Co-Existence of a Rudimentary Non-Communicating Horn with a Unicornuate Uterus in Association with 2 Components of the VACTERL Association: A Case Report
A B S T R A C T
The prevalence of congenital uterine anomalies has been reported as 6.7% in the general population. The unicornuate uterus accounts for 2.4-13% of all Mullerian anomalies and has a prevalence of 1:1000. A unicornuate uterus may be present alone or with a rudimentary horn and 75-90% of rudimentary horns are non-communicating. A pregnancy in the rudimentary horn may lead to uterine rupture, haemoperitoneum with a high risk of maternal mortality. The association of a unicornuate uterus with a non-communicating uterine horn to the VACTERL association of defects (vertebral anomalies, anorectal malformations, cardiovascular anomalies, tracheoesophageal fistula, esophageal atresia, renal anomalies and limb defects) has been described only twice in the literature. We report a patient who was born with an extra thumb and had a trachea-bronchial remnant with oesophageal stenosis that were both operated on earlier, and they were associated with a non-communicating rudimentary uterine horn. To the best of our knowledge, this is the third case reported in the literature of a VACTERL association to a unicornuate uterus with a non-communicating functional rudimentary horn. Given the high risk for the patient if pregnant an early diagnosis is paramount. This case highlights the importance of considering Mullerian defects in the young patient born with components of the VACTERL association.
Keywords
Mullerian anomalies, VACTERL association, unicornuate uterus with rudimentary horn
Introduction
The prevalence of congenital uterine anomalies has been reported as 6.7% (95% CI, 6.0-7.4) in the general population, although women with recurrent miscarriage have a prevalence of 16.7% (95% CI, 14.8-18.6) [1]. The unicornuate uterus is the consequence of the abnormal or failed development of one Mullerian duct and it accounts for 2.4-13% of all Mullerian anomalies [2]. The prevalence of unicornuate uterus in the general population is 1:1000 [1]. Approximately 75-90% of cases of rudimentary horns are non-communicating [3]. A unicornuate uterus (or Hemi-uterus) with a rudimentary horn (communicating or not) belongs to the U4a ESHRE/ESGE classification [4]. Pregnancy in the rudimentary horn is rare (1:100,000) [5]. It may, however, lead to uterine rupture usually with an emergency presentation associated with haemoperitoneum and high risk of maternal mortality [6]. There is an unusual association of birth defects first described by Say B and Gerald P in 1968, later described with the acronym of VATER: V (vertebral defect), A (anal atresia), TE (tracheoesophageal fistula), and R (radial dysplasia and renal defects) by Quan in 1973 and followed by the acronym VACTERL (addition of limb defects) in 1976 [7-9]. We report a patient with a unicornuate uterus and a non-communicating rudimentary horn with a link to the VACTERL association.
Case Presentation
An 18-year-old woman was referred to our clinic complaining of severe dysmenorrhoea (8/10), pelvic pain and dyspareunia. Her menstrual cycle was irregular. She had undergone laparoscopic excision of endometriosis and insertion of a Mirena coil 5 months before which made no difference to her symptoms. She had attained menarche at the age of 13. She had been using the combined contraceptive pill for over the past 4 years with no relief of her dysmenorrhoea. Her surgical history included the excision of an extra thumb and the resection of a tracheo-bronchial remnant with primary esophageal anastomosis and fundoplication followed by endoscopic esophageal dilatations. Her physical appearance was normal, and her secondary sexual characteristics were normally developed. A bimanual examination revealed moderate discomfort on deep palpation and mobilization of the cervix. Blood tests including levels of CA 125 were reported as normal. Analysis of peripheral blood revealed a 46 XX normal female karyotype. Pelvic magnetic resonance imaging revealed two uterine horns with the left horn measuring 78 x 30 x 23 mm, containing a coil, and communicating with the cervical canal. The right horn was smaller than the left one and had an endometrial canal but showed no communication with the left horn. It would appear to be attached via a thick tissue band (Figure 1). Both ovaries revealed normal characteristics. The renal tract imaging revealed both kidneys of normal appearance and size.
Figure 1: MRI findings: There are 2 separated horns identified with the left horn communicating with the cervical canal. The right horn has an endometrial canal of its own which does not seem to communicate with the left horn or cervix and appears to be attached to the uterus via soft tissue band.
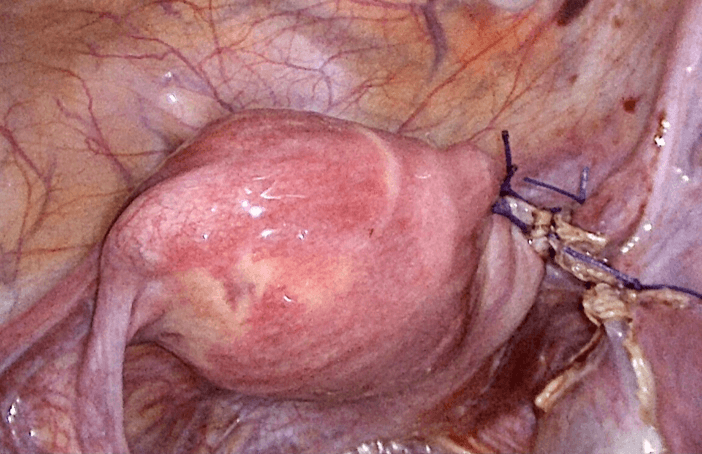
At laparoscopy a small right rudimentary horn was confirmed, and it was attached to the left unicornuate uterus by a thick band of tissue. The ovaries and Fallopian tubes had a normal appearance (Figure 2). There was no evidence of endometriosis. The appendix had a normal appearance. The coil was removed, and an intrauterine manipulator placed after a hysteroscopy was performed. The right ureter was identified retroperitoneally and dissected off, after the sectioning of the round ligament and the right Fallopian tube using a LigasureTM (Medtronic) device. The main artery to the rudimentary horn coursed lower and lateral to the left unicornuate uterus and it was involved by the above referred band of tissue. After the band of tissue was dissected off the arterial supply was diathermied and cut. Transillumination by hysteroscopy helped to delineate the plane of dissection. Two separated stitches of vicryl were applied to the lateral edge of the unicornuate uterus to reinforce its wall. The rudimentary horn was extracted after contained knife morcellation and using a laparoscopic endobag. Extensive lavage was done using Hartman’s solution (Figure 3). A Mirena coil was inserted at the end. The operating time was 110 minutes. The patient was discharged home the following day. The histology confirmed proliferative endometrium in the resected rudimentary horn. Eight months after the above surgery the patient is still pain free.
Figure 2: Operative findings. A left unicornuate uterus with a rudimentary horn on the right side with some degree of separation in between. The Fallopian tubes and both ovaries appear to be normal with the right fallopian tube inserting into the rudimentary horn.
Figure 3: The rudimentary horn has been excised as well as the ipsilateral Fallopian tube. The right lateral aspect of the unicornuate uterus has been reinforced with 2 separated stitches of vicryl.
Discussion
The prevalence of a unicornuate uterus in the general population is 1:1000 and is the consequence of the abnormal or failed development of one Mullerian duct, accounting for 2.4-13% of all Mullerian anomalies [1, 2]. Approximately 75-90% of cases of rudimentary horns are non-communicating [3]. Pregnancy in a non-communicating horn is rare (1:100,000) and it has been attributed to the trans-peritoneal migration of spermatozoa [5, 10]. Early diagnosis is challenging, and pregnancy progression usually results in the rudimentary horn rupture around the second trimester in 80-90% cases becoming an emergency with the consequent high maternal morbidity and mortality [11-18].
Although the diagnosis in the non-pregnant condition is difficult the presence of dysmenorrhoea (70% cases) and an adnexal mass together with haematometra (50% cases) should raise the possibility of a Mullerian anomaly. However, as endometriosis may be present in 20-40% cases and this is a very common condition, the diagnosis may be delayed [19]. A dedicated ultrasonography exam may be valuable in these circumstances to confirm the presence of a rudimentary horn and the extent of the functioning endometrium, but recently Magnetic Resonance Imaging has become crucial in the evaluation of Mullerian anomalies allowing for the simultaneous assessment of the anatomy, type of attachment between the rudimentary horn and the unicornuate uterus, and the study of the urinary tract as Mullerian anomalies are associated with renal anomalies in 40.5% cases and with one-sided renal agenesis in 28% [20-23].
Regarding treatment, there are 2 options: the first option involving a metroplasty, but long-term follow-up is still scarce with only one report of a patient who conceived by in vitro fertilization and embryo transfer and was delivered from twins by caesarean-section at 33 weeks [24]. The second option is the surgical excision of the non-communicating rudimentary horn, which was chosen in the patient we report. Although it does not improve the reproductive outcome it had the goal of treating the persistent severe dysmenorrhoea caused by haematometra, preventing any possible endometriosis recurrence and avoiding a pregnancy in the rudimentary horn with a potential life-threatening uterine rupture.
The laparoscopic technique is mainly determined by the type of anatomical attachment between the rudimentary horn and the unicornuate uterus [25, 26]. Preoperative magnetic resonance should reveal if the rudimentary horn is firmly attached to the unicornuate uterus or if it is attached by a band of tissue like in the present case. The use of the hysteroscope during surgery is advisable to assess the normality of the unicornuate uterine cavity and also to perform the trans-illumination of the unicornuate uterus in order to confirm the plane of dissection between the horns and to minimize the risk of entering the cavity of the unicornuate uterus when transecting off the rudimentary horn. The retroperitoneal dissection of the ureter is advisable to reduce the risk of ureteral damage as there is a high risk of ureteral malposition and the presence of aberrant vessels [25]. The ipsilateral salpingectomy is removed to avoid the rare occurrence of an ectopic pregnancy.
The VACTERL association is a non-random association of birth defects that affects multiple parts of the body (V-vertebral anomalies, A-anorectal malformations, C-cardiovascular anomalies, T-tracheoesophageal fistula, E-esophageal atresia, R-renal anomalies and L-limb defects). It should be defined by at least 2 or 3 component defects [27]. There is no cognitive impairment of the individual. The aetiology of VACTERL association is not well understood. A specific genetical abnormality has not been found but sporadic cases have revealed mutations in FGF8, HOXD13, ZIC3, PTEN, FANCB, FOXF1 and TRAP1 genes and mitochondrial DNA [28].
The co-existence of the VACTERL association to a unicornuate uterus with a non-communicating functioning rudimentary horn was first described by Nunes in a 28-year-old woman known to have a missing vertebra, imperforated anus, anovaginal fistula, right renal agenesis and an extra digit in one hand in 2009 [29]. The second case reporting the association of a non-communicating functioning rudimentary horn with the VACTERL association was in a 17-year-old woman with a previous tracheoesophageal malformation, repair of imperforated anus and left renal agenesis in 2019 [30]. We report a patient who had a unicornuate uterus with a coexistent non-communicating rudimentary uterine horn who was born with an extra thumb and had a trachea-bronchial remnant with esophageal stenosis that were both operated earlier on. To the best of our knowledge this is the third case reported in the literature of VACTERL association to a unicornuate uterus with a non-communicating functional rudimentary horn. This case highlights the importance of considering Mullerian defects in a woman born with features of the reported VACTERL association.
Conclusion
The presence of a non-communicating rudimentary horn associated to a unicornuate uterus carries a high risk for maternal mortality if the diagnosis is delayed and uterine rupture occurs during pregnancy. This case report stresses the importance of considering the diagnosis of a Mullerian defect in a patient born with components of the VACTERL association.
Acknowledgement
I am grateful to the theatre surgical team at Braemar Hospital, Hamilton, New Zealand for their invaluable assistance.
Approval Statement
The Braemar Hospital Clinical Committee has approved this submission.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 07, Jul 2021Accepted: Wed 21, Jul 2021
Published: Tue 03, Aug 2021
Copyright
© 2023 Jose D Roman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CROGR.2021.02.01
Author Info
Corresponding Author
Jose D RomanDepartment of Gynaecology, Braemar Hospital, Hamilton Lake, Hamilton, New Zealand
Figures & Tables


References
1. Saravelos SH,
Cocksedge KA, Li TC (2008) Prevalence and diagnosis of congenital uterine
anomalies in women with reproductive failure: a critical appraisal. Hum
Reprod Update 14: 415-429. [Crossref]
2. Caserta D, Mallozi M, Meldolesi C, Bianchi P, Moscarini M (2014) Pregnancy
in a unicornuate uterus: a case report. J Med Case Rep 8: 130. [Crossref]
3. Buttram VC Jr,
Gibbons WE (1979) Müllerian anomalies: a proposed classification. (An analysis
of 144 cases). Fertil Steril 32: 40-46. [Crossref]
4. Grimbizis GF,
Gordts S, Di Spiezio Sardo AD, Brucker S, De Angelis C et al. (2013) The
ESHRE/ESGE consensus on the classification of female Genital tract congenital
anomalies. Hum Reprod 28: 2032-2044. [Crossref]
5. Engmann L, Schmidt
D, Nulsen J, Maier D, Benadiva C (2004) An unusual anatomic variation of a
unicornuate uterus with normal external uterine morphology. Fertil Steril
824: 950-953. [Crossref]
6. Shah NH, Deshmukh
M, Somani A, Paranjpe SH (2017) Laparoscopic Management Of Non Communicating
Rudimentary Horn Pregnancy. JPGO 4.
7.
Say
B, Gerald PS (1968) A new polydactyly/imperforate-anus/vertebral-anomalies syndrome? Lancet
21 2: 688. [Crossref]
8. Quan L, Smith DW
(1973) The VATER association. Vertebral defects, Anal atresia, T-E fistula with
esophageal atresia, Radial and Renal dysplasia: a spectrum of associated
defects. J Pediatr 82: 104-107. [Crossref]
9.
Baumann W,
Greinacher I, Emmrich P, Spranger J (1976) [Vater or Vacterl syndrome (author's
transl)]. Klin Padiatr 188: 328-337. [Crossref]
10.
Dicker
D, Nitke S, Shoenfield A, Fish B, Meizner I et al. (1998) Laparoscopic
management of rudimentary horn pregnancy. Hum Reprod 13: 2643-2644. [Crossref]
11.
Goel
P, Kumar PK, Mehra R, Huria A (2007) Unruptured postdated pregnancy with a live
fetus in a noncommunicating rudimentary horn. Indian J Med Sci 61:
23-27. [Crossref]
12. Mengistu K, Bobe T,
Tilahun G, Kifle K, Geleta D (2020) Rudimentary Horn Pregnancy Diagnosed after Laparotomy.
Case Rep Obstet Gynecol 2020: 5816487. [Crossref]
13. Nishi H, Funayama
H, Fukumine N, Yagishita M, Nohira T et al. (2003) Rupture of pregnant
noncommunicating rudimentary uterine horn with fetal salvage: a case report. Arch
Gynecol Obstet 268: 224-226. [Crossref]
14. Kuscu NK, Lacin S,
Kartal O, Koyuncu F (2002) Rupture of rudimentary horn pregnancy at the 15th
week of gestation: a case report. Eur J Obstet Gynecol Reprod Biol 102:
209-210. [Crossref]
15. Daskalakis G,
Pilalis A, Lykeridou K, Anksaklis A (2002) Rupture of noncommunicating
rudimentary uterine horn pregnancy. Obstet Gynecol 100: 1108-1110. [Crossref]
16. Zaidi J, Carr J
(1994) Rupture of pregnant rudimentary uterine horn with fetal salvage. Acta
Obstet Gynecol Scand 73: 359-360. [Crossref]
17. Elsayegh A, Nwosu
EC (1998) Rupture of pregnancy in the communicating rudimentary uterine horn at
34 weeks. Hum Reprod 13: 3566-3568. [Crossref]
18. Oral B, Guney M,
Ozsoy M, Sonai S (2001) Placenta accreta associated with a ruptured pregnant
rudimentary uterine horn. Case report and review of the literature. Arch
Gynecol Obstet 265: 100-102. [Crossref]
19. Heinonen PK (1997)
Unicornuate uterus and rudimentary horn. Fertil Steril 68: 224-230. [Crossref]
20. Agacayak E, Peker
N, Yavuz M, Findik FM, Evsen MS et al. (2020) Rudimentary horn pregnancy - ten
years of experience. Ginekol Pol 91: 117-122. [Crossref]
21. Marten K,
Vosshenrich R, Funke M, Obenauer S, Baum F et al. (2003) MRI in the evaluation
of müllerian duct anomalies. Clin Imaging 27: 346-350. [Crossref]
22. Jayasinghe Y, Rane
A, Stalewski H, Grover S (2005) The presentation and early diagnosis of the
rudimentary uterine horn. Obstet Gynecol 105: 1456-1467. [Crossref]
23. Akar ME, Bayar D,
Yildiz S, Ozel M, Yilmaz Z (2005) Reproductive outcome of women with
unicornuate uterus. Aust N Z J Obstet Gynaecol 45: 148-150. [Crossref]
24. Zhang Y, Liu S,
Zhang X, Ding Y, Hua K (2019) Laparoscopic metroplasty for unicornuate uterus
with a functional noncommunicating rudimentary horn. Int J Gynaecol Obstet
149: 31-36. [Crossref]
25. Fedele L, Bianchi
S, Zanconato G, Berlanda N, Bergamini V (2005) Laparoscopic removal of the
cavitated noncommunicating rudimentary uterine horn: surgical aspects in 10
cases. Fertil Steril 83: 432-436. [Crossref]
26. Falcone T, Gidwani
G, Paraiso M, Beverly C, Goldberg J (1997) Anatomical variation in the
rudimentary horns of a unicornuate uterus: implications for laparoscopic
surgery. Hum Reprod 12: 263-265. [Crossref]
27. Rittler M, Paz JE,
Castilla EE (1996) VACTERL association, epidemiologic definition and
delineation. Am J Med Genet 63: 529-536. [Crossref]
28. Nakamura Y,
Kikugawa S, Seki S, Takahata M, Iwasaki N et al. (2015) PCSK5 mutation in a
patient with the VACTERL association. BMC Res Notes 8: 228. [Crossref]
29. Nunes N, Karandikar S, Cooper S, Jaganathan R, Irani S (2009) VATER/VACTERL syndrome (vertebra/anus/cardiac/trachea/esophogus/radius/renal/limb anomalies) with a noncommunicating functioning uterine horn and a unicornuate uterus: a case report. Fertil Steril 91: 1957.e11-1957.e12. [Crossref]
30. Obeidat R, Aleshawi AJ, Tashtush NA, Alsarawi H (2019) Unicornuate uterus with a rudimentary non-communicating cavitary horn in association with VACTERL association: case report. BMC Womens Health 19: 71. [Crossref]
