Case Report of an Aortic Laceration after a Posterior Approach for Lumbar Disc Herniation Repair
A B S T R A C T
The posterior approach for lumbar disc herniation surgeries is one of the most used methods worldwide [1]. Though rare, vascular issues can occur during surgery on the lower spine, with reported cases of arteriovenous fistulas, pseudoaneurysms, and vascular lacerations [2, 3]. Aortic tears, an uncommon yet serious complication of spinal surgery, have been documented [2].We report a specific instance of aortic injury following a left L3L4 lumbar disc herniation repair through the posterior approach, managed using an endovascular procedure called CERAB (Covered Endovascular Reconstruction of Aortic Bifurcation).
Keywords
Aortic laceration, lumbar disc herniation, vascular complication
Introduction
The posterior approach for lumbar disc herniation repair stands as an established and reliable technique. It has been used for several decades. However, this method does carry certain risks [1]. Iatrogenic vascular injuries subsequent to lumbar disc herniation procedures are rare but potentially lethal. They have been extensively documented in medical literature [2, 4]. Their incidence remains static, fluctuating between 0.01 and 0.05% over the past half-century [5, 6]. Mortality rates for these injuries range widely from 10 to 65%. It depends on several factors such as the time of the diagnosis, lesion dimensions, vessel type affected, and the patient's hemodynamic stabilization [1, 2, 5, 7, 8]. The anatomical proximity of vessels immediately anterior to the anterior longitudinal ligament renders them easily accessible yet notably vulnerable. Predominantly, the L4L5 vertebral level is implicated in these vascular injuries, primarily affecting the iliac arteries [2, 4, 5]. The primary suspected cause for vascular injury during lumbar disc herniation surgery often stems from excessive penetration by the pituitary rongeur [5, 9]. Here, we present the case of a patient treated for a disc herniation via the posterior approach complicated by an aortic laceration necessitating endovascular intervention.
Figure 1: A demonstration of a vascular injury mechanism during lumbar disc herniation surgery often stems from excessive penetration by the pituitary rongeur. Green: anterior longitudinal ligament.
Case Presentation
A 37-year-old male presented himself urgently to the spine surgery clinic in late October 2023 with uncontrolled cruralgia and anterior left thigh anaesthesia. An MRI performed a week earlier revealed a lumbar disc herniation at the L3L4 level, causing compression at the left L3 nerve root. Following the consultation, the patient underwent infiltration and was scheduled for surgery five days later. The surgical procedure proceeded uneventfully, maintaining stable vital signs and minimal blood loss. However, during the postoperative night, the patient began experiencing abdominal pain.
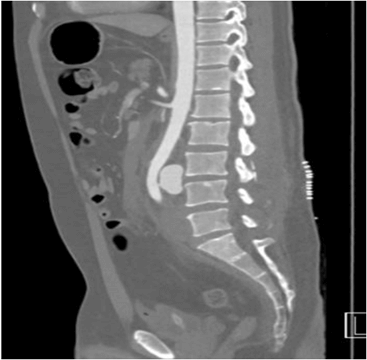
Figure 2: Angio-CT scan, sagittal section visualization of the posterior aortic laceration adjacent to the L3-L4 intervertebral space.
Figure 3: Angio-CT scan, axial section. Visualization of the posterior aortic laceration in relation to the L3-L4 intervertebral space.
By the first postoperative day, the abdominal discomfort escalated, although the clinical assessment exhibited a reassuringly soft and depressible abdomen. The patient's parameters remained within normal ranges, with a drain output of 5 cc and a recorded hemoglobin level of 13.5 g/dL (preoperative level: 15 g/dL). Upon attempting ambulation, taking around twenty steps, the patient experienced syncope accompanied by hypotension (80/40 mmHg) and tachycardia (114 bpm). Subsequent to the clinical presentation, a repeat blood analysis showed stable hemoglobin levels. A urinary bladder scan was done and ruled out a post-operative urinary retention. An emergent angio scanner was requested. The imaging revealed a 14 cm retroperitoneal hematoma with active bleeding originating from the abdominal aorta approximately 8 cm below the renal arteries, proximal to the aortic bifurcation. The patient was promptly transferred to the intensive care unit, maintaining hemodynamic stability. Considering this and the injury's localization, immediate intervention was undertaken in the operating room employing an endovascular approach. The procedure conceited in a covered endovascular reconstruction of aortic bifurcation (CERAB) utilizing a 16 × 48 mm begraft aortic stent and a kissing technique with two 8 × 57 mm beGraft stents (Bentley). Final arteriography demonstrated complete exclusion of the breach.
Subsequently, the patient was moved back to the intensive care unit for postoperative monitoring, receiving prophylactic amoxicillin/clavulanate. His clinical course thereafter showed progressive resolution of abdominal pain and complete cessation of cruralgia. A follow- up angio-scan conducted on the second postoperative day exhibited satisfactory stent patency and successful surgical outcomes without active hemorrhage. The immediate postoperative period and subsequent days demonstrated favourable clinical progress in terms of abdominal discomfort and wound healing. Discharge on the fifth postoperative day included lifelong antiplatelet therapy with 80 mg of acetylsalicylic acid once daily. At the one-month follow-up, the patient remained asymptomatic without any reported complications.
Figure 4: Angio-CT scan, frontal section. Highlighting the CERAB (covered endovascular reconstruction of aortic bifurcation).
Discussion
The incidence of vascular complications predominates in L4-L5 disc herniation surgeries, given the global prevalence of this surgical level. However, aortic injuries are more prevalent in L3- L4 disc herniation surgeries due to distinct anatomical relationships [2, 4, 5]. Accurately determining the incidence of these vascular complications proves challenging due to a selection bias in the literature because most of the cases reported were patients that survived [3, 4, 16]. However, an approximate occurrence of one vascular complication per spinal surgeon's career is estimated [2, 5, 10]. Hence, there's a crucial imperative to prompt healthcare professionals to report complications, enabling comprehensive registries for critical analysis and procedural improvement.
Risk factors contributing to vascular injuries during spinal interventions include delicate surgical manipulation of nearby anatomical structures, instrument sharpness, and excessive vascular compression. Patient-specific anatomical variations, such as atypical vessel positions or pre-existing vascular anomalies, heighten susceptibility to these injuries. Rigorous analysis of pre-operative imaging and surgery procedure planification is indispensable for precise delineation of neighbouring anatomical structures. Vascular injuries typically manifest as hypovolemic shock attributable to active hemorrhage, often presenting as hypotension, tachycardia, diminished haemoglobin levels, and uncontrolled pain. Notably, our case emphasized abdominal pain, observed in approximately 20% of similar cases [6]. Intraoperative bleeding visualization occurs in fewer than 50% of cases [4]. Thus, absence of intraoperative bleeding does not conclusively exclude vascular injury. Vigilant monitoring of patient parameters and daily clinical evaluations serve as pivotal indicators for potential vascular compromise. Consequently, surgeon familiarity with procedural complications is imperative for prompt management of postoperative anomalies.
Mortality rates linked to aortic lacerations vary widely, ranging from 18 to 38% [2, 4]. Immediate surgical intervention is crucial to prevent hemorrhagic shock. While open surgical repair via direct suturing is the traditional approach, it bears significant morbidity rating up to 50%, predominantly due to the posterior localization of these injuries. Endovascular management offers a less invasive alternative, offering lower morbidity and mortality rates [7, 10]. Hence, adopting endovascular techniques whenever feasible, particularly in hemodynamically stable patients, seems the best option. In the context of hemodynamically compromised patients, intraoperative angiography may be employed concomitantly for diagnostic purposes, facilitating simultaneous implementation of endovascular repair interventions [7].
Conclusion
Patients undergoing posterior spine surgery are at risk of vascular complications due to proximity to major vessels. Surgeons should be aware of these complications. Consideration should be given to the possibility of vascular injury if postoperative signs include abdominal pain, hypotension, tachycardia, and reduced hemoglobin levels. These injuries bear high mortality rates and necessitate urgent surgical intervention. Endovascular approaches are safe, less invasive, and demonstrate good efficacy in managing such complications.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
Patient consent had been obtained.
Article Info
Article Type
Case ReportPublication history
Received: Fri 22, Dec 2023Accepted: Mon 05, Feb 2024
Published: Wed 28, Feb 2024
Copyright
© 2023 Matthys Madalina. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2024.01.02
Author Info
Matthys Madalina Hafez K. Tessely H. Copin A. Bhogal H. Arend P.
Corresponding Author
Matthys MadalinaDepartment of Vascular Surgery, EpiCURA Hospital, Baudour, Belgium
Figures & Tables



References
1. Liu B, Ye K, Gao S,
Liu K, Feng H et al. (2019) The summary of experience of abdominal vascular
injury related to posterior lumbar surgery. Int Orthop 43: 2191-2198. [Crossref]
2. Papadoulas S,
Konstantinou D, Kourea HP, Kritikos N, Haftouras N et al. (2002) Vascular
injury complicating lumbar disc surgery. A systematic review. Eur J Vasc
Endovasc Surg 24: 189-195. [Crossref]
3. Mehdorn AS, Mehdorn
M, Mehdorn HM (2023) Vascular Injury During Lumbar Disc Surgery: Case Report. Acta
Neurochir Suppl 130: 185-189. [Crossref]
4. Akhaddar A, Alaoui
M, Turgut M, Hall W (2021) Iatrogenic vascular laceration during posterior
lumbar disc surgery: a literature review. Neurosurg Rev 44: 821-842. [Crossref]
5. Goel A, Kumar P,
Bahadur R (2019) Abdominal Vascular Injury During Posterior Lumbar Discectomy,
Experience from Three Cases and Review of Literature. Spine (Phila Pa 1976)
44: E1227-E1230. [Crossref]
6. Inamasu J, Guiot BH
(2006) Vascular injury and complication in neurosurgical spine surgery. Acta
Neurochir (Wien) 148: 375-387. [Crossref]
7. van Zitteren M, Fan
B, Lohle PN, de Nie JC, de Waal Malefijt J et al. A shift toward endovascular
repair for vascular complications in lumbar disc surgery during the last
decade. Ann Vasc Surg 27: 810-819. [Crossref]
8. Canaud L, Hireche
K, Joyeux F, D’Annoville T, Berthet JP et al. (2011) Endovascular repair of
aorto-iliac artery injuries after lumbar-spine surgery. Eur J Vasc Endovasc
Surg 42: 167-171. [Crossref]
9. Ganesan C, Petrus L, Ross IB (2012) Regarding the possibility of anterior vascular injury from the posterior approach to the lumbar disc space: an anatomical study. Spine (Phila Pa 1976) 37: E1371-E1375. [Crossref]
10. Kwinta BM, Myszka AM, Bigaj MM, Dragan MR, Kenig J et al. (2020) Iatrogenic Common Iliac Vessel Injury During Routine Degenerative Lumbar Spine Surgery: Report of 2 Cases and Review of Literature. World Neurosurg 137: 111-118. [Crossref]
