Colonic Stent as “Bridge to Surgery” and Its Complications: A Case Report
A B S T R A C T
Introduction: Endoluminal colonic stents can be used as a palliative solution in case of neoplastic subocclusions of the bowel and in some cases, they have been proposed as a temporary solution, in place of the derivative stoma, waiting for radical surgery. The "bridge to surgery" solution however can be complicated by perforations or dislocations that can make the patient's cancer treatment more complex.
Case Presentation: A seventy-nine-year-old female patient presented a medium sigma adenocarcinoma that was treated initially with a stent to solve the bowel subocclusion. The procedure was complicated by a perforation that leaded to a modification of the TNM stage and consequently of the oncological therapeutic attitude.
Conclusion: Self expandable stents could be used to solve the bowel occlusion to replace the derivative stoma performed in urgency. These procedures guarantee a better quality of life and generally less morbidity. However, an accurate assessment of the risks resulting from the positioning of the stents is necessary, avoiding the implant of the stent in tortuous or angled sections of the bowel with a high risk of decubitus and consequently of micro or macro perforations.
Keywords
Colorectal cancer, self-expandable stents, bowel occlusion, operative colonoscopy
Introduction
Colorectal cancer (CRC) incidence and mortality rates vary markedly around the world. Globally, CRC is the third most commonly diagnosed cancer in males and the second in females, with 1.8 million new cases and almost 861,000 deaths in 2018 according to the World Health Organization GLOBOCAN database [1]. Previous studies demonstrated that 8-29% of patients with primary CRC present malignant colonic obstruction. In the past, emergency surgery has been the primary treatment for malignant colonic obstruction. During the 90’s, self-expandable stents have become increasingly popular to treat the obstruction of different segments of the digestive tract in order to allow a correct staging of the neoplasm and allow to procrastinate the definitive surgical intervention avoiding the creation of a temporary stoma [2]. We report a case regarding a visceral perforation as a complication of the temporary positioning of an endoluminal stent at the level of the middle sigma.
Case Report
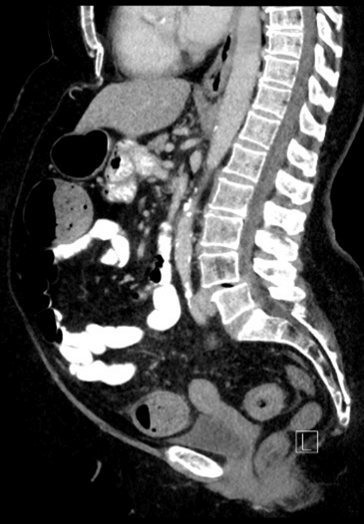
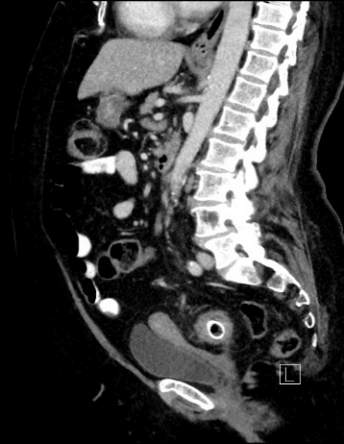
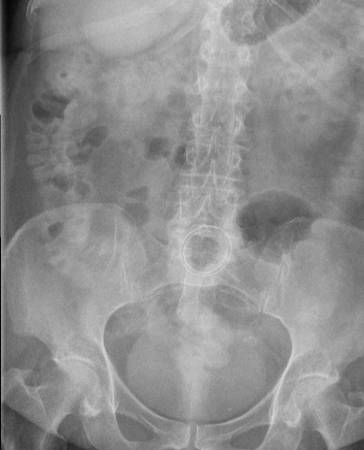
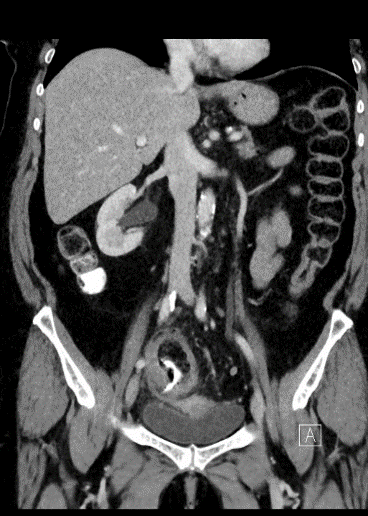
A 79 years old woman presented a sigmoid adenocarcinoma that was treated with a sigma stent as a bridge to surgery and that developed a colon perforation and ended up to be a pT4 a, pN0 (0/21) V0, G2, R0, M1 cy + from an initial stage of PT2, changing the whole prognosis and the whole treatment. S.M. is a 79-year-old woman with COPD and arterial hypertension that presented abdominal pain with no stools since 2 days. A CT scan showed a circumferential thickening of the sigma walls with a minimal infiltration of perisigmoid adipose tissue and an important fecal impaction of the whole upstream colon compatible with a sigma neoplasia (Figure 1) while colonoscopy showed a stenosing lesion of the medium sigma at 30 cm from the anal margin. After an interview with the patient who refused a temporary stoma, a metallic stent was therefore positioned from the gastroenterologist as a ‘’bridge to surgery’, in order to allow complete staging and to face the definitive surgical intervention in elective conditions (Figures 2 & 3). Histological examination of the biopsies showed the presence of a moderately differentiated adenocarcinoma of the colon. The patient restarted a normal feeding with regular bowel function and went home with the resolution of symptoms.
Figure 1: Sagittal image from a contrast enhanced CT scan showing a circumferential thickening of the sigma walls with a minimal infiltration of perisigmoid adipose tissue.
Figure 2: Sagittal image from a contrast enhanced CT scan showing the self expanding metallic stent positioned as a “bridge to surgery”.
Figure 3: Abdominal CR image showing the correct positioning of the self expanding metallic stent.
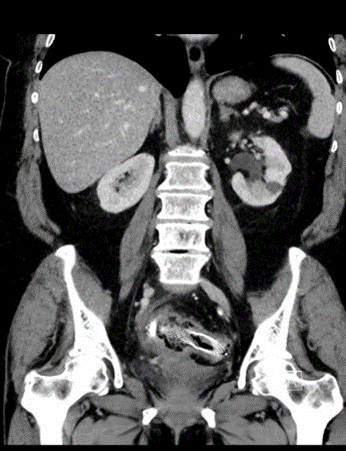
Seven days later the patient came back to the emergency room because of some cramp-like abdominal pain localized in the lower quadrants. The CT-scan showed a small air bubble located on the anterior wall of the stent (Figures 4 & 5). The patient underwent a laparotomy with sigmoid and rectum resection. The histology showed a moderately differentiated adenocarcinoma with adipose tissue and serosa perforation due to the ischemic necrosis of the sigma wall where the stent was placed.
Figure 4: Axial CT scan performed 7 days after stent positioning, showing sign of stent diplacement into the bowel lumen and infiltration of perisigmoid adipose tissue.
Figure 5: Coronal image from a contrast enhanced CT scan performed 7 days after stent positioning showing stent displacement and high suspicion of bowel perforation.
Furthermore, peritoneal fluid washing showed malignant cells. The patient went finally home in good conditions. A PET-TC performed one month later showed the presence of increased glucometabolic activity and presence of micronodules in the pelvic excavation, in the Douglas hollow and in the mesorect were highly suspicious for peritoneal carcinosis. Because of the pT4a stage and the positivity peritoneal lavage recognized as a negative prognostic factor conditioning recurrence (peritoneal and extraperitoneal) and survival, chemotherapy with fluoropyrimidine with oxaliplatin has been proposed to the patient.
Discussion
Obstruction of the left colon may be the first manifestation of colorectal cancer. Surgery performed in emergency often leads to the creation of a stoma. This choice is burdened by high morbidity and prolonged periods of hospitalization. According to these considerations, in recent years it has been proposed the placement of temporary metal stents that would allow surgery to be delayed in elective conditions. Self-expandable metallic stents are being used increasingly to treat the obstruction of different segments of the digestive tract. Its use has extended to colonic obstruction either as a definitive palliative procedure or as a primary step towards elective open surgery. It could be a minimally invasive alternative to urgent treatment, followed later on by elective colectomy.
Currently indications for stent placement in patients with malignant colorectal disease are temporary stenting usually in partial obstruction of the colon as a “bridge to surgery” to avoid emergency surgery and palliation in colorectal cancer patients or in extra colonic tumors causing acute abdominal obstruction (e.g. advanced gastric cancer, ovarian cancer …et cetera). Colonic stent placement seems to be relatively safe and effective and has some advantages over surgery but could be associated with complications. Possible adverse complications are perforation, stent migration, stent obstruction, haemorrhages and pain [3, 4, 5]. As far as the perforation is concerned, this complication may occur immediately after the procedure or after months [6]. The perforation rate of colonic stenting is 7.4% [7]. Almost 70% of perforations occur in the first week after stent placement [7]. Stent design, benign etiology, and bevacizumab were identified as risk factors for perforation [7]. Intraprocedural stricture dilation and concomitant chemotherapy were not associated with an increased risk of perforation [7].
In our case the perforation caused the spreading of the tumoral cells from the abdominal wall to the whole pelvis, changing the whole prognosis and the whole treatment. According to the recent studies, it is described that elective surgery after stent insertion does not adversely affect long-term oncologic outcomes [8]. Many studies comparing emergency surgery to the use of stents as a bridge to surgery demonstrate a lower rate of a temporary and permanent stoma and a lower short-term morbidity in a patient undergoing stent placement [9]. On the other hand, until more long-term oncological studies are available, stenting cannot be established as the gold standard of treatment [7]. Surgery was associated with clinical success, while stents showed shorter hospital stay and fewer definitive stomas [7]. In addition to that, stents could be an alternative for patients with incurable obstructive tumors in situation of emergency (acute abdomen) and moreover, with the advantage of early hospital discharge without a stoma [7].
Conclusion
The review of the literature suggests the validity of the use of stents both in primitive colorectal tumors and in the extravisceral forms [10]. In this way a rapid resolution of the occlusive clinical set is achieved with a reduction in the number of emergency surgical procedures (already worsened by a high morbidity, mortality and the need for intestinal derivation that is often definitive) with an improvement in the quality of life of terminal patients and optimal preparation for surgery in operable patients or candidates for neoadjuvant therapy with the aim of performing radical surgery [11]. Besides, studies show that elective surgery after stent insertion does not adversely affect long-term oncologic outcomes [8].
Indication for positioning of the stent, however, must be carefully assessed as the tortuosity of the stenotic or colic tracts immediately proximal and distal can favour the decubitus of the stent on the intestinal wall and cause necrosis and perforation of the bowel. It is therefore the authors' opinion and responsibility to recommend extreme attention and an accurate anatomical study of the obstruction before giving indication to temporary stenting, since the perforation, as in our case, modify the clinical picture and oncological prognosis, as a consequence of the peritoneal spread of the carcinoma initially confined to the visceral wall.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Sat 07, Nov 2020Accepted: Tue 17, Nov 2020
Published: Fri 11, Dec 2020
Copyright
© 2023 Marco De Monti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2020.02.05
Author Info
Elena Pastore Giovanna Schiavone Emanuele Meroni Francesco Salmoiraghi Marco De Monti
Corresponding Author
Marco De MontiEOC - Beata Vergine Regional Hospital, Department of Surgery, Mendrisio, Switzerland
Figures & Tables
References
- Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol 14: 89-103. [Crossref]
- Ribeiro IB, de Moura DTH, Thompson CC, de Moura EGH (2019) Acute abdominal obstruction: Colon stent or emergency surgery? An evidence-based review. World J Gastrointest Endosc 11: 193-208. [Crossref]
- Kim C, Park JJ, Seo YS, Jang YJ, Lee JY et al. (2005) Complications of Self-Expandable Colorectal Stenting for the Treatment of Acute Large Bowel Obstruction. Gastrointest Endosc 61: AB262.
- Stankiewicz R, Kozieł S, Pertkiewicz J, Zieniewicz K (2018) Outcomes and complications of self-expanding metal stent placement for malignant colonic obstruction in a single-center study. Wideochir Inne Tech Maloinwazyjne 13: 53-56. [Crossref]
- Small AJ, Coelho Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71: 560-572. [Crossref]
- Lee YJ, Yoon JY, Park JJ, Park SJ, Kim JH et al. (2018) Clinical outcomes and factors related to colonic perforations in patients receiving self-expandable metal stent insertion for malignant colorectal obstruction. Gastrointest Endosc 87: 1548-1557.e1. [Crossref]
- Van Halsema EE, Van Hooft JE, Small AJ, Baron TH, García Cano J et al. (2014) Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc 79: 970-982.e7. [Crossref]
- Yang SY, Park YY, Han YD, Cho MS, Hur H et al. (2019) Oncologic Outcomes of Self-Expandable Metallic Stent as a Bridge to Surgery and Safety and Feasibility of Minimally Invasive Surgery for Acute Malignant Colonic Obstruction. Ann Surg Oncol 26: 2787-2796. [Crossref]
- Ribeiro IB, Moura DTH, Thompson CC, Moura EGH (2019) Acute abdominal obstruction: Colon stent or emergency surgery? An evidence-based review. World J Gastrointest Endosc 11: 193-208. [Crossref]
- Alcantara M, Serra X, Bombardó J, Falcó J, Perandreu J et al. (2007) Colorectal stenting as an effective therapy for preoperative and palliative treatment of large bowel obstruction: 9 years’ experience. Tech Coloproctol 11: 316-322. [Crossref]
- Cantarella F, Bugiantella W, Mingrone E, Graziosi L, Ricci P et al. (2009) Preliminary experience on the application of metallic stents for treatment of colorectal malignant stenosis. Ann Ital Chir 80: 127-130. [Crossref]
