Bowel Perforation Due to Complicated Jejunal Diverticulitis: A Rare Case Report and Literature Review
A B S T R A C T
Small bowel diverticulosis is a rare and acquired disease usually diagnosed as an incidental radiological finding. We report the case of a 65-year-old man admitted to our Emergency Department with abdominal pain and fever. The CT-scan showed multiple jejunal diverticular eversions and oedema of the surrounding tissues. At urgent laparotomy the radiological finding was confirmed with microperforation of one diverticula. Bowel resection was performed and histology revealed erosive inflammation with ischemic mucosa.
Small bowel diverticula do not require any treatment if asymptomatic, nevertheless cases like this could be life-threatening. Urgent surgical procedure must be the treatment of choice in these patients.
Keywords
Jejunal, small bowel diverticulitis, perforation
Introduction
Small intestinal diverticula represent a rare and acquired disease, generally affecting the elderly [1]. They are usually asymptomatic and diagnosed as an incidental radiologic finding. No treatment is required in these cases. Pathogenesis is characterized by abnormalities in either the smooth muscle or the myenteric plexus causing herniation of mucosa and submucosa through the muscular layer of the bowel wall. This differentiate them from true diverticula as Meckel’s, which are congenital and have all the bowel wall layers herniated. The site of origin is usually the small bowel mesenteric border. Diagnosis and management can be challenging since this condition could lead to potentially fatal complications as perforation requiring urgent surgical treatment [2, 3].
Case Presentation
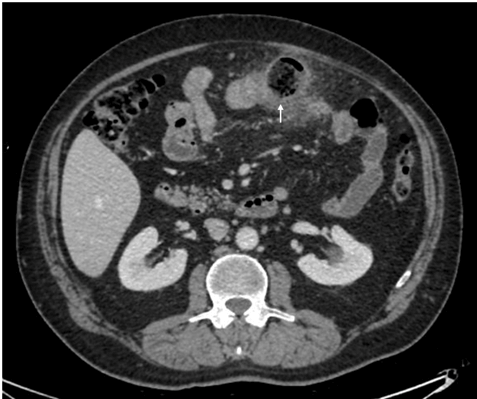
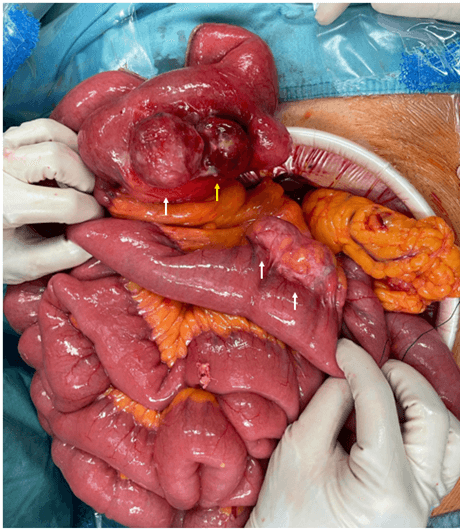
A 65-year-old man was admitted to our Emergency Department with abdominal pain and fever started four days before, in absence of other symptoms. The patient was stable, with normal heart rate (75 bpm) and blood pressure (130/80 mmHg). Abdomen was soft but tender between the epigastric and umbilical region. Laboratory findings on admission showed WBC 10.2×109/L, CRP 131 mg/L; other blood values were unremarkable. Abdominal CT scan (Figure 1) revealed two proximal jejunal diverticular eversions of 3 and 4 cm in maximum diameter, respectively. Oedema of the surrounding tissues and a localized fluid collection with an air bubble were also identified. Intraoperative findings at urgent laparotomy consist of a 70 cm-jejunal segment, about 100 cm far from the Treitz ligament, with inflamed loops. Four diverticula on the mesenteric border were observed. One of the extroflections had a microperforation that originated an abscess (Figure 2). The jejunal segment was resected and a mechanical latero-lateral anastomosis was performed to restore bowel continuity. The following hospital stay was uneventful with discharge on postoperative day 5. Histology showed an erosive inflammation with ischemic mucosa and an abscessualized area with a fistulous tract due to microperforation. At 1, 3 and 6 months follow-up the patient resulted in good conditions, in the absence of complications.
Figure 1: Axial CT-scan showing one of the jejunal diverticula, indicated by the arrow.
Figure 2: Intra-operative findings showing all four jejunal diverticula, indicated by arrows (the yellow one indicates the perforated diverticula).
Discussion
Small bowel diverticulosis is a very rare event, occurring in about 1% of the population, with a greater prevalence at the duodenal level followed by the jejunal-ileal district [4]. First described by Sömmering and Baille in 1794, these are false diverticula, or pseudodiverticula, thus involving the mucosa and submucosa herniating through the muscular layer of the intestinal wall [5]. Such diverticula are acquired, generally affecting adults over 60 years of age and males [6, 7]. Usually asymptomatic, they are often autopsy or imaging occasional findings. They require no treatment in such cases. However, they can generally manifest with abdominal pain in diverticulitis. Medical therapy based on fasting, fluid therapy and broad-spectrum antibiotics is often sufficient to regress symptoms in these cases. On the other hand, in case of complications as intestinal perforation, bleeding or even obstruction, surgical treatment is recommended with bowel resection and direct restoration of intestinal continuity.
Bowel perforation is one of the most feared complications as it can lead, if not treated promptly, to a rapid worsening of patient's prognosis with high mortality rates. Few cases of jejunal diverticulitis complicated by perforation have been described in literature, with clinical features ranging from more nuanced symptoms of chronic and nonspecific abdominal pain to acute abdomen [8-10]. The treatment of these dangerous scenarios requires a surgical approach. An interesting management algorithm proposed by Zi Qin Ng et al. classifies small bowel diverticulitis into uncomplicated, in which the proposed treatment is based on fasting and antibiotic therapy, and complicated, that can be associated with localized or diffuse peritonitis [11]. In the localized forms, a noninterventional first approach may be effective and surgery should be proposed only in case of clinical worsening. In case of diffuse peritonitis, instead, the first approach has to be surgical. A third, rarer group, represented by complications such as volvulus, intussusception or bowel occlusion, should be managed surgically, too.
Thus, early diagnosis, whereby the radiological gold standard is represented by CT-scan, remains crucial to identify the diverticulitis grade promptly and treat it straightforward, avoiding dangerous worsening of the patient's prognosis [12]. In our case, the clinical scenario led to a rapid radiological diagnosis and consequent surgery with jejunal resection and direct restoration of bowel continuity, a procedure that should be considered of choice in these patients.
Statements and Declarations
The corresponding author declares that he acts on behalf of all authors and that all authors have approved the submission.
Data Availability
Information was obtained consulting clinical records but are available from the corresponding author on reasonable request.
Conflicts of Interest
None.
Funding
None.
Consent
Informed consent was obtained from the patient.
Copyright and Permissions
No pictures or parts of text reproduced or copied from other publications (including publications by the authors) are included in the manuscript.
Ethical Considerations
The study was based on hospital data obtained consulting clinical records, therefore ethical disclosure was not necessary.
Acknowledgments
Not necessary.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 20, Feb 2023Accepted: Wed 08, Mar 2023
Published: Thu 16, Mar 2023
Copyright
© 2023 Mauro Giambusso. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.01.03
Author Info
Mauro Giambusso Paolo Mirco Marta Di Grezia Valentina Bianchi
Corresponding Author
Mauro GiambussoEmergency and Trauma Surgery Unit, A. Gemelli University Hospital Foundation and IRCCS, Rome, Italy
Figures & Tables
References
1. Bosanquet DC,
Williams N, Lewis MH (2010) Acquired small bowel diverticular disease: a
review. Br J Hosp Med 71: 552-555. [Crossref]
2. Rangan V, Lamont JT
(2020) Small Bowel Diverticulosis: Pathogenesis, Clinical Management, and New
Concepts. Curr Gastroenterol Rep 22: 4. [Crossref]
3. Wilcox RD, Shatney
CH (1988) Surgical implications of jejunal diverticula. South Med J 81:
1386-1391. [Crossref]
4. Akbari ME, Atqiaee
K, Lotfollahzadeh S, Moghadam ANJ, Sobhiyeh MR (2013) Perforated jejunal
diverticula- a rare cause of acute abdominal pain: a case report. Gastroenterol
Hepatol Bed Bench 6: 156-158. [Crossref]
5. Abdelhalim D, Kania
T, Heldreth A, Champion N, Mukherjee I (2022) Operative Management of
Perforated Jejunal Diverticulitis. Cureus 14: e21330. [Crossref]
6. de Bree E,
Grammatikakis J, Christodoulakis M, Tsiftsis D (1998) The clinical significance
of acquired jejunoileal diverticula. Am J Gastroenterol 93: 2523-2528. [Crossref]
7. Hardon SF, den Boer
FC, Aallali T, Fransen GA, Muller S (2021) Perforated jejunal diverticula in a
young woman: A case report. Int J Surg Case Rep 81:105838. [Crossref]
8. Gurala D, Idiculla
PS, Patibandla P, Philipose J, Krzyzak M et al. (2019) Perforated Jejunal
Diverticulitis. Case Rep Gastroenterol 13: 521-525. [Crossref]
9. Mejri A, Arfaoui K,
Hedfi M, Znaidi H (2022) Perforated jejunal diverticulum as an unsual cause of
acute abdomen: A case report. Int J Surg Case Rep 94: 107130. [Crossref]
10. Sarıtaş AG, Topal
U, Eray İC, Dalcı K, Akçamı AT et al. (2019) Jejunal diverticulosis complicated
with perforation: A rare acute abdomen etiology. Int J Surg Case Rep 63:
101-103. [Crossref]
11. Ng ZQ, Theophilus M, Navadgi S, Menon T, Wijesuriya R (2019) Jejunal Diverticulitis: A Single-Center Experience and Proposed Management Algorithm. Surg Infect (Larchmt) 20: 499-503. [Crossref]
12. Fintelmann F, Levine MS, Rubesin SE (2008) Jejunal diverticulosis: findings on CT in 28 patients. AJR Am J Roentgenol 190: 1286-1290. [Crossref]
