Brown Tumor Secondary to Hyperparathyroidism: A Case Report
A B S T R A C T
Brown Tumors are rare benign tumors that are considered to be the end manifestation of hyperparathyroidism. They can be clinically identified as localized palpable masses in any part of the skeleton. Radiological features vary according to the extent of hyperparathyroidism. In this case report, we present a 24-year-old male on haemodialysis for end stage renal disease, with brown tumor of the mandible and maxillary alveolus as a consequence of longstanding secondary hyperparathyroidism.
Keywords
Brown tumor, hyperparathyroidism, ESRD, parathyroidectomy
Introduction
Brown Tumors are rare benign reactive tumors. They are considered the end manifestation of hyperparathyroidism. Diagnosis can be difficult sometimes, but not impossible. Medical and surgical treatment can help in resolving it.
Case Report
24 years old male, presented to the clinic with features of brown tumor. Known to have hypertension, chronic renal disease on dialysis for 8 years, and hyperparathyroidism. Patient was on cinacalcet, his PTH level improved for a while, but then increased, hence was referred to our clinic. Investigations for his condition was proceeded, PTH was high around 190 pmol/L, US of the neck to look for parathyroid gland was done, didn’t show any parathyroid masses, so scintigraphy and CT of the head, neck and chest was done.
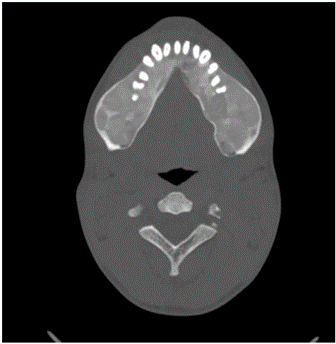
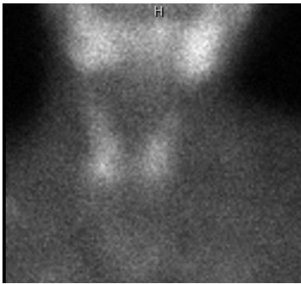
CT scan showed an expansion of the bone seen especially in the mandible and maxillary alveolus with multiple lucencies throughout the skeleton; these bony changes suggestive of brown tumor (Figure 1), no parathyroid mass, and no ectopic parathyroid gland were seen. Scintigraphy showed right lower lobe of the thyroid uptake, probable of right inferior parathyroid adenoma, no ectopic uptake (Figure 2). Patient was taken for parathyroidectomy after doing nuclear medicine parathyroid injection, the left superior and inferior parathyroid glands were removed, same thing in the right side and pieces of both sides were sent for frozen pathology, remaining of the right gland was re transplanted in the sternocleidomastoid muscle. PTH level was sent after 15 min of the removal.
Gamaprobe was used to check for nuclear uptake, the readings were in the left side more than 500 both in the superior and inferior glands area, and the readings for the right side were 1000. Pathologist called reporting that right side superior parathyroid tissue is an enlarged parathyroid glands, the right inferior parathyroid tissue is just lymph node. Left side inferior parathyroid tissue is a piece of thymus without malignancy, and the superior part is a parathyroid gland.
Figure 1: Lesions in the mandible, features of brown tumor.
Figure 2: Scintigraphy, showing right inferior thyroid uptake.
Since the parathyroid adenoma was not yet found, dissection was continued until the mediastinum, stripping down the nerve without injuring it, and 2 more structures were seen in the right and left inferior part, were taken for frozen pathology. PTH level didn’t decrease much as well. Since nothing else was found, wound was closed, decision was made to re image the patient. CT scan and scintigraphy test were done 2 days after the surgery, which showed possible presence of parathyroid adenoma in the region of the lower pole of the right thyroid lobe. The result was discussed with the patient but unfortunately decided not to do any more procedures and got discharged.
Discussion
Hyperparathyroidism is classified into three prominent entities; primary, secondary, and tertiary hyperparathyroidism. Primary hyperparathyroidism has increased parathyroid hormone (PTH) levels along with high calcium and low phosphate levels, usually secondary to parathyroid adenoma, parathyroid hyperplasia or parathyroid carcinoma, which is considered the third most common endocrine disorders and occurs mostly in post-menopausal women [1]. Secondary hyperparathyroidism has high PTH levels along with low calcium and high phosphate levels, usually due to chronic kidney disease or vitamin D deficiency. Lastly, tertiary hyperparathyroidism has high PTH along with high calcium and high phosphate levels and this usually manifests itself in the setting of long standing secondary hyperparathyroidism [2].
Brown tumors, also known as osteitis fibrosa cystica, are considered rare benign reactive tumors with prevalence of about 4.5% in primary hyperparathyroidism and 1.5-1.7% in secondary hyperparathyroidism [3]. It gets the name “brown tumor” because of its high vascularity, hemorrhage, and haemosiderin deposition giving it the brownish red colour [4]. Brown tumors are considered to be the end stage manifestation of hyperparathyroidism in the bones and rarely are the initial sign of hyperparathyroidism [5]. They form by the imbalance between osteoclastic and osteoblastic activity in the bone leading to fibrous replacement of the parenchyma [6]. They have three stage of development; in the first stage osteoclasts resorb bone due to the effect of high PTH with subsequent formation of collagen fibers in the bone marrow. The second stage, also called the fibrotic osteitis stage, signifying the resorption of the trabecular bone with replacement of the bone marrow with fibrosis, haemosiderin-laden macrophage, hemorrhage, microfracture, and reactive woven bone formation. In the final stage, known as fibrous cystic osteitis, cystic degeneration occurs secondary to the ongoing effect of hyperparathyroidism and hemorrhage [7].
Clinically, brown tumors manifest themselves as localized palpable, tender, and hard masses usually in the mandible, sternum, ribs, pelvis, and long bones [8]. Additionally, patients usually complain of other symptoms secondary to hypercalcemia; like abdominal pain, nausea, vomiting, constipation, renal stones, and fatigue [9]. Radiological manifestation varies according to the extent of the hyperparathyroidism; nonetheless, they are typically well-circumscribed monolocular or multilocular lytic masses with either sclerotic margins at the periphery or infiltration into surrounding soft tissue with cortical damage [4, 9]. Diagnosis can be difficult sometimes as radiologically it can mimic metastatic lesions or primary tumors like giant cell tumors, hence to differentiate between them, the diagnosis is made based on the laboratory findings with calcium, phosphate, parathyroid hormone level, alkaline phosphatase; histologic results; and radiological results all together [9, 10]. Treatment is mainly aimed at resolving the primary problem, which is the hyperparathyroidism. Since parathyroid adenoma is one of the most common etiologies for brown tumors, surgery to remove the adenoma can result in almost complete remission with remineralization of the lytic bone portions [11]. Nonetheless, for large disfiguring lesions surgical excision of the brown tumor alone may be indicated [6].
In hyperparathyroidism, the mainstay of the treatment is aiming to control the calcium level [12]. However, in cases of primary and tertiary hyperparathyroidism, surgical management is first line therapy which is achieved by performing a parathyroidectomy [13]. Parathyroid adenoma localization can be done by several ways; invasive and non-invasive methods. Non-invasive methods consist of imaging studies like: ultrasonography, CT, MRI, or scintigraphy using technetium (Tc-99m) sestamibi [14]. Scintigraphy has a high sensitivity reaching around 80% in localizing a single adenoma, however this sensitivity drops to 25% when there are multiple adenomas [15]. Surgical management of parathyroid adenoma is by surgical exploration of the neck with subsequent removal of the adenoma, biopsy of another parathyroid gland is indicated if another adenoma or multiple gland hyperplasia is suspected [15]. There are several ways to check if the adenoma is successfully removed during and after the surgery. Intraoperatively a rapid PTH assay can be used and post-operatively a calcium and PTH levels can be checked which would show a downward trend if the pathological gland was removed [14].
Some studies hypothesize that post-Para thyroidectomy of the adenoma; the PTH will not go back to normal due to the desensitization of the PTH receptors or post-receptor level. This leads to a higher than normal level of PTH to maintain normal calcium level and function appropriately. This idea is supported by the fact that patients with bigger tumors and higher PTH levels pre-operatively have higher PTH levels post-operatively when compared with their lesser counterparts [16]. Others hypothesize that the remaining glands undergo hyperplasia as a compensatory mechanism leading to a high PTH in the follow up period and a subsequent high calcium level; presenting as recurrent hyperparathyroidism [17]. Hence regular follow up after the surgical treatment is needed. Some researches emphasized that even the bone involvement like brown tumor, will regress over time after the surgical treatment, nevertheless some other studies are showing the opposite [18].
Conclusion
Brown tumor is a rare complication of hyperparathyroidism. Diagnosis can be challenging as it can mimic other diagnosis; nevertheless, it can be treated once it is diagnosed and surgically removed. Follow up is indicated to check for recurrence and removal of the corrected parathyroid gland.
Article Info
Article Type
Case ReportPublication history
Received: Mon 24, Apr 2023Accepted: Tue 09, May 2023
Published: Fri 19, May 2023
Copyright
© 2023 Alharmoodi F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.02.03
Author Info
Alharmoodi F Alsheryani M Alhajeri L Alshaikh M Aby Ali H Alfelasi M
Corresponding Author
Alharmoodi FDepartment of General Surgery, Tawam Hospital, Alain, United Arab Emirates
Figures & Tables
References
1. Fraser WD (2009)
Hyperparathyroidism. Lancet 374: 145-158. [Crossref]
2. Xu B, Yu J, Lu Y,
Han B (2020) Primary hyperparathyroidism presenting as a brown tumor in the
mandible: a case report. BMC Endocr Disord 20: 6. [Crossref]
3. Lessa MM, Sakae FA,
Tsuji RK, Filho BCA, Voegels RL et al. (2005) Brown tumor of the facial bones:
case report and literature review. Ear Nose Throat J 84: 432-434. [Crossref]
4. Nair PP, Gharote
HP, Thomas S, Guruprasad R, Singh N (2011) Brown tumour of the jaw. BMJ Case
Rep 2011: bcr0720114465. [Crossref]
5. Alhusban M, Baqain
ZH (2011) Mandibular brown tumor as the first manifestation of primary
hyperparathyroidism: A case report. Saudi Dent J 23: 107-109. [Crossref]
6. Suarez Cunqueiro
MM, Schoen R, Kersten A, Klisch J, Schmelzeisen R (2004) Brown tumor of the
mandible as first manifestation of atypical parathyroid adenoma. J Oral
Maxillofacl Surg 62: 1024-1028. [Crossref]
7. Xu W, Qu Y, Shi W,
Ma B, Jiang H et al. (2019) Multiple bone brown tumor secondary to primary
hyperparathyroidism: a case report and literature review. Gland Surg 8:
810-816. [Crossref]
8. Toescu SM, Ibrahim
M, O'Donovan DG, Balasubramaniam G, David KM (2019) Complex spinal fixation of
a cervical vertebra Brown tumour: report of an unusual case. Br J Neurosurg
33: 684-686. [Crossref]
9. Zou H, Song L, Jia
M, Wang L, Sun Y (2018) Brown tumor of multiple facial bones associated with
primary hyperparathyroidism: A clinical case report. Medicine (Baltimore)
97: e11877. [Crossref]
10. Choi JH, Kim KJ,
Lee YJ, Kim SH, Kim SG et al. (2015) Primary Hyperparathyroidism with Extensive
Brown Tumors and Multiple Fractures in a 20-Year-Old Woman. Endocrinol Metab
(Seoul) 30: 614-619. [Crossref]
11. Hu J, He S, Yang J,
Ye C, Yang X et al. (2019) Management of brown tumor of spine with primary
hyperparathyroidism: A case report and literature review. Medicine
(Baltimore) 98: e15007. [Crossref]
12. Selvi F, Cakarer S,
Tanakol R, Guler SD, Keskin C (2009) Brown tumour of the maxilla and mandible:
a rare complication of tertiary hyperparathyroidism. Dentomaxillofac Radiol
38: 53-58. [Crossref]
13. Triantafillidou K,
Zouloumis L, Karakinaris G, Kalimeras E, Iordanidis F (2006) Brown tumors of
the jaws associated with primary or secondary hyperparathyroidism. A clinical
study and review of the literature. Am J Otolaryngol 27: 281-286. [Crossref]
14. Williams BA, Trites
JRB, Taylor SM, Bullock MJ, Hart RD (2014) Surgical management of primary
hyperparathyroidism in Canada. J Otolaryngol Head Neck Surg 43: 44. [Crossref]
15. Prihantono P,
Palinggi E, Haryasena H, Hamdani W, Binekada IMC (2019) Surgical Treatment for
Parathyroid Adenoma: A Case Report. Open Access Maced J Med Sci 7:
2497-2501. [Crossref]
16. Sagiv R, Delgado B,
Sadeh R, Shasha, S, Fraenkel,M et al. (2021) High parathyroid hormone levels
after parathyroidectomy for parathyroid adenoma are not related to the
cellularity of the remaining glands. Laryngoscope Investig Otolaryngol
6: 1220-1227. [Crossref]
17. Rose DM, Wood TF, Van Herle AJ, Cohan P, Singer FR et al. (2001) Long-term management and outcome of parathyroidectomy for sporadic primary multiple-gland disease. Arch Surg 136: 621-626. [Crossref]
18. Hon Ke Sia, Ming-Chia H, Li Heng Yang, Shih Te T (2012) Maxillary brown tumor as initial presentation of parathyroid adenoma: A case report. Kaohsiung J Med Sci 28: 400-403. [Crossref]
