencing rehabilitation. Prosthet Orthot Int 9: 69-78. [Crossref]
- Fisher K, Hanspal RS, Marks L (2003) Return to work after lower limb amputation. Int J Rehabil Res 26: 51-56. [Crossref]
- Whyte AS, Carroll LJ (2002) A preliminary examination of the relationship between employment, pain and disability in an amputee population. Disabil Rehabil 24: 462-470. [Crossref]
- Hagberg K, Hansson E, Branemark R (2014) Outcome of percutaneous osseointegrated prostheses for patients with unilateral transfemoral amputation at two-year follow-up. Arch Phys Med Rehabil 95: 2120-2127. [Crossref]
- Van de Meent H, Hopman MT, Frolke JP (2013) Walking ability and quality of life in subjects withtransfemoral amputation: a comparison of osseointegration with socket prostheses. Arch Phys Med Rehabil 94: 2174-2178. [Crossref]
- Haggstrom EE, Hansson E, Hagberg K (2013) Comparison of prosthetic costs and service between osseointegrated and conventional suspended transfemoral prostheses. Prosthet Orthot Int 37: 152-160. [Crossref]
- Juhnke DL, Beck JP, Jeyapalina S, Aschoff HH (2015) Fifteen years of experience with Integral-Leg- Prosthesis:Cohort study of artificial limb attachment system. J Rehabil Res Dev 52: 407-420. [Crossref]
- Smith DG, Horn P, Malchow D, Boone DA, Reiber GE et al. (1995) Prosthetic history, prosthetich charges, and functional outcome of the isolated, traumatic below-knee amputee. J Trauma 38: 44-47. [Crossref]
