Cecal Volvulus Presenting after Onset of Acute Pancreatitis: A Case Report
A B S T R A C T
Cecal volvulus is a rare, potentially life-threatening cause of large bowel obstruction (LBO). Discerning LBO in the background of chronic episodes of epigastric or abdominal pain ensures timely treatment and reduces the risk of complications. Atypical demographic presentation may pose a clinical danger that can be best avoided with standardized diagnostic imaging. We report a case of cecal volvulus in a male patient with a history of alcohol use disorder and pancreatitis. The patient underwent a right hemicolectomy with small bowel resection and primary anastomosis.
Introduction
Volvulus occurs when a loop of bowel twists around itself and its supporting mesentery [1]. Cecal volvulus involves torsion of the cecum and ascending colon around the mesenteric vascular pedicles [2]. The annual incidence of cecal volvulus is 2.8-7.1 per million people, with the most commonly affected being female patients ages 40-60 years old [3, 4]. Cecal volvulus is responsible for only 1-1.5% of all adult intestinal obstructions and for 25-40% of all volvulus involving the colon, and serious complications include gangrene, bowel perforation, and peritonitis [5]. We present a 51-year-old male who presented with abdominal pain with a history of alcohol abuse and pancreatitis; his diagnosis of cecal volvulus was delayed due to suspected pancreatitis.
Case Presentation
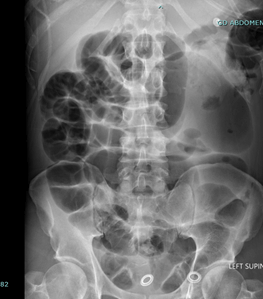
A 51-year-old male presented to the emergency department complaining of a three-day history of dull and worsening upper abdominal pain. The patient has a history of alcohol use and pancreatitis and stated that the abdominal pain felt similar to past episodes. He denied any nausea, vomiting, or changes in bowel movements, and the provisional diagnosis was considered to be pancreatitis. The physical examination revealed relatively normal vital signs with a temperature of 36.8ºC, heart rate of 95, and BP of 168/96. On general examination, minimal tenderness was found in the epigastric region without abdominal distention. Hematologic tests demonstrated normal values: white blood cell count of 8.1/mm3 and haemoglobin 12.9. Additional lab values were normal: ALT 13 U/L, AST 29 U/L, alkaline phosphatase 67 U/L, total bilirubin 0.6 mg/dL, lipase 167 U/L, and troponin <0.01. The initial x-ray showed no acute abnormalities, and abdominopelvic CT only demonstrated acute pancreatitis without fluid collection, a 4 cm hepatic hemangioma, and mild intrahepatic biliary duct dilation (Figure 1).
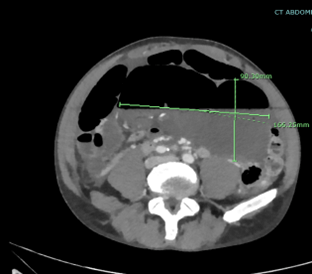
The patient returned to the ED two days later with diffuse abdominal pain, distension, and vomiting worsening for one and a half hours. He could pass gas but denied having a bowel movement for a few days. The X-ray showed a dilated loop of large bowel in the right hemiabdomen with multiple air-fluid levels seen within the small bowel consistent with small bowel obstruction (Figure 2). Abdominal computed tomography (CT) confirmed a large cecal volvulus with a high-grade small bowel obstruction and a mild to moderate amount of new ascites, which could be secondary to the high-grade bowel obstruction. (Figure 3).
Figure 1: A) Axial and B) coronal abdominal CT showing abnormalities in liver and pancreas. Large bowel abnormalities were not observed.
Figure 2: Supine abdominal radiograph showing the dilated cecum from the right lower quadrant to the left upper quadrant and the air-fluid level.
Figure 3: Axial abdominal CT scan with contrast showing marked distention of cecum measuring about 166 mm extending from the right lower quadrant to the epigastrium.
An exploratory laparotomy was performed through a midline incision, and upon entering the abdomen, immediate expression of foul-smelling ascites was cleared in the colon. Further, intraoperative findings displayed signs of bowel ischaemia in the cecum, right colon, and distal ileum, the cecum being frankly necrotic with a blackened appearance noted up to the level of the hepatic flexure. Upon evisceration of the small bowel, torsion along the mesentery was identified and relieved manually with no adhesions. A right hemicolectomy and small bowel resection with primary anastomosis were then performed. Enterotomy was created at the distal staple line to allow for manual decompression of the distended small bowel containing air and fluid. After 1 L of succus was evacuated from the small bowel, the distal staple line and enterotomy were resected. A primary staple was then used to transect the small bowel where it appeared healthy and, although still erythematous, mesentery was divided with the enseal device. A side-to-side and functional end-to-end anastomosis was created between the distal small bowel and the hepatic flexure.
The initial postoperative recovery was uneventful, with the patient reporting flatus and bowel movement. On the fifth postoperative day, the patient experienced abdominal distention due to small bowel obstruction and required nasogastric tube decompression. High-grade small bowel obstruction was observed on CT with a transition point in the region of anastomosis. The patient reported flatus and having bowel movements. Postoperative ileus was initially suspected, and the patient was monitored for potential resolution.
Persistent signs of bowel obstruction were observed. Gastrografin challenge was performed, and on the eleventh postoperative day, the patient was brought back to the operating room for likely revision of the ileocolic anastomosis and adhesiolysis. After manually confirming the patency of the anastomosis, adhesions present at the site were released. Depressive colotomy was then performed with the evacuation of 1800 cc of bilious fluid. Subsequent postoperative recovery was uneventful, and the patient was discharged on the fifteenth postoperative day of initial surgical intervention and the fourth day of the second operation.
Discussion
Cecal volvulus is a rare cause of intestinal obstruction in the United States, responsible for about 4% of cases of LBO [5]. The mean age of presentation is 61.8, and it is more common in patients with a history of post-surgical adhesions, chronic constipation, bedridden, or previous colonoscopy procedures. In the younger population, the cause could be due to mesenterium commune, other intestinal malformation, or excessive exercise [6]. In addition, the length of the mesentery directly affects the risk of cecal volvulus due to the increased mobility of the cecum and the risk of torsion along the long axis [7].
Despite this patient’s initial presentation with pancreatitis, it is important to keep bowel obstruction in the differential diagnosis due to the possibility of rapid progression and further complications. Any inflammation and obstruction of the large bowel can cause the accumulation of gas and dilation of the cecum and lead to axial torsion [7]. If not surgically corrected promptly, bowel ischaemia results in imminent necrosis and an increasing risk of severe complications such as peritonitis, gangrene, and bowel perforation. Due to the severe complications, it is important to recognize cecal volvulus promptly; symptoms are typically right abdominal pain, early absence of abdominal clicks, and asymmetric distension. The symptoms of colicky pain in the ileocecal region can manifest 2-3 days before permanent torsion occurs [8].
The definitive diagnosis occurs with radiographic imaging if three signs are present: cecum dilation, air-fluid level in the right lower quadrant, and an absence of gas in the colon, but 30% of patients do not show these radiographic features [8]. CT imaging can confirm the diagnosis in 90% of patients [9]. Signs on the radiograph are cecal enlargement, also known as comma appearance, abnormal cecal positioning, and whirl sign in which the whirl is composed of spiral loops of collapsed cecum into the distal colon. Distension is often noted along with small bowel distention with air-fluid levels and an empty distal colon; however, 10% of cases are only diagnosed intra-operatively [5].
Surgical intervention is regarded as the most definitive form of treatment, and nonoperative modalities are not utilized due to being less successful. Treatments such as colonoscopic reduction carry the risk of colonic perforation, and the success rate for reduction is only 30% [9]. Alternative procedures like simple detorsion and cecopexy are associated with recurrence rates of up to 13-75% and 20%, respectively compared to resection (0%) [9, 10]. Laparoscopic procedures are only beginning to be performed. However, they are associated with a high risk of perforation. Bowel resection with ileocolic anastomosis is considered the most effective surgical intervention in treating cecal volvulus. A right hemicolectomy was performed in this case, followed by ileocolic anastomosis due to bowel compromise.
Delayed treatment of cecal volvulus carries a mortality of over 30%. Most studies indicate patients should be treated within 24-72 hours after diagnosis [3]. Patients typically present to the emergency room with non-specific gastrointestinal symptoms such as abdominal pain, distension, vomiting, or constipation. The physical examination findings most commonly include abdominal tenderness and enlargement. In some cases, an abdominal mass is noted [11]. Despite abnormal history or irregular demographics, LBO should be considered. Delaying treatment is associated with poor outcomes, such as increased mortality risk in surgery, necrosis, and perforation. Even after treatment, patients have high morbidity due to prolonged ileus, wound infection, respiratory failure, and bowel obstruction [5].
Conclusion
If diagnosis is delayed, cecal volvulus is a rare cause of LBO with high mortality. Timely diagnosis occurs with radiographic imaging in patients with suspected bowel obstruction. However, presentation is generally nonspecific, and diagnosis may be delayed in patients with a history of alcohol abuse disorder and pancreatitis. Additionally, an atypical presenting demographic may serve as a confounding factor. An abdominal CT scan leads to a definitive diagnosis. The most effective form of treatment is surgical, with procedure variations depending on the presence of bowel ischaemia and patient haemostability. Patient outcomes depend most on timely diagnosis and treatment.
Article Info
Article Type
Case ReportPublication history
Received: Mon 04, Sep 2023Accepted: Tue 26, Sep 2023
Published: Fri 06, Oct 2023
Copyright
© 2023 Filip Siembida. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2023.03.05
Author Info
Alexander M. Kravets Filip Siembida Ashley Langley Ahmer Khan
Corresponding Author
Filip SiembidaTransitional Year Resident, Einstein Healthcare Network, East Norriton, USA
Figures & Tables

References
1.
Le CK, Nahirniak P,
Qaja E (2022) Cecal Volvulus. StatPearls [Internet]. [Crossref]
2.
Ramírez Ramírez MM,
Villanueva Sáenz E, Ramírez Wiella Schwuchow G (2017) Elective laparoscopic
right colectomy for caecal volvulus: case report and literature review. Cir
Cir 85: 87-92. [Crossref]
3.
Atamanalp SS, Ozogul
B, Kisaoglu A (2012) Cecal volvulus: a rare cause of intestinal obstruction. Eurasian
J Med 44: 115-116. [Crossref]
4. Majeski J (2005) Operative therapy for cecal volvulus combining resection
with colopexy. Am J Surg 189: 211-213. [Crossref]
5.
Khaniya S, Shakya VC,
Koirala R, Pokharel K, Regmi R et al. (2010) Caecal volvulus: a twisted tale. Trop
Doct 40: 244-246. [Crossref]
6.
Katoh T, Shigemori T,
Fukaya R, Suzuki H (2009) Cecal volvulus: report of a case and review of
Japanese literature. World J Gastroenterol 15: 2547-2549. [Crossref]
7.
Donhauser JL, Atwell S
(1949) Volvulus of the cecum with a review of 100 cases in the literature and a
report of six new cases. Arch Surg 58: 129-148. [Crossref]
8.
Zabeirou AA, Belghali
H, Souiki T, Majdoub KI, Toughrai I et al. (2019) Acute cecal volvulus: A
diagnostic and therapeutic challenge in emergency: A case report. Ann Med
Surg (Lond) 48: 69-72. [Crossref]
9.
Anderson JR, Welch GH
(1986) Acute volvulus of the right colon: an analysis of 69 patients. World
J Surg 10: 336-342. [Crossref]
10. Underhill J, Munding E, Hayden D (2021) Acute Colonic Pseudo-obstruction and Volvulus: Pathophysiology, Evaluation, and Treatment. Clin Colon Rectal Surg 34: 242-250. [Crossref]
11. Fenzl N, DeSilva SG, Scott J (2017) Cecal volvulus case report. Imaging Med, 9: 31-32.
