Journals
Carotid Artery Stenosis in Patients Treated for Head and Neck Cancer: A Community Based Retrospective Analysis
A B S T R A C T
Purpose
Radiotherapy treatment to the head and neck region is associated with a higher risk of developing carotid artery stenosis (CAS). This increases the patient’s risk for future cerebral vascular events such as stroke or transient ischemic attacks. We performed a community based observational retrospective study of CAS in patients who received surgical and/or radiation therapy treatment for head and neck malignancies.
Methods and Material
This study is a retrospective two-site institutional study. Data from 170 patients were obtained from Sacred Heart Hospital and Holy Family Hospital in Spokane, WA, USA between 2004 and 2007. A Fisher’s exact test was used to determine the prevalence of post-treatment CAS in patients who received radiotherapy and those who received surgery alone.
Results
One hundred and seventy patients met the inclusion criteria for this study. Thirty patients received surgery alone, 80 patients received radiation alone, and 60 received radiation plus surgery. Patients who received radiation therapy (radiation alone and radiation plus surgery groups) had a rate of any CAS of 17.9%, while those who received surgery alone had a rate of 13.3% (P = 0.789). Comparing patients who received radiation therapy to those who received surgery alone revealed rates of clinically significant CAS of 14.2% and 10.0%, respectively (P = 0.770). There were seven cases of severe CAS, all occurring in patients who received radiation.
Conclusions
Our study revealed nominally higher rates of CAS in patients who received radiotherapy for head and neck cancer. CAS is associated with an increased risk of harmful cerebrovascular events such as stroke and transient ischemic attack. A “gold standard” screening algorithm and management protocol has not yet been established for these patients. Thus, more research is needed to establish a “gold standard” screening algorithm for asymptomatic CAS in head and neck cancer survivors who have received therapeutic radiotherapy treatment.
K E Y W O R D S
carotid artery stenosis, radiation therapy, head and neck cancer
I N T R O D U C T I O N
Radiation therapy is often an important component of treatment for head and neck malignancies with the goals of increasing overall survival and reducing the risk of future local and distant disease recurrence. However, radiation therapy to the head and neck can be associated with an increased risk of atherosclerotic plaque development and an elevated risk of carotid artery stenosis (CAS). This places patients at risk of experiencing harmful cerebral events such as stroke and transient ischemic attack (TIA), resulting in significant mortality, morbidity, and loss of quality-adjusted life years (QALYs) [1]. CAS is of particular concern as it often remains clinically silent until severe stenosis is reached, at which point the risk of debilitating cerebrovascular event occurrence is relatively high [1]. It is therefore important to better understand the link between radiotherapy to the head and neck and CAS so that future studies can evaluate screening protocol and optimize how to manage these late toxicities.
The pathogenesis of radiation-induced atherosclerosis has yet to be definitively elucidated; however, according to Cheng, et al., the process is characterized by “…direct vessel wall damage, with intimal proliferation followed by necrosis of the media, periadventitial fibrosis, and accelerated atherosclerosis from intimal thickening and medial hyperplasia” [2].
Due to a lack of clear published consensus, there is not a currently established “gold standard” algorithm for screening and subsequent management of CAS in patients who have received head and neck radiotherapy. Our study aim was to evaluate our institutional risk of CAS in patients who were treated with radiotherapy for head and neck malignancies, and to further utilize this information to help establish new local screening and management guidelines for radiation-induced CAS in our community. Through this analysis, we were interested in generating further hypotheses regarding incidence risk and associations with patient pre-treatment characteristics.
Methods
Our study is a retrospective two-site institutional study of 170 patients from Sacred Heart Medical Center and Holy Family Hospital in Spokane, WA, USA. Data were obtained from a central institutional cancer database between 2004 and 2007. IRB approval was obtained. Inclusion criteria consisted of patients with malignancies of the lip, oral cavity, parotid glands, major salivary glands, tonsils, oropharynx, nasopharynx, pharynx, nasal cavity, sinus, glottis, supraglottis, sub-glottis, and larynx. Patients were excluded if they received chemotherapy alone, or no treatment. Histological cancer type was not taken into account in this study, although it was recognized that most patients had squamous cell carcinoma.
Patients were divided into three separate groups according to treatment received: surgery alone, radiation alone, and radiation plus surgery. The median follow-up time for patients in the study was 74 months. The diagnosis of CAS was based on information available in the medical record. For the purposes of our study, clinically significant stenosis was defined as ≥50% stenosis by either ultrasound (US) or computed tomography (CT). Cases of CAS were considered severe if the medical records indicated stenosis of >70% or if described as “high-grade” or “severe” by either US or CT.
The prevalence of post-treatment CAS across the three treatment groups were compared. The difference in prevalence of CAS between patients who received radiotherapy and those who received surgery alone were compared with a Fisher’s exact test.
Figure 1: Observed carotid artery stenosis in patients who received surgery only
Figure 2: Observed carotid artery stenosis in patients who received radiation only
Figure 3: Observed carotid artery stenosis in patients who received radiation plus surgery
Tables
Table 1: Observed carotid artery stenosis in different treatment modalities
|
|
#of Patients |
# with CAS |
#with Significant CAS |
# with Severe CAS |
|
Surgery Alone |
30 |
4 |
3 |
0 |
|
Radiation Alone |
80 |
16 |
15 |
6 |
|
Radiation Plus Surgery |
60 |
9 |
5 |
1 |
Results
A total of 170 patients met the inclusion criteria for the study. The prevalence of carotid artery stenosis in each patient group is shown in Table 1. Of the 170 patients, 30 patients received surgery alone, 80 patients received radiation alone, and 60 received radiation plus surgery.
Of the 30 patients that received surgery alone, four patients (13.3%) were diagnosed with CAS. Three of these patients (10.0%) were diagnosed with significant CAS, and zero had severe CAS. These results can be seen in Figure 1.
Diagnoses of CAS in the radiation alone group are shown in Figure 2. Sixteen of the 80 patients (20.0%) were diagnosed with CAS. Fifteen of these 16 patients (18.8%) were diagnosed with significant CAS, and six (7.5%) were diagnosed with severe CAS.
As seen in Figure 3, of the 60 patients that received radiation plus surgery, nine patients (15.0%) were diagnosed with CAS, of which five patients (8.3%) were diagnosed with significant CAS, and one patient (1.7%) was diagnosed with severe CAS.
Patients that received radiation therapy (surgery plus radiotherapy and radiotherapy alone groups) had a rate of CAS of 17.9%, while the surgery alone group had a rate of CAS of 13.3% (P = 0.789).
Clinically significant CAS was found at a rate of 14.2% in the groups that received radiotherapy, compared to 10.0% for the surgery alone group (P = 0.770). Additionally, all seven cases of severe CAS were seen in patients who had received radiotherapy.
Discussion
A standard screening and management protocol in the United States for CAS in patients with head and neck malignancies treated with radiotherapy has yet to be established due to a lack of available published level 1 evidence on this subject. The goal of this study was to provide hypothesis-generating preliminary data which could lead to future, more rigorous studies. This retrospective study attempts to further establish the relationship between major head and neck cancer treatment modalities and CAS incidence such that future studies may investigate best screening practices and help to establish standardized screening and management guidelines for CAS in patients following treatment.
Our data shows that radiotherapy to the head and neck is associated with a statistically insignificant higher prevalence of all stages of CAS. In support of these findings, a study by Yang and Wang of 71 patients who received head and neck radiotherapy revealed that all 71 patients had detectable CAS [3]. Additionally, a 62 patients case control study by Anzidei, et al. found that there was a statistically significant increase in carotid artery plaque volume (P = 0.001), fatty plaques (P = 0.001), and mixed plaques (P = 0.034) in the group that received head and neck radiotherapy [4]. A study by Lam, et al. compared 71 patients who received head and neck radiotherapy for nasopharyngeal carcinoma to 51 newly-diagnosed nasopharyngeal carcinoma patients prior to receiving radiotherapy. The researchers found no difference in atherosclerotic risk factors between the two groups, but that cases of arterial stenosis involving the common, internal, or external carotid arteries were more common in the radiotherapy group than in the newly-diagnosed group (P < 0.01) [5]. In a systematic review with meta-analysis of eight studies including 1,070 patients by Bashar, et al., it was found that the pooled risk ratio for overall stenosis rate in patients who received radiotherapy to the head and neck was 4.38 (95% CI, 2.98 – 6.45, P = 0.0001) [6]. The researchers also found that the incidence of both mild and severe stenosis were higher in the radiotherapy group (pooled RR 2.74 [95% CI, 1.75 – 4.30], P = 0.0001 and pooled RR 7.51 [95% CI, 2.75 – 20.32], P < 0.0001, respectively) [6].
It is known that CAS increases risk for the occurrence of cerebrovascular events, including hypo-perfusion, plaque embolus and thrombus formation. A systematic review of 34 published articles by Gujral, et al. showed that the relative risk of stroke in patients who received radiation therapy to the neck versus those that had not was 5.6 [7]. In a cross-sectional study by Cheng, et al., two-thirds of patients with radiotherapy-induced CAS of 70% or greater had either a stroke or TIA [8]. It is therefore of importance to generate standardized screening and management guidelines for post-radiotherapy CAS. Currently, there is a lack of evidence regarding the effectiveness of screening for radiation-induced CAS. This is a topic requiring further study.
It should be noted that all cases of severe stenosis in the current study occurred in patients who received radiotherapy as a component of treatment. We acknowledge that our study has many limitations due to the limited sample size and retrospective nature. We could not demonstrate a statistically significant difference between groups because of the small number of events. Selection bias is also a possibility in this study, as patients who received radiation therapy may have had more advanced disease. Additionally, patients treated with radiation-alone may have had co-morbidities that precluded surgical treatment that may be associated with a higher baseline risk of CAS. Demographic data such as age, sex, and race were not captured in this study, nor were disease characteristics such as tumor grade and stage.
The incidence rates of oropharyngeal cancer are rising in younger populations due to an increase in HPV-related cancers [9, 10]. Due to patients being diagnosed with these cancers at a young age, longer follow-up and lifelong screening protocols and guidelines will be needed. Long-term management of young patients with CAS is likely to present challenges, and a better understanding of the pathogenesis of radiotherapy-induced CAS may help guide therapies to improve long-term outcomes and quality of life. The current study highlights that CAS is common after treatment for head and neck cancer, and the role of screening may need further clarification by future studies in this patient population.
Conclusion
CAS is a commonly reported long-term side effect seen in patients treated for head and neck malignancies. Although our study did not reveal a statistically significant difference in CAS between patients treated with radiotherapy and patients treated with surgery alone, a correlation between clinically significant CAS and radiotherapy has been demonstrated in other studies. CAS increases the risk of harmful cerebrovascular sequelae. Due to the lack of standardized and reported clinical data, a standardized screening algorithm and subsequent management protocol in the United States has not yet been established for these patients. We feel that this study provides additional insights into the need for more rigorous future studies on this subject. Lowering the risk of post-treatment cerebrovascular events for these patients is a significant need and will lead to overall improvement in quality of life. More research is needed to determine best practices for screening and treatment algorithms of asymptomatic radiotherapy-induced CAS in head and neck cancer survivors.
Acknowledgements
We would like to acknowledge Shelley Berdar RN/BSN and the Providence Tumor Registry Team for their support and assistance with this research project.
Funding
This work was funded in part by the Community Cancer Fund, Spokane, WA.
No authors of this paper have any financial disclosures to make.
All authors listed contributed to the design and implementation of the research, to the analysis of results, and to the writing of this manuscript.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 27, Apr 2018Accepted: Mon 07, May 2018
Published: Tue 22, May 2018
Copyright
© 2023 Jason Call. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2018.10.012
Author Info
Aaron E Wagner John S Goodman Brian J Mitchell Christopher M Lee Howard R Sanders Jason Call Jeffrey D Bunn Robert K Fairbanks Ryan Nachreiner Wayne T Lamoreaux
Corresponding Author
Jason CallAlaska Cancer Treatment Center, Anchorage, AK, USA
Figures & Tables
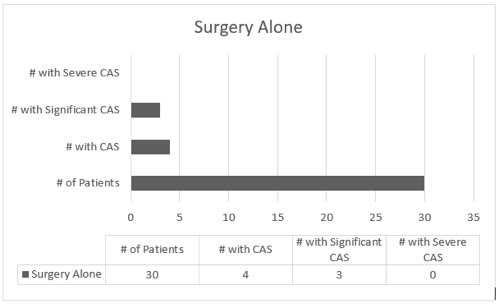
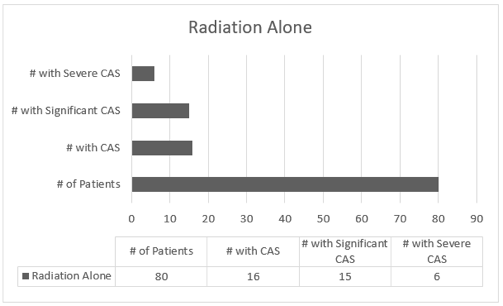
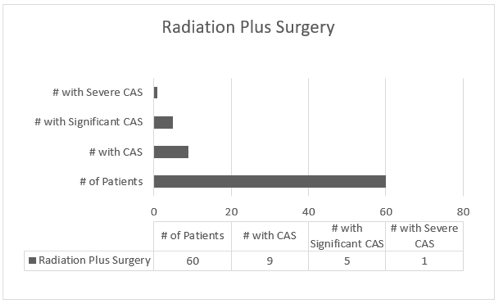
Table 1: Observed carotid artery stenosis in different treatment modalities
|
|
#of Patients |
# with CAS |
#with Significant CAS |
# with Severe CAS |
|
Surgery Alone |
30 |
4 |
3 |
0 |
|
Radiation Alone |
80 |
16 |
15 |
6 |
|
Radiation Plus Surgery |
60 |
9 |
5 |
1 |
References
1. Gujral DM, Shah BN, Chahal NS, Senior R, Harrington KJ, et al. (2014) Clinical features of radiation-induced carotid atherosclerosis. Clin Oncol (R Coll Radiol) 26: 94-102. [Crossref]
2. Cheng SW, Ting AC, Wu LL (2002) Ultrasonic analysis of plaque characteristics and intimal-medial thickness in radiation-induced atherosclerotic carotid arteries. Eur J Vasc Endovasc Surg 24: 499-504. [Crossref]
3. Yang Y, Wang T (2016) Radiotherapy of the neck and carotid stenosis. J Biol Regul Homeost Agents 30: 795-799. [Crossref]
4. Anzidei M, Suri JS, Saba L, Sanfilippo R, Laddeo G, et al. (2016) Longitudinal assessment of carotid atherosclerosis after Radiation Therapy using Computed Tomography: A case control Study. Eur Radiol 26:72-78. [Crossref]
5. Lam WW, Leung SF, So NM, Wong KS, Liu KH, et al. (2001) Incidence of carotid stenosis in nasopharyngeal carcinoma patients after radiotherapy. Cancer 92: 2357-2363. [Crossref]
6. Bashar K, Healy D, Clarke-Moloney M, Burke P, Kavanagh E, et al. (2014) Effects of neck radiation therapy on extra-cranial carotid arteries atherosclerosis disease prevalence: systematic review and a meta-analysis. PLoS One 9: 110389. [Crossref]
7. Gujral DM, Chahal N, Senior R, Harrington KJ, Nutting CM (2014) Radiation-induced carotid artery atherosclerosis. Radiother Oncol 110: 31-38. [Crossref]
8. Cheng SW, Ting AC, Lam LK, Wei WI (2000) Carotid stenosis after radiotherapy for nasopharyngeal carcinoma. Arch Otolaryngol Head Neck Surg 126: 517-521. [Crossref]
9. Laprise C, Madathil SA, Schlecht NF, Castonguay G, Soulières D, et al. (2017) Human papillomavirus genotypes and risk of head and neck cancers: Results from the HeNCe Life case-control study. Oral Oncol 69: 56-61. [Crossref]
10. Tota JE, Anderson WF, Coffey C, Califano J, Cozen W, et al. (2017) Rising incidence of oral tongue cancer among white men and women in the United States, 1973-2012. Oral Oncol 67: 146-152. [Crossref]
